Short‑term impact of aged garlic extract on endothelial function in diabetes: A randomized, double‑blind, placebo‑controlled trial
- Authors:
- Published online on: December 27, 2019 https://doi.org/10.3892/etm.2019.8377
- Pages: 1485-1489
-
Copyright: © Hamal et al. This is an open access article distributed under the terms of Creative Commons Attribution License.
Abstract
Introduction
High arterial stiffness is known to be a risk factor, as well as a prognostic marker for cardiovascular disease (CVD) (1). Endothelial dysfunction plays a key role in arterial stiffness by reducing the endothelial properties of vasodilatation, accelerating the proinflammatory and prothrombotic properties (2). Endothelial dysfunction is an early event in patients with CVD and is considered as one of the several potential contributors to plaque destabilization (3).
A number of non-invasive techniques are available to assess the endothelial function and arterial stiffness of the peripheral vasculature, such as brachial artery flow-mediated vasodilatation (bFMD), pulse wave velocity (PWV) and cardio-ankle vascular index (CAVI) (4,5). These non-invasive methods were widely used clinically to predict the risk of subclinical atherosclerosis in individuals who are at a high risk of CVD (6). CAVI is an inexpensive, non-invasive, office-based method which is used to evaluate arterial stiffness in the aorta, femoral artery and tibial artery, which reflects the degree of cardiovascular disease (1,7). The advantage to CAVI is that it is not affected by blood pressure (BP) and the measurements are automatic via validated software (6,8,9).
Our group has demonstrated the cardioprotective effects of AGE by decreasing atherosclerotic plaque progression in patients with type 2 diabetes (10) and improving endothelial function (11,12). Endothelial dysfunction plays a critical role in the pathogenesis of micro- and macrovascular diseases in patients with type 2 diabetes (13). Annual screening is recommended for diabetic patients for the early detection of micro- and macrovascular complications. This study investigated the effects of AGE in individuals with type 2 diabetes on vascular elasticity and endothelial function, which was measured by CAVI, over a period of 3 months.
Patients and methods
Study population and randomization
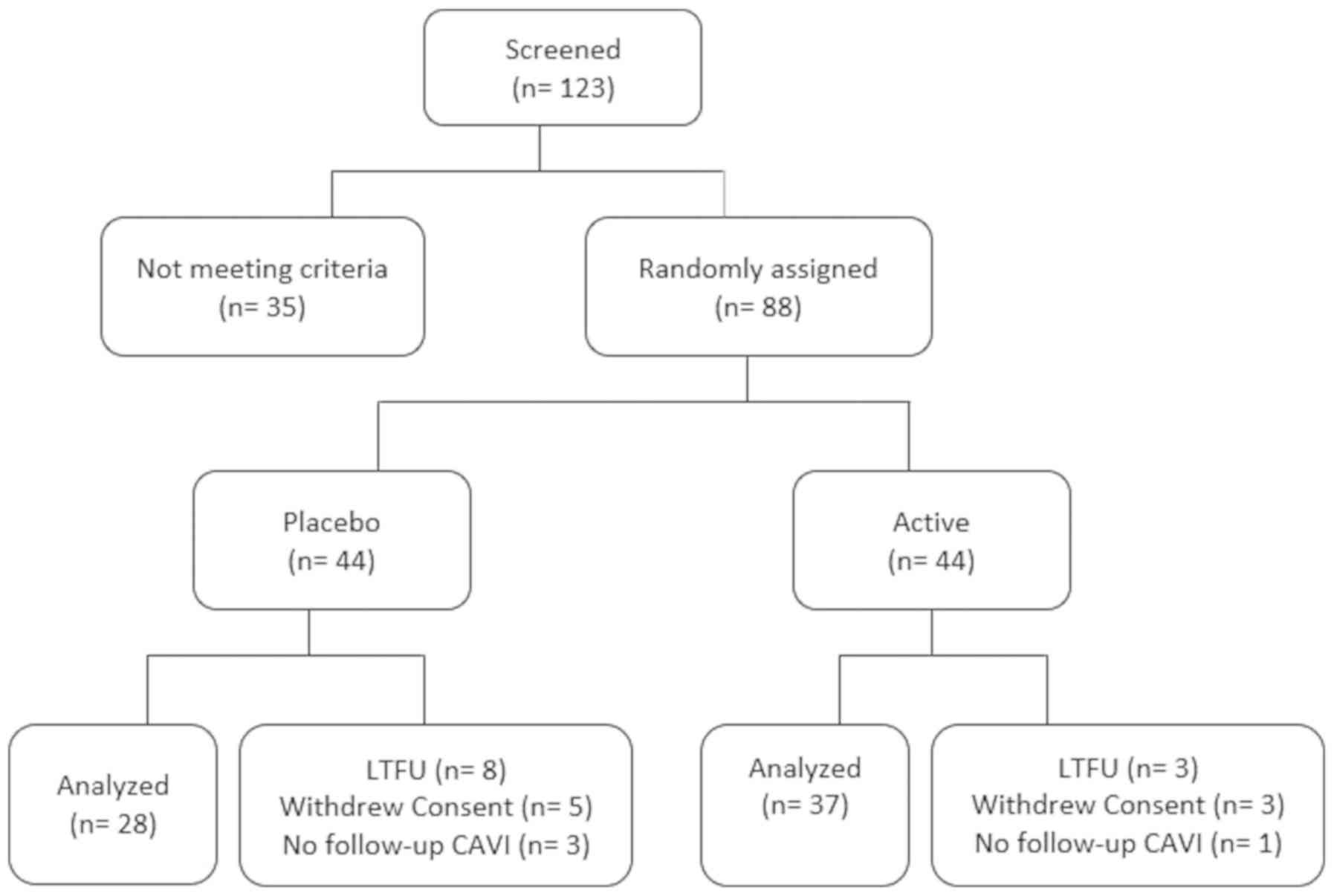
A total of 88 patients with type 2 diabetes were enrolled in a double-blind, placebo-controlled randomized study, who met the eligibility criteria (inclusion and exclusion criteria), after signing a written informed consent that was approved by the Institutional Review Board (IRB) of the Lundquist Institute for Biomedical Innovation at Harbor UCLA Medical Center (NCT03931434). Of these 88 patients, 23 patients were unable to undergo all follow-up visits (Fig. 1). Cardiovascular risk factors, and hemoglobin A1c (HbA1c) and serum lipid profiles were obtained using standard techniques at baseline. Participants were followed-up for 3 months with CAVI measured at baseline and again at 3 months.
Patients were randomized at a 1:1 ratio to receive AGE (active group) or the placebo. All participants were advised to take 2 capsules twice daily with water for 3 months. The 2,400 mg of AGE capsules were provided by Wakunaga of America Co., Ltd. with a matched placebo pill which looked similar to AGE, but did not contain any garlic or active ingredient. Both the active and placebo study drugs were similar in size and color. The study drug was packaged in the containers sent by the sponsor as per the randomization list and was sent to the site with a printed label containing only the number of the patient. The randomization key was provided to the principal investigator and was opened only after the completion of the study. We conducted an inter-trial phone visit to ensure study medication compliance. The AGE capsule used in this study is commercially available in the market.
Inclusion criteria
We enrolled patients between age 30–75 years with a known history of type 2 diabetes mellitus (HbA1c >6.5% or fasting blood sugar >125 mg/dl or taking antidiabetic medications) and who signed an informed consent form.
Exclusion criteria
We excluded patients with known hypersensitivity to AGE, a body weight in excess of 350 pounds, a history of coronary artery disease (CAD), myocardial infarction (MI), stroke or life-threatening arrhythmia within the prior 6 months, New York Heart Association Functional Classification II–IV heart failure, renal impairment (serum creatinine >1.4 mg/dl), current tobacco use, a history of bleeding disorders or use of anticoagulants, hypertensive encephalopathy or cerebrovascular accident, or who were currently enrolled in another placebo-controlled trial.
Measurement of CAVI
CAVI was measured using the VaSera (Fukuda Denshi non-invasive BP, pulse wave velocity (PWV) and heart sound monitor/measuring device that integrated the values to compute an ankle-brachial index (ABI) and a proxy of arterial stiffness (CAVI). Briefly, blood pressure cuffs were applied to the bilateral upper arms and ankles, with the subject lying in the supine position and the head held in midline position. Electrocardiographic electrodes were placed on both wrists and a microphone was placed on the sternal angle for phonocardiography. After resting for 10 min, the examinations were performed. To detect the brachial and ankle pulse waves with cuffs, a low cuff pressure from 30 to 50 mmHg was used to ensure minimal effect of cuff pressure on hemodynamics. Following automatic measurements, the obtained data were analyzed using VSS-10 software (Fukuda Denshi), and the values of the right and left CAVI were measured. The averages of the right and left CAVIs were used for analysis.
Statistical analysis
Continuous variables are expressed as the means ± SD, while categorical variables are stated as counts and percentages. A Student's t-test or Chi-square test was used to determine differences in all baseline parameters between the placebo and AGE group. An ANOVA model with treatment as the main effect was used to compare changes with CAVI from baseline to follow-up between the groups, while using Tukey's procedure for post hoc analysis and comparison of multiple groups. Pearson's correlation coefficient was used to analyze the strength of the correlation between the left and right CAVI measures at each visit. A P-value of <0.05 was considered to indicate a statistically significant difference. SAS software (version 9.4) was used to carry out all statistical analyses.
Results
A total of 65 patients (38 men and 27 women; mean age 58.45±11.25 years) completed 2 study visits (baseline and 3 months), where baseline and follow-up CAVI measures were assessed (Fig. 1). Out of the 65 patients, 37 were randomized to the treatment (AGE; active) group (19 males; mean age, 59.3±10.8 years). Patients current medications, such as aspirin, hypertensive or hyperlipidemia or diabetic medications, did not change during the 3 months of the study. The baseline characteristics of the patients have been published elsewhere (14).
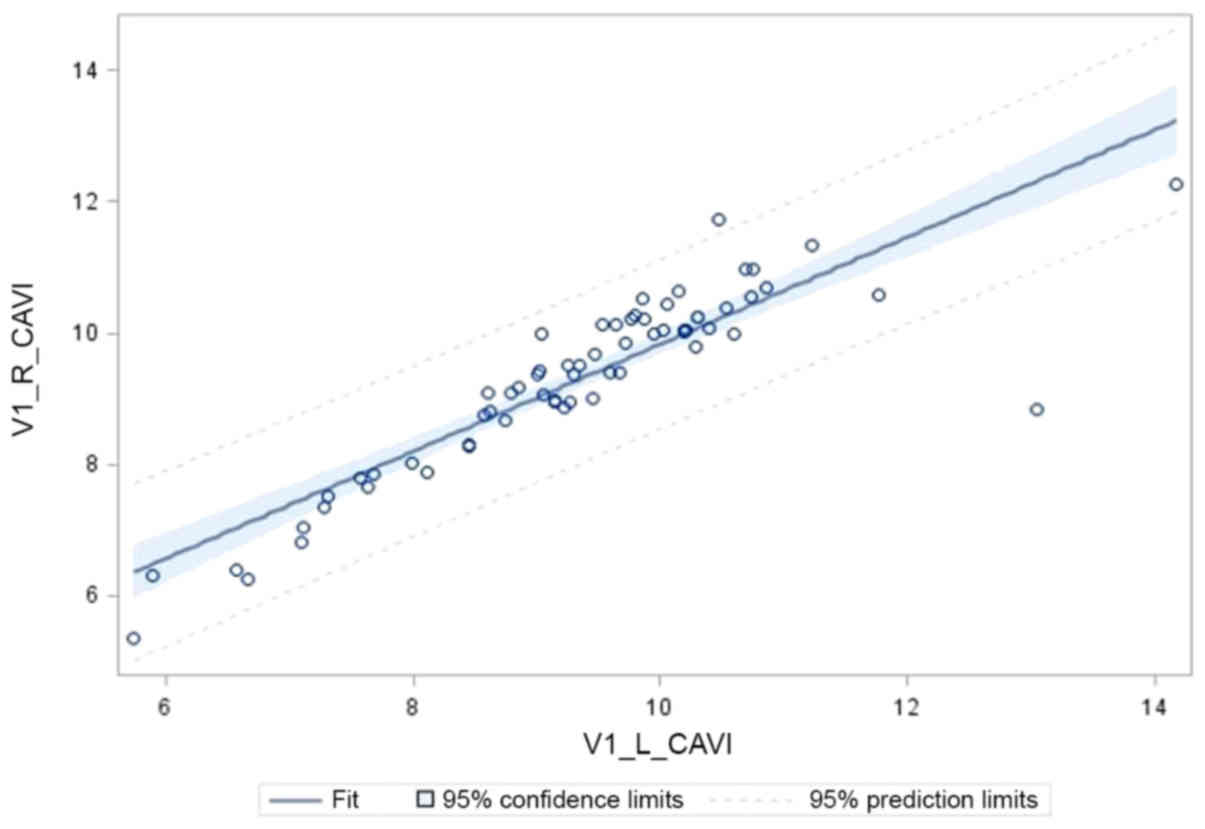
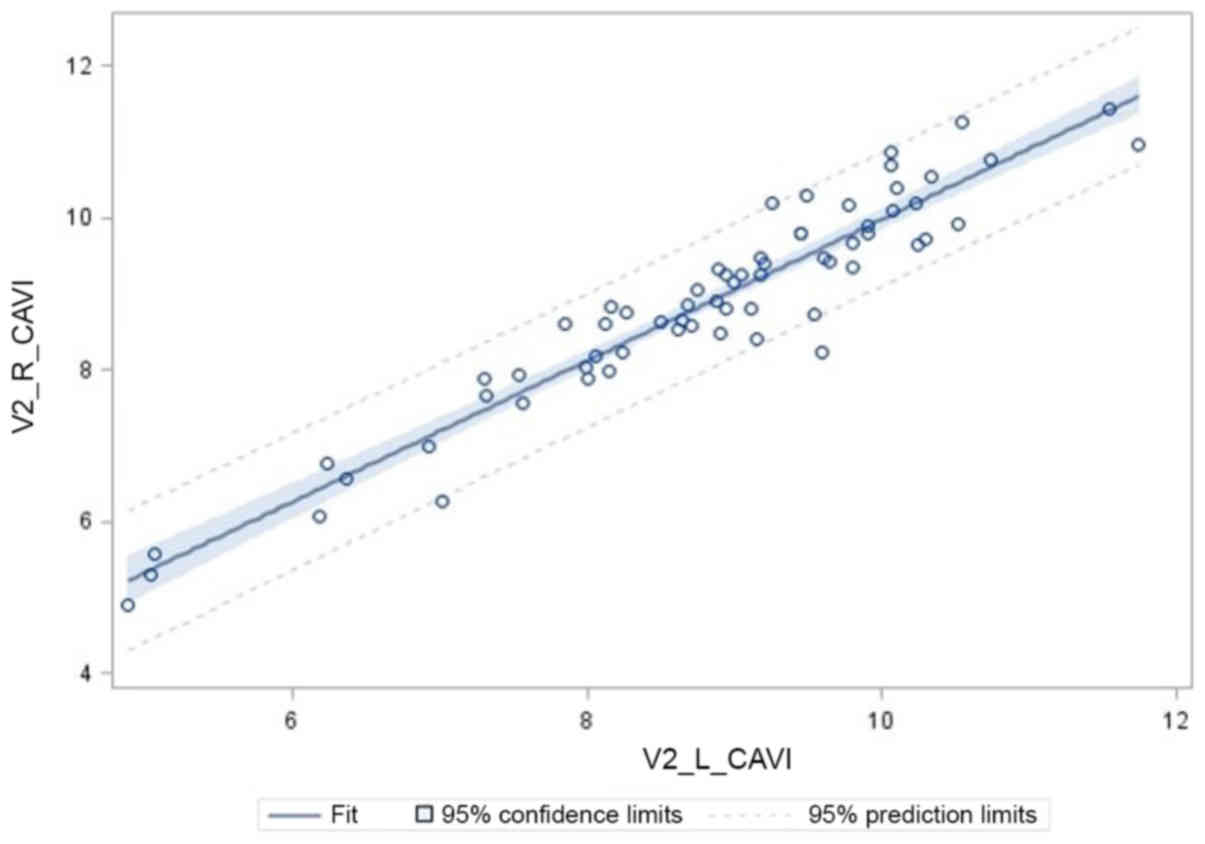
The primary objective of this study was reduction in CAVI over a 3-month period. As shown in Table I, CAVI was significantly reduced on the right arm by 0.64±1.09, relative to the placebo group reduction of 0.11±0.92 (P=0.04). On the left arm, CAVI was trending toward a significant reduction by 0.79±1.58, relative to 0.16±1.05 in the placebo group (P=0.07). The reduction based upon the average of both arms was 0.71±1.27 in AGE vs. 0.13± 0.94 (P=0.04). As shown Table II, the CAVI measures completed on the right and left arms for both visits were highly and significantly correlated, (Pearsons's r for visit 1 = 0.89, P<0.0001; visit 2 = 0.95, P<0.0001) indicating a high degree of consistency in the CAVI measures (Figs. 2 and 3).
Discussion
To the best of our knowledge, this is the first study to demonstrate the effects of AGE on arterial stiffness by improving endothelial function, which was measured by CAVI over a period of 3 months in patients with type 2 diabetes. Diabetic patients with a high 10-year atherosclerotic cardiovascular disease (ASCVD) risk score have been noted to have high CAVI (>9) (15). CAVI is independent of blood pressure and highly reproducible, which is significantly higher in patients with coronary artery stenosis (1,6–9,16). In comparison to PWV, CAVI reflects the smooth muscle contraction rather than changes in BP, and changes over a short period of time in response to sympathetic tone and pharmacological influences (17). The current study demonstrated AGE reduced the arterial stiffness, which was demonstrated by CAVI, which inturn reduces the risk of coronary events.
Arterial stiffness increases with age through the loss of elastin and collagen fibers, which results in increased blood pressure (18). Kobayashi et al (19) demonstrated the significant association between endothelial dysfunction and increased arterial stiffness. Tomiyama et al (20) demonstrated the significant association of bFMD endothelial measurements with arterial stiffness assessed by PWV. Previous studies have indicated that treatments targeting to reduce arterial stiffness and wave reflections can reduce the risk of CVD along with a reduction in BP (21). Larijani et al (11) demonstrated the beneficial effects of AGE and CoQ10 on vascular elasticity and endothelial function in firefighters (mean reduction of PWV, 1.21; 95% CI, −2.1 to −0.32; P=0.005). Ried and Fakler (22) demonstrated the potential effect of garlic in lowering BP through a meta-analysis, including 20 clinical trials with hypertensive individuals (8–9 mmHg of SBP and 6–7 mmHg of DBP; P<0.0001). Furthermore, Breithaupt-Grögler et al (23) demonstrated the protective effects of garlic extract on arterial stiffness assessed by PWV (active vs. placebo; 8.3±1.46 vs. 9.8±2.45 m/sec; P<0.0001) and pressure-standardized elastic vascular resistance (EVR) (active vs. placebo; 0.63±0.21 vs. 0.9±0.44 m2 · sec-2 · mm Hg-1; P<0.0001) compared to the placebo. The results of the current study are consistent with those of previous studies and the mean of both right and left CAVI was significantly improved in AGE group relative to the placebo (0.71+1.27 vs. 0.13+0.94; P=0.04).
Oxidative stress and systemic inflammation play a key role in endothelial dysfunction, which impairs the pathways leading to the production of endothelial-derived relaxing factors, such as nitric oxide (NO), prostacyclin, tissue plasminogen activator and vasoconstrictors (eg, leukotrienes and endothelin-1) (24). Increased oxidative stress accelerates the production of reactive oxygen species (ROS), leading to the inactivation of two anti-atherosclerotic enzymes, such as endothelial nitric oxide synthase (eNOS) and prostacyclin synthases (25,26). Endogenous NO is a potent vasodilator and is produced by two pathways. The first one is by the oxidation of L-arginine in the vascular endothelium by eNOS and the other is by reducing the dietary nitrate (NO3-) to nitrite (NO2-) to NO (27,28). The uncoupling of NOS is a mechanism which plays a critical role in endothelial dysfunction, resulting in the generation of high levels of superoxide (O2-), leading to the formation of potent oxidant peroxynitrite (ONOO-), which is highly toxic, damaging biomolecules, including proteins, lipids and DNA (22,29). Previous studies have used bFMD as an index of endothelial NO regulation of vascular tone, and targeting ROS with vitamin C and dietary nitrate supplement improved vascular function in a number of conditions known to be associated with excess oxidative stress (e.g., type II diabetes, hypertension and CAD) (30–32).
AGE contains water soluble S-allyl cysteine (SAC) and S-allymercaptocysteine (SAMC), which have potent antioxidant properties to protect the vascular endothelium from oxidative stress (11) and has also been reported to have a cholesterol-lowering effect (33). The thiol components (γ-glutamylcysteine) of garlic have the ability to reduce blood pressure by modulating NO, H2S and endothelial synthesis as previously described (21,34–36). Furthermore, AGE has been shown to exert an anti-inflammatory effect by decreasing the expression of CD36 on foam cells and oxidized LDL uptake by macrophages (37). Taken together, the antioxidant and anti-inflammatory properties of garlic increase the enzymatic activity of endothelial cells, such as eNOS, catalase, glutathione peroxidase and superoxide reductase to maintain vascular hemostasis, which may be useful for the prevention of CVD (38).
The current study has several limitations. First, the sample size was relatively small and follow-up was relatively short-term to demonstrate the effects of AGE on BP. Second, patients were under different therapies for hyperlipidemia, hypertension and type 2 diabetes mellitus at different doses. Due to our small sample size, a separate analysis by different background medications was not performed.
In conclusion, this study indicates that at the end of 3 months, the change in CAVI was significantly greater in the AGE group than in the placebo group. Further studies however, are required to evaluate whether AGE has the ability to improve arterial stiffness and endothelial function and thereby decrease adverse cardiovascular events.
Acknowledgements
Not applicable.
Funding
This study was funded by Wakunaga of America Co., Ltd., Mission Viejo, CA, USA.
Availability of data and materials
All data generated or analyzed during this study are included in this published article or are available from the corresponding author on reasonable request.
Authors' contributions
MJB conceived of and designed the study. SH, LC, DB, BTC and MJB collected the patient information and generated the clinical data. AK, LC, DB, SM, KS, FF, SKR and MJB analyzed and/or interpreted the data; and SH, LC, DB, AK, KS, BTC, FF and MJB drafted or revised the manuscript. All authors have read and approved the final version of the manuscript.
Ethics approval and consent to participate
All patients were enrolled in this study after signing a written informed consent that was approved by the Institutional Review Board (IRB) of the Lundquist Institute for Biomedical Innovation at Harbor UCLA Medical Center (NCT03931434).
Patient consent for publication
Not applicable.
Competing interests
MJB discloses work for the National Institutes of Health and General Electric Healthcare. All the other authors declare that they have no competing interests.
References
|
Nakamura K, Tomaru T, Yamamura S, Miyashita Y, Shirai K and Noike H: Cardio-ankle vascular index is a candidate predictor of coronary atherosclerosis. Circ J. 72:598–604. 2008. View Article : Google Scholar : PubMed/NCBI | |
|
Endemann DH and Schiffrin EL: Endothelial dysfunction. J Am Soc Nephrol. 15:1983–1992. 2004. View Article : Google Scholar : PubMed/NCBI | |
|
Williams MJA, Sutherland WHF, McCormick MP, Yeoman DJ and de Jong SA: Aged garlic extract improves endothelial function in men with coronary artery disease. Phytother Res. 19:314–319. 2005. View Article : Google Scholar : PubMed/NCBI | |
|
Huck CJ, Bronas UG, Williamson EB, Draheim CC, Duprez DA and Dengel DR: Noninvasive measurements of arterial stiffness: Repeatability and interrelationships with endothelial function and arterial morphology measures. Vasc Health Risk Manag. 3:343–349. 2007.PubMed/NCBI | |
|
Shekar C, Li D, Cherukuri L, Shaikh K, Hamal S, Birudaraju D, Shodhan S, Nezarat N, Dailing C, Flores F, et al: Abstract 16894: Association Between Flow Mediated Vasodilation and Coronary Artery Disease. Circulation. 138:A168942018. | |
|
Kanamoto M, Matsumoto N, Shiga T, Kunimoto F and Saito S: Relationship between coronary artery stenosis and cardio-ankle vascular index (CAVI) in patients undergoing cardiovascular surgery. J Cardiovasc Dis Res. 4:15–19. 2013. View Article : Google Scholar : PubMed/NCBI | |
|
Sairaku A, Eno S, Hondo T, Teragawa H, Nakano Y, Matsuda K, Kisaka T and Kihara Y: Head-to-head comparison of the cardio-ankle vascular index between patients with acute coronary syndrome and stable angina pectoris. Hypertens Res. 33:1162–1166. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
Miyoshi T, Doi M, Hirohata S, Sakane K, Kamikawa S, Kitawaki T, Kaji Y, Kusano KF, Ninomiya Y and Kusachi S: Cardio-ankle vascular index is independently associated with the severity of coronary atherosclerosis and left ventricular function in patients with ischemic heart disease. J Atheroscler Thromb. 17:249–258. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
Izuhara M, Shioji K, Kadota S, Baba O, Takeuchi Y, Uegaito T, Mutsuo S and Matsuda M: Relationship of cardio-ankle vascular index (CAVI) to carotid and coronary arteriosclerosis. Circ J. 72:1762–1767. 2008. View Article : Google Scholar : PubMed/NCBI | |
|
Shaikh K, Cherukuri L, Birudaraju D, Nakanishi R, Almeida S, Jayawardena E, Shekar C, Flores F, Hamal S, Sheikh S, et al: Aged garlic extract reduces low attenuation plaque in coronary arteries of patients with diabetes in a prospective randomized double-blind study. J Am Coll Cardiol. 73:16452019. View Article : Google Scholar | |
|
Larijani VN, Ahmadi N, Zeb I, Khan F, Flores F and Budoff M: Beneficial effects of aged garlic extract and coenzyme Q10 on vascular elasticity and endothelial function: The FAITH randomized clinical trial. Nutrition. 29:71–75. 2013. View Article : Google Scholar : PubMed/NCBI | |
|
Zeb I, Ahmadi N, Nasir K, Kadakia J, Larijani VN, Flores F, Li D and Budoff MJ: Aged garlic extract and coenzyme Q10 have favorable effect on inflammatory markers and coronary atherosclerosis progression: A randomized clinical trial. J Cardiovasc Dis Res. 3:185–190. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Dhananjayan R, Koundinya KSS, Malati T and Kutala VK: Endothelial dysfunction in type 2 diabetes mellitus. Indian J Clin Biochem. 31:372–379. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Hutchins E, Shaikh K, Kininger A, Cherukuri L, Birudaraju D, Mao SS, Nakanishi R, Almeida S, Jayawardena E, Shekar C, Flores F, et al: Aged garlic extract reduces left ventricular myocardial mass in patients with diabetes: A prospective randomized controlled double-blind study. Exp Ther Med (In Press). | |
|
Park SY, Chin SO, Rhee SY, Oh S, Woo JT, Kim SW and Chon S: Cardio-Ankle Vascular Index as a Surrogate Marker of Early Atherosclerotic Cardiovascular Disease in Koreans with Type 2 Diabetes Mellitus. Diabetes Metab J. 42:285–295. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Horinaka S, Yabe A, Yagi H, Ishimura K, Hara H, Iemua T and Matsuoka H: Comparison of atherosclerotic indicators between cardio ankle vascular index and brachial ankle pulse wave velocity. Angiology. 60:468–476. 2009. View Article : Google Scholar : PubMed/NCBI | |
|
Sun CK: Cardio-ankle vascular index (CAVI) as an indicator of arterial stiffness. Integr Blood Press Control. 6:27–38. 2013. View Article : Google Scholar : PubMed/NCBI | |
|
Mattace-Raso FUS, van der Cammen TJM, Hofman A, van Popele NM, Bos ML, Schalekamp MADH, Asmar R, Reneman RS, Hoeks AP, Breteler MM, et al: Arterial stiffness and risk of coronary heart disease and stroke: The Rotterdam Study. Circulation. 113:657–663. 2006. View Article : Google Scholar : PubMed/NCBI | |
|
Kobayashi K, Akishita M, Yu W, Hashimoto M, Ohni M and Toba K: Interrelationship between non-invasive measurements of atherosclerosis: Flow-mediated dilation of brachial artery, carotid intima-media thickness and pulse wave velocity. Atherosclerosis. 173:13–18. 2004. View Article : Google Scholar : PubMed/NCBI | |
|
Tomiyama H, Ishizu T, Kohro T, Matsumoto C, Higashi Y, Takase B, Suzuki T, Ueda S, Yamazaki T, Furumoto T, et al: Longitudinal association among endothelial function, arterial stiffness and subclinical organ damage in hypertension. Int J Cardiol. 253:161–166. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Boutouyrie P, Fliser D, Goldsmith D, Covic A, Wiecek A, Ortiz A, Martinez-Castelao A, Lindholm B, Massy ZA, Suleymanlar G, et al: Assessment of arterial stiffness for clinical and epidemiological studies: Methodological considerations for validation and entry into the European Renal and Cardiovascular Medicine registry. Nephrol Dial Transplant. 29:232–239. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Ried K and Fakler P: Potential of garlic (Allium sativum) in lowering high blood pressure: Mechanisms of action and clinical relevance. Integr Blood Press Control. 7:71–82. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Breithaupt-Grögler K, Ling M, Boudoulas H and Belz GG: Protective effect of chronic garlic intake on elastic properties of aorta in the elderly. Circulation. 96:2649–2655. 1997. View Article : Google Scholar : PubMed/NCBI | |
|
Lerman A and Zeiher AM: Endothelial function: Cardiac events. Circulation. 111:363–368. 2005. View Article : Google Scholar : PubMed/NCBI | |
|
Craige SM, Kant S and Keaney JF Jr: Reactive oxygen species in endothelial function - from disease to adaptation. Circ J. 79:1145–1155. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Du X, Edelstein D, Obici S, Higham N, Zou M-H and Brownlee M: Insulin resistance reduces arterial prostacyclin synthase and eNOS activities by increasing endothelial fatty acid oxidation. J Clin Invest. 116:1071–1080. 2006. View Article : Google Scholar : PubMed/NCBI | |
|
Duncan C, Dougall H, Johnston P, Green S, Brogan R, Leifert C, Smith L, Golden M and Benjamin N: Chemical generation of nitric oxide in the mouth from the enterosalivary circulation of dietary nitrate. Nat Med. 1:546–551. 1995. View Article : Google Scholar : PubMed/NCBI | |
|
Lundberg JO and Govoni M: Inorganic nitrate is a possible source for systemic generation of nitric oxide. Free Radic Biol Med. 37:395–400. 2004. View Article : Google Scholar : PubMed/NCBI | |
|
Förstermann U and Sessa WC: Nitric oxide synthases: regulation and function. Eur Heart J. 33:829–837, 837a-837d. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Carlström M, Larsen FJ, Nyström T, Hezel M, Borniquel S, Weitzberg E and Lundberg JO: Dietary inorganic nitrate reverses features of metabolic syndrome in endothelial nitric oxide synthase-deficient mice. Proc Natl Acad Sci USA. 107:17716–17720. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
Lara J, Ashor AW, Oggioni C, Ahluwalia A, Mathers JC and Siervo M: Effects of inorganic nitrate and beetroot supplementation on endothelial function: A systematic review and meta-analysis. Eur J Nutr. 55:451–459. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Levine GN, Frei B, Koulouris SN, Gerhard MD, Keaney JF Jr and Vita JA: Ascorbic acid reverses endothelial vasomotor dysfunction in patients with coronary artery disease. Circulation. 93:1107–1113. 1996. View Article : Google Scholar : PubMed/NCBI | |
|
Ackermann RT, Mulrow CD, Ramirez G, Gardner CD, Morbidoni L and Lawrence VA: Garlic shows promise for improving some cardiovascular risk factors. Arch Intern Med. 161:813–824. 2001. View Article : Google Scholar : PubMed/NCBI | |
|
Sendl A, Elbl G, Steinke B, Redl K, Breu W and Wagner H: Comparative pharmacological investigations of Allium ursinum and Allium sativum. Planta Med. 58:1–7. 1992. View Article : Google Scholar : PubMed/NCBI | |
|
Kim-Park S and Ku DD: Garlic elicits a nitric oxide-dependent relaxation and inhibits hypoxic pulmonary vasoconstriction in rats. Clin Exp Pharmacol Physiol. 27:780–786. 2000. View Article : Google Scholar : PubMed/NCBI | |
|
Benavides GA, Squadrito GL, Mills RW, Patel HD, Isbell TS, Patel RP, Darley-Usmar VM, Doeller JE and Kraus DW: Hydrogen sulfide mediates the vasoactivity of garlic. Proc Natl Acad Sci USA. 104:17977–17982. 2007. View Article : Google Scholar : PubMed/NCBI | |
|
Ide N, Keller C and Weiss N: Aged garlic extract inhibits homocysteine-induced CD36 expression and foam cell formation in human macrophages. J Nutr. 136 (Suppl):755S–758S. 2006. View Article : Google Scholar : PubMed/NCBI | |
|
Ahmadi N, Nabavi V, Zughaib H, Patel N, Rathod A, Flores F, Mao S, Hajsadeghi F and Budoff M: Aged Garlic Extract with Supplement is Associated with Beneficial Effect on Bone Mineral Density and Predicts Lack of Progression of Atherosclerosis: A Prospective Double Blinded Randomized Trial. Int J Cardiovasc Res. 4:32015. |