Anti‑epileptic mechanism of isopimaric acid from Platycladi cacumen based on network pharmacology, molecular docking and biological validation
- Authors:
- Published online on: July 3, 2024 https://doi.org/10.3892/etm.2024.12637
- Article Number: 348
-
Copyright: © Wang et al. This is an open access article distributed under the terms of Creative Commons Attribution License.
Abstract
Introduction
Epilepsy is a common neurological disorder caused by abnormal brain discharge, characterized by recurrent limb twitching and loss of consciousness. It affects ~1% of the global population. Currently, antiseizure medication (ASM) is the primary treatment for epilepsy (1). However ~30% of cases remain medically intractable, resulting in a heavy economic burden on patients and society (2). Therefore, it is necessary to develop novel ASMs that effectively control seizures.
Platycladi cacumen (PC), a widely used traditional Chinese medicine, is derived from dry twigs and leaves of Platycladi orientalis (L.) Franco. It is traditionally used to cool blood, stanch bleeding, dispel pathogenic winds, remove dampness, eliminate phlegm and raise hair and blacken hair (3). Recently, PC was shown to exert anti-inflammatory, antioxidative and neuroprotective effects (4). Aqueous extracts of PC suppress lipopolysaccharide (LPS)-induced intestinal inflammation by increasing colon length and inhibiting fecal occult blood, severe diarrhea and enteritis (5). PC carbonisata-derived nanoparticles inhibit ulcerative colitis induced by 2,4,6,-trinitrobenzenesulfonic acid in rats by decreasing tumor necrosis factor-α (TNF-α) and interleukin-6 and upregulating interleukin-10(4). Furthermore, denuded mice treated with water extract of PC for 4 weeks exhibit increased hair growth with increasing hair bulb size and dermis and epidermal thickness (6). A similar effect was found with volatile oil extracts of PC (7). Furthermore, PC exerts renoprotective effects by targeting renal organic anion transporters 1 and 3 to inhibit protein activity (8). A total of 43 compounds have been extracted and separated by 75% methanol from PC and grouped as organic acids, flavonoids, phenylpropanoids, volatile oils and tannins (9). Among them, myricitrin, quercitrin and amentoflavone are the primary compounds (10) that ameliorate liver ischemia-reperfusion and (11) kidney injury (11) and inhibit platelet activation in arterial thrombosis (12) and human breast cancer (13).
The efficacy of PC against epilepsy has been reported in ‘Effective Prescription for Epilepsy Treatment’ (14). However, its anti-epileptic components and underlying mechanisms remain unclear. Therefore, in the present study, the anti-epileptic compound PC was explored using network pharmacology and in vitro experiments.
Materials and methods
Construction of an ‘Herbs-Components-Targets’ (H-C-T) network
The Traditional Chinese Medicine System Pharmacology Database (TCMSP) was used to identify the active ingredients of PC (15), of which, the components whose toxicokinetic absorption, distribution, metabolism and excretion (ADME) adhered to oral bioavailability (OB) ≥30% and drug-likeness (DL) ≥0.18 were defined as the main compounds. Druggable compounds that may cross the blood-brain barrier (BBB) as predicted by SwissADME (swissadme.ch/index.ph) were further used to identify targets on the SwissTargetPrediction (SWISS; new.swisstargetprediction.ch/) and similarity ensemble approach (SEA; sea.bkslab.org/) websites by using relative Canonical Simplified Molecular Input Line Entry System (SMILES) numbers.
Genes associated with epilepsy were obtained from GeneCards (version 4.9.0; genecards.org/). Overlapping genes between targets of the druggable compounds and epilepsy-associated targets were retrieved using VENN map (bioinformatics.psb.ugent.be/webtools/Venn/). The protein-protein interaction (PPI) network was analyzed using the protein-protein interaction networks functional enrichment analysis online tool (STRING; string-db.org/) and core genes were obtained using the CytoNCA of Cytoscape3.9.1 (cytoscape.org/) with the criteria of two-fold the median value of degree centrality (DC), median values of betweenness centrality (BC) and closeness centrality (16). The H-C-T network of PC was constructed using Cytoscape3.9.1.
Gene functions and pathway analysis
Gene Ontology (GO) biological process, cellular component and molecular function and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathways were analyzed among the overlapping genes using the web-based tool DAVID v6.8 (david.ncifcrf.gov/tools.jsp) (17). P<0.05 (Bonferroni-corrected) was considered to indicate statistical significance.
Cell culture and proliferation assay
The murine microglial cell line BV2 was purchased from Procell Life Science & Technology Co., Ltd. and cultured in high-glucose Dulbecco's modified Eagle's medium (DMEM; Gibco; Thermo Fisher Scientific, Inc.) with 10% fetal bovine serum (Clark Bioscience) and 1% streptomycin/penicillin (Biosharp Life Sciences) in a humidified incubator with 5% CO2 at 37˚C.
Cell proliferation was assessed using Cell Counting Kit-8 (CCK8; Dojindo Molecular Technologies, Inc.). Briefly, cells (1x104/ml) were seeded and cultured in 96-well microplates for 24 h. Cells were treated with isopimaric acid (IPA, Sigma-Aldrich; Merck KGaA; 0.1, 1.0, 10.0, 100.0 and 1,000.0 µM) for 24 h, followed by incubation with 10 µl CCK8 reagent for 1 h all at 37˚C. Absorbance was measured by a microplate reader (BioTek Instruments, Inc.; EPOCH2NS) at 450 nm. Survival rate was calculated as follows (18): Survival rate %=absorbance of IPA/absorbance of control x100%.
Wound healing assay
Confluent BV2 cells (90%) were scratched using a pipette tip and washed three times with PBS to remove non-adherent cells. The cells were incubated with LPS (1 µg/ml; Sigma-Aldrich; Merck KGaA) in the presence or absence of 0.0, 0.1, 1.0, 10.0 or 100.0 µM IPA for 24 h ay 37˚C. Images of the central cell-free zone before and after treatment were obtained by light field microscopy (magnification, x200; Zeiss X-Cite; Carl Zeiss AG) (19). The migratory area was calculated as follows: Migratory area (%)=[(area at 0 h - area at 24 h)/area at 0 h] x100%.
LDH assay
The medium of cells treated with LPS in the presence or absence of IPA was collected to determine the released LDH content using assay kits (no. A020-2-2; Nanjing Jiancheng Bioengineering Institute) as previously described (20).
Flow cytometric analysis of cellular reactive oxygen species (ROS)
Following treatment with LPS in the presence or absence of IPA for 24 h, cells were incubated at 37˚C with 10 µM 2',7'-dichlorofluorescin diacetate (MedChemExpress) diluted in DMEM for 30 min in the dark. Images were captured using a fluorescence microscope (Zeiss X-Cite; Zeiss AG) and mean intensity was measured using a flow cytometer (NovoCyte; Agilent Technologies, Inc.) in the fluorescein isothiocyanate (FITC) channel.
Annexin Ⅴ-FITC/propidium iodide (PI) analysis for apoptosis
BV2 cells were digested 37˚C for 5 min using trypsin, followed by incubation with Annexin-FITC and PI for 5 min at room temperature (Boster Biological Technology). Fluorescence intensities were detected using a flow cytometer (NovoCyte) with FITC and PI channels, as previously described (21). A total of four populations of cells were distinguished: Viable (no staining), early apoptosis (Annexin Ⅴ+PI-), late apoptotic cells (Annexin Ⅴ+PI+), and necrotic (Annexin Ⅴ-PI+) cells. Apoptosis was determined as early + late apoptosis.
Determination of mitochondrial membrane potential (MMP)
Cells were treated with IPA and LPS for 24 h, followed by incubation with 500 µl JC-1 working solution in the dark (Beyotime Institute of Biotechnology) for 20 min at 37˚C. Images were obtained using a fluorescence microscope in the FITC and PI channels (magnification, x200; Zeiss X-Cite; Carl Zeiss AG).
Reverse transcription-quantitative (RT-q)PCR
Total RNA from BV2 cells was extracted using TRIzol (Invitrogen; Thermo Fisher Scientific, Inc.) and reverse-transcribed to cDNA using MonScript Reverse Transcriptase (cat. no. MR05101; Monad Biotech Co., Ltd.), followed by SYBR Green PCR (cat. no. MQ00401; Monad Biotech Co., Ltd.), according to the manufacturer's protocol as previously described (21). Relative expression levels of target genes were calculated based on the 2-∆∆Cq method using actin as a reference housekeeping gene (22). The primer sequences are listed in Table I.
Western blotting
Total protein was extracted from BV2 cells using a cell lysis buffer (cat. no. P0013, Beyotime Institute of Biotechnology) with a phosphatase inhibitor, while concentrations of proteins were determined by bicinchoninic acid method (Wuhan Boster Biological Technology, Ltd.). Protein lysates (50 µg) were resolved by 10% sodium dodecyl sulfate-polyacrylamide gel electrophoresis and transferred onto a polyvinyl difluoride membrane (MilliporeSigma) via electroblotting. Each blot was blocked by QuickBlock (cat. no. P0256; Beyotime Institute of Biotechnology) for 15 min at room temperature and incubated with primary antibodies overnight at 4˚C (Table II). Membranes were incubated with horseradish peroxidase-conjugated secondary antibodies (Proteintech Group, Inc.; cat. no. 20000858; 1: 2,000; cat. no. 20000757; 1:5,000) for 1 h at 37˚C. The blots were visualized by the ChemiDoc XRS imaging system (Bio-Rad Laboratories, Inc.) with BeyoECL kit (cat. no. 081723240119; Beyotime Institute of Biotechnology) and quantified using ImageJ Software (v1.52a; National Institutes of Health).
Molecular docking
The crystallographic structure of AKT was obtained from the Protein Data Bank (PDB code: 4GV1) (23) and docking by using Schrödinger (version 2015) (24). Briefly, the Protein Preparation Wizard and Receptor Grid Generation modules were used to prepare the proteins. Ionization-generated possible states of the LigPrep module were set at a target pH of 7.0±2.0 to prepare IPA to dock flexibly into the ligand site using a Ligand Docking module in standard precision mode, as previously described (25).
Statistical analysis
Data are presented as the mean ± SD. Normally distributed data were analyzed using the Shapiro-Wilk test and one-way ANOVA followed by Dunn's post hoc test for multiple groups using GraphPad Prism (version 9.0.0; Dotmatics) (26). Non-normally distributed data were analyzed using Kruskal-Wallis test. P<0.05 was considered to indicate a statistically significant difference.
Results
Targets prediction of PC and visualization of H-C-T network
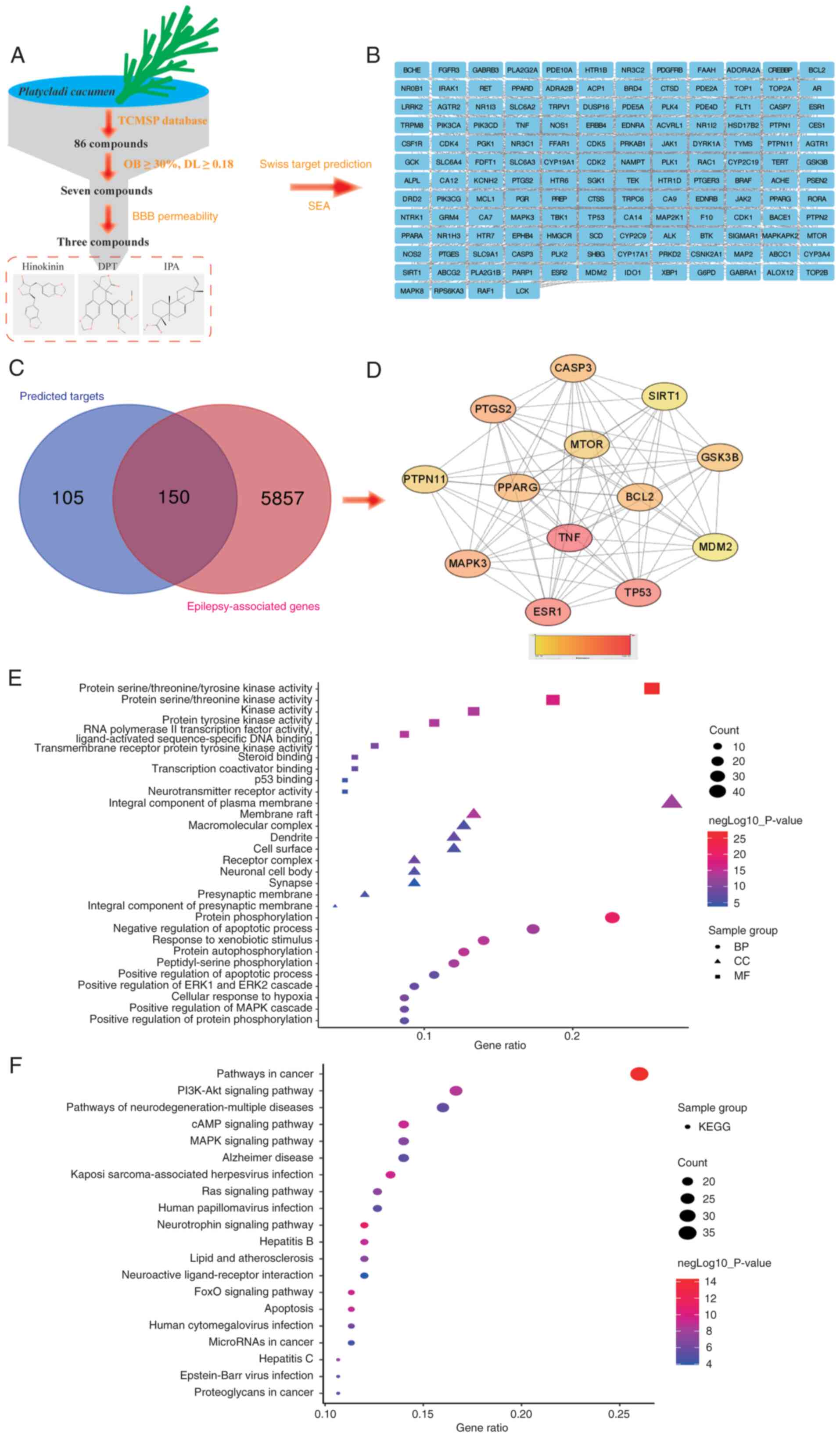
A total of seven primary compounds were obtained from the TCMSP, of which hinokinin, IPA and deoxypicropodophyllotoxin (DPT) exhibited the potential to cross the BBB (Table III; Fig. 1A). Based on SMILES numbers of these three components, 255 potential targets of PC were identified by target fishing from the SWISS and SEA databases, of which 150 were associated with epilepsy (Fig. 1B). These composite targets were input into STRING to construct a PPI network with connected targets (combined score >0.7), including 259 nodes and 308 edges (Fig. 1C). A total of 13 targets, including TNF, tumor protein (TP53), estrogen receptor 1 (ESR1), prostaglandin-endoperoxide synthase 2 (PTGS2), microtubule affinity regulating kinase 3 (MARK3), peroxisome proliferative activated receptor gamma (PPARG), caspase 3 (CASP3), B-cell lymphoma-2 (BCL2), glycogen synthase kinase 3 beta (GSK3B), mammalian target of rapamycin (mTOR), protein tyrosine phosphatase non-receptor type11 (PTPN11), sirtuin1 (SIRT1) and murine double minute 2 (MDM2) exceeded the values (two-fold of DC, median of BC and closeness centrality; Fig. 1D). Among these, BCL2, GSK3B, and mTOR are potential anti-epileptic targets for hinokinin; CASP3, mTOR, and SIRT1 for DPT; and TNF, TP53, ESR1, PTGS2, MAPK3, PPARG, PTPN11, and MDM2 for IPA. In particular, TNF showed the highest subgraph centrality value.
GO and KEGG enrichment analysis
GO and pathway enrichment analyses were performed for overlapping targets (150 genes) that were significantly enriched ‘protein phosphorylation’, ‘negative regulation of apoptotic process’, ‘response to xenobiotic stimulus’, ‘protein autophosphorylation’ and ‘peptidyl-serine phosphorylation’ in the biological processes. In terms of cellular component, the overlapping targets were enriched in the ‘membrane raft’, ‘macromolecular complex’, ‘dendrite’, ‘cell surface’, and ‘receptor complex’. With respect to molecular function, the core targets were enriched in ‘protein serine/threonine/tyrosine kinase activity’, ‘protein serine/threonine kinase activity’, ‘kinase activity’, ‘protein tyrosine kinase activity’, and ‘RNA polymerase II transcription factor activity, ligand-activated sequence-specific DNA binding’ (Fig. 1E). A total of 150 genes were enriched in 140 pathways, of which ‘pathways in cancer’, ‘PI3K-Akt signaling pathway’, ‘pathways of neurodegeneration-multiple diseases’, ‘cAMP signaling pathway’ and ‘MAPK signaling pathway’ were the most enriched (Fig. 1F).
IPA inhibits elevation of ROS production and migration of murine microglia cells induced by glutamate and LPS
IPA serves a role in pathological processes, including antibacterial activity (27) and anti-NLR family, pyrin domain containing protein 3 (NLRP3) inflammasome (28) and anti-Alzheimer's disease effects (29,30). IPA activates large-conductance Ca2+-activated K+ channels (31,32) by targeting gamma-aminobutuyric acid (GABA) receptors to induce chloride ion currents (33). Therefore, it was hypothesized that IPA may be a might be a target compound to treat epilepsy. Hence, glutamate- and LPS-induced excitotoxicity and neuroinflammation in murine microglia cells BV2 were examined to determine the anti-epileptic effects of IPA, as previously described (34).
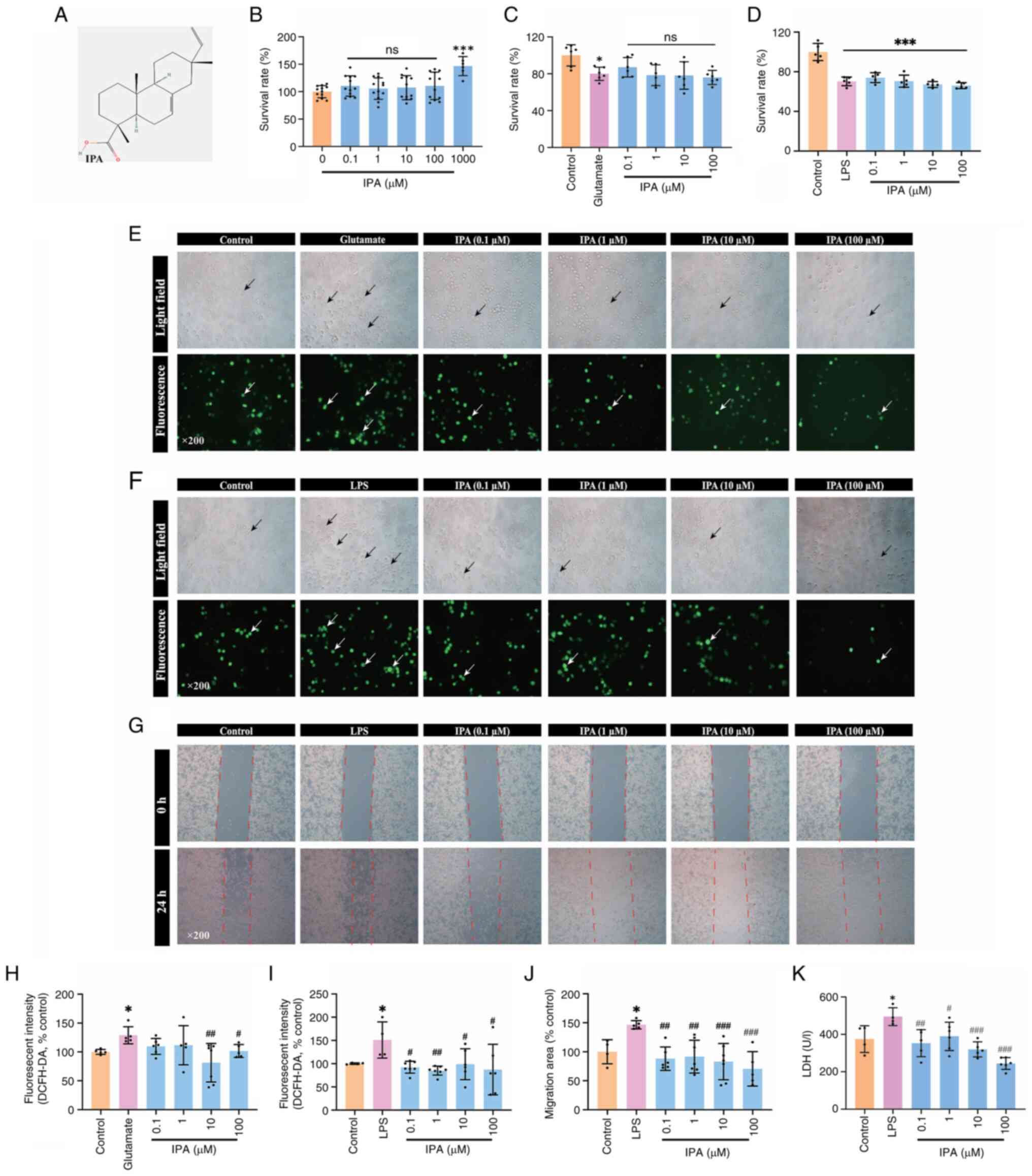
IPA (0.1-1,000.0 µM) was used to verify its effect on the survival of BV2 cells. Concentrations of IPA from 0.1 to 100.0 µM did not affect the survival rate of BV2 cells and were applied in subsequent experiments (Fig. 2A and B). BV2 cells treated with glutamate (5 mM) for 12 h and LPS (1 µg/ml) for 24 h notably suppressed the survival rate. However, co-administration of IPA did not improve the survival of BV2 cells (Fig. 2C and D) but significantly suppressed the production of ROS induced by glutamate (Fig. 2E and F) and LPS (Fig. 2G and H).
IPA significantly inhibited the wound closure of BV2 induced by LPS (0.1, 1.0, 10.0 and 100 µM IPA corresponded to 88.10±20.17, 91.55±28.29, 83.03±11.79 and 70.55±29.71%, respectively, compared with 146.60±7.19% migration area in the LPS group; Fig. 2I and J) and decreased LDH release (0.1, 1.0, 10.0 and 100.0 µM IPA doses corresponded to 352.93±72.37, 389.63±75.72, 319.76±40.31, and 244.11±31.44, respectively, compared with 495.12±47.63 U/l in the LPS group; Fig. 2K).
IPA suppresses LPS-induced apoptosis in BV2 cells
Treatment with IPA in the range of 0.1-100.0 µM prevented the LPS-induced late phase of apoptosis (LPS, 9.94±6.05%; 0.1 µM, 3.47±1.30%; 1 µM, 4.19±1.58%; 10 µM, 4.40±2.10%; 100 µM, 4.33±2.88%; Fig. 3A-C). It was confirmed by MMP that BV2 cells treated with IPA showed decreased JC-1 monomers compared with the LPS group (Fig. 3D).
IPA suppresses mRNA expression of anti-oxidative genes including superoxide dismutase (SOD)-1 and SOD-2, inflammatory genes (IL-1β and TNF-α) and M2-polarization genes (Arg-1) in LPS-treated BV2 cells
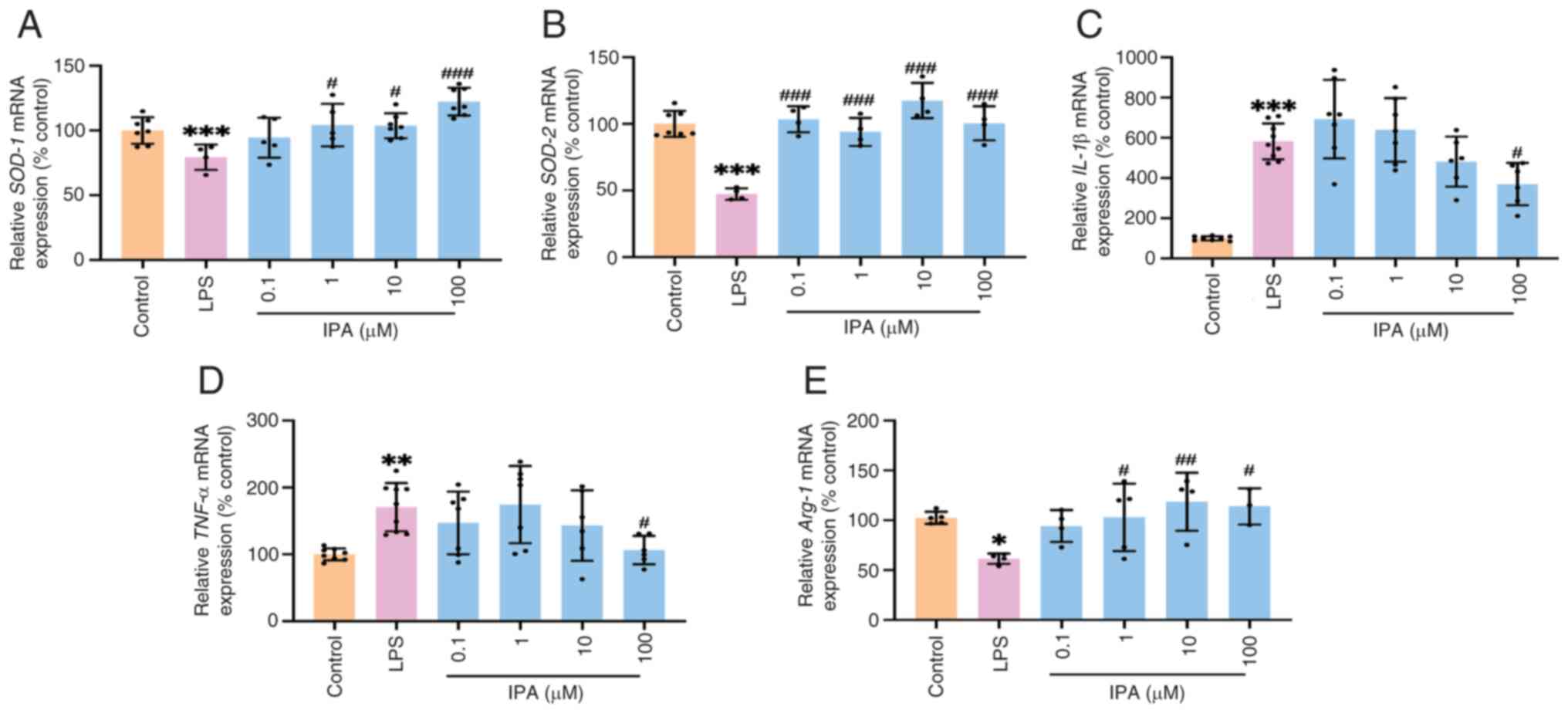
To explore the mechanism of action of IPA, mRNA expression of SOD-1 and SOD-2, which indicate ROS overload (35), was assessed. IPA at concentrations of 1, 10, and 100 µM significantly increased mRNA expression of SOD-1 and SOD-2 (Fig. 4A and B). LPS induced significant increases of the mRNA expression of inflammatory genes including IL-1β (Fig. 4C) and TNF-α (Fig. 4D), while 100 µM of IPA significantly decreased the mRNA expression of IL-1β and TNF-α. Furthermore, it was demonstrated that LPS suppressed the mRNA expression of Arg-1, a specific surface phenotype marker of M2(36). IPA at concentrations of 1, 10, and 100 µM significantly increased the mRNA expression of Arg-1, indicating that IPA induced the polarization of BV2 to M2 (Fig. 4E).
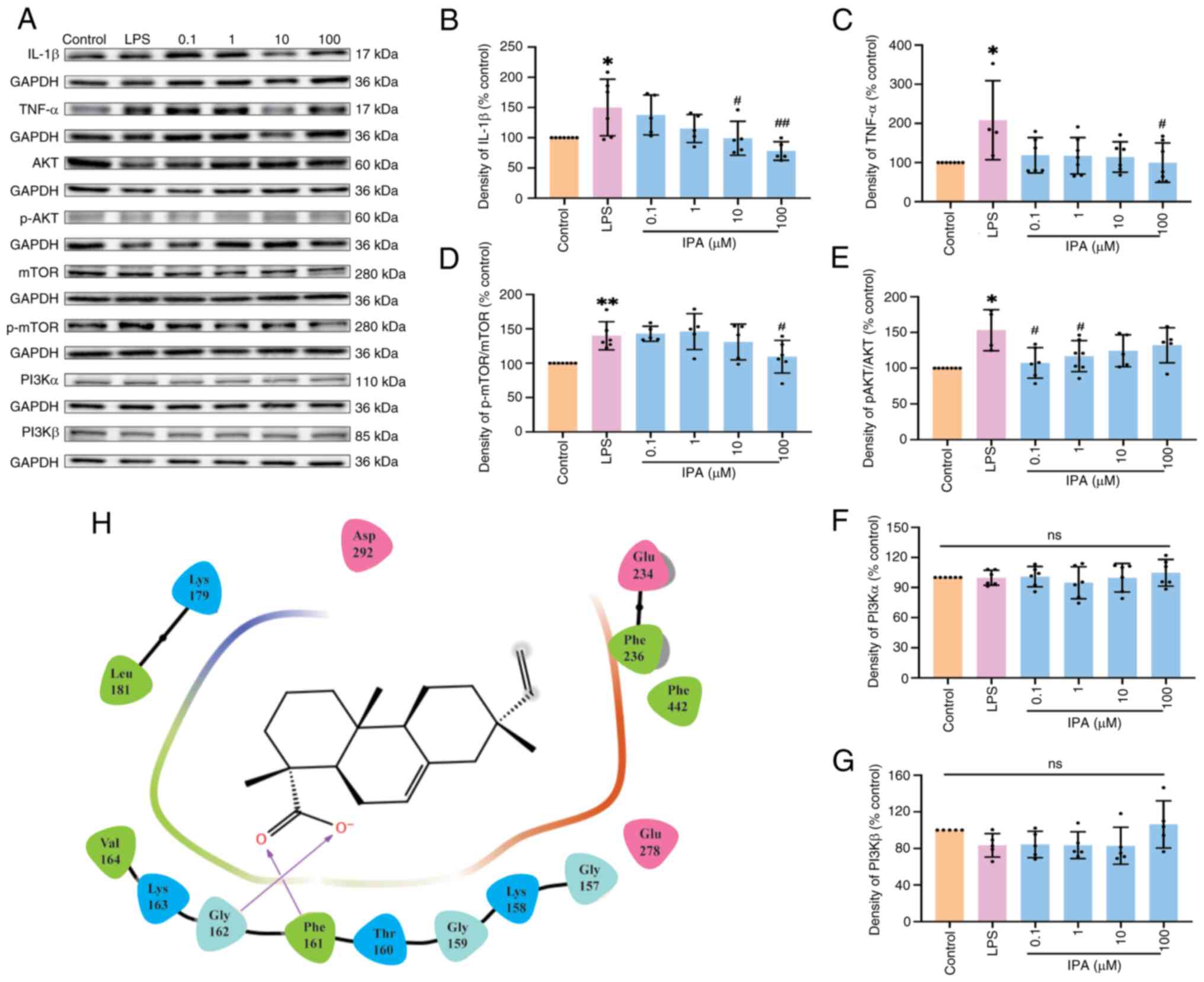
IPA suppresses protein expression of IL-1β and TNF-α by inhibiting the phosphorylation of hyperactive mTOR and AKT
Protein expression of hub (TNF-α and mTOR) and PI3K/AKT signaling pathway genes (AKT and p-AKT; Fig. 5A) were assessed. IPA inhibited protein expression of IL-1β (Fig. 5B) and TNF-α (Fig. 5C) compared with the LPS group. IPA also suppressed phosphorylation of mTOR (Fig. 5D) and AKT (Fig. 5E) but not of phosphatidylinositol 3-kinase (PI3K)α and β (Fig. 5F and G). Furthermore, molecular docking results confirmed that two oxygen atoms of carboxyl in IPA docked on the key Phe161 and Gly162 residue of AKT, which may interrupt the phosphorylation of AKT (37) (Fig. 5H).
Discussion
A total of ~40 antiepileptic drugs have been used to treat epileptic patients in clinical settings (38). However, most control the occurrence of acute seizures and do not exert a true antiepileptogenic effect. Currently, ~30% of patients with epilepsy experience uncontrollable seizures (39). Therefore, exploring novel antiepileptic drugs that impede epileptogenesis is vital for treating refractory epilepsy. Chinese herbal medicines including Gastrodia elata, Uncaria rhynchophylla, Acrori tatarinowii, Paeonia lactiflora, Bupleurum Chinese and PC have been used to treat seizures and epilepsy for thousands of years (40-42). The present study demonstrated that three compounds from PC, hinokinin, DPT and IPA showed druggability in crossing the BBB. In total, 150 predicted targets were associated with epilepsy, suggesting that hinokinin, DPT and IPA are potential components of PC against epilepsy.
Microglia are the primary glial cells in the central nervous system and act as immune protectors to maintain stability of the nerve cell microenvironment. Upon abnormal stimulation, microglia are transformed, exhibiting cellular structures varying from ramified to amoeboid, and enhancing migration to the injured region (43), where they induce release of inflammatory cytokines (IL-1β and TNF-α), and cause inflammation (44). Microglial activation and inflammation have been observed in the brain of patients with refractory epilepsy (45,46), which increases neuronal excitability and contributes to epileptogenesis (47). In the present study, IPA, a diterpenoid compound separated from PC (48), alleviated glutamate- and LPS-induced oxidative stress and inflammation in BV2 cells, confirming previous studies where IPA not only inhibited production of inflammation protein NF-κB in HBEC3-KT (Homo sapiens lung and bronchial epithelial cells), MRC-5 (Homo sapiens lung fibroblasts), and THP-1 cells (Homo sapiens peripheral blood monocyte) (49), but also suppressed the proliferation and metastasis of breast cancer cells including (MDA-MB-231 and MCF-7) via mitochondrial oxidative phosphorylation signaling pathways (50). In particular, IPA significantly increased mRNA expression of anti-oxidative kinases (SOD-1 and SOD-2) and decreased gene expression of inflammatory factors (IL-1β and TNF-α), suggesting an anti-inflammation role in microglia.
An increasing number of studies have confirmed that hyperactive mTOR is involved in inflammation and apoptosis of microglia during epileptogenesis and is a potential target for epileptic treatment (51,52). Somatic mTOR variants, including p.C1483Y and p.C1483R, have been identified in patients with refractory epilepsy and focal cortical malformation (53), while, kainic acid- and LPS-induced seizures significantly activate mTOR in rats (54,55). The activation of mTOR in microglia enhances inflammatory responses (56). Furthermore, the PI3K/Akt pathway is key for mTOR-involved cell survival and migration (57,58). The present study demonstrated that IPA significantly inhibited phosphorylation of mTOR, confirming a previous study showing that inhibiting the PI3K/Akt/mTOR pathway prevents microglial apoptosis (59). As previous studies have demonstrated that protein expression of PI3Kα and β is significantly increased in acute and chronic epilepsy, independent of phosphorylation levels (60,61), the present study only analyzed the protein expression of PI3Kα and β. However, the present study did not find any changes to PI3Kα and β. Further analysis by molecular docking suggested that IPA may directly combine with AKT at the Phe161 and Gly162 residues and suppress activation of AKT, in line with a previous study that demonstrated residue Phe161 serves a vital role on AKT (37). Overall, the present study suggested that IPA inhibited LPS-induced neuroinflammation via the Akt/mTOR pathway. However, lack of data on the selectivity and specificity of IPA for AKT and mTOR in anti-epileptic activity is a limitation of the present study. Hence, their direct association should be investigated in the future.
In summary, IPA may be a potential anti-epileptic compound in PC that acts by suppressing neuroinflammation, apoptosis and polarization via the Akt/mTOR pathway. These findings indicate that IPA may be a novel anti-epileptic drug.
Acknowledgements
The authors would like to thank Dr Junyu Xu (Hainan Medical University, Haikou, China) for help with molecular docking.
Funding
Funding: The present study was supported by the Hainan Provincial Key Research and Development Program (grant nos. ZDYF2021SHFZ092 and ZDYF2022SHFZ109); Hainan Provincial Natural Science Foundation of China (grant no. 820RC630); Epilepsy Research Science Innovation Group of Hainan Medical University (grant no. 2022); Hainan Province Clinical Medical Center (grant no. 2021); Excellent Talent Team of Hainan Province (grant no. QRCBT202121) and National Natural Science Foundation of China (grant nos. 81960249, 82260270 and 82360838).
Availability of data and materials
The data generated in the present study may be requested from the corresponding author.
Authors' contributions
YaW conceived and designed the study, analyzed data, wrote the manuscript and constructed figures. YuW, CL and DL designed the experiments. YuW performed experiments and constructed figures. YaW, YC, and QL confirm the authenticity of all the raw data. YC and QL designed the experiment, wrote the manuscript, and supervised the study. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
|
Asadi-Pooya AA, Brigo F, Lattanzi S and Blumcke I: Adult epilepsy. Lancet. 402:412–424. 2023.PubMed/NCBI View Article : Google Scholar | |
|
Pitkanen A, Ekolle Ndode-Ekane X, Lapinlampi N and Puhakka N: Epilepsy biomarkers-Toward etiology and pathology specificity. Neurobiol Dis. 123:42–58. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Chinese Pharmacopoeia Commission: Pharmacopoeia of the People's Republic of China. Vol 1. China Medical Science and Technology Press, Beijing, pp292-293, 2015. | |
|
Zhang ML, Liu YH and Qu HH: Protective effect of nanoparticles from Platycladi cacumen carbonisata on 2,4,6-Trinitrobenzene Sulfonic Acid (TNBS)-Induced Colitis in Rats. J Biomed Nanotechnol. 18:422–434. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Zhang HX, Li YY, Liu ZJ and Wang JF: Quercetin effectively improves LPS-induced intestinal inflammation, pyroptosis, and disruption of the barrier function through the TLR4/NF-κB/NLRP3 signaling pathway in vivo and in vitro. Food Nutr Res. 66(8948)2022.PubMed/NCBI View Article : Google Scholar | |
|
Fu H, Li W, Weng Z, Huang Z, Liu J, Mao Q and Ding B: Water extract of cacumen platycladi promotes hair growth through the Akt/GSK3beta/beta-catenin signaling pathway. Front Pharmacol. 14(1038039)2023.PubMed/NCBI View Article : Google Scholar | |
|
Zhang Y, Chen S, Qu F, Su G and Zhao Y: In vivo and in vitro evaluation of hair growth potential of Cacumen Platycladi, and GC-MS analysis of the active constituents of volatile oil. J Ethnopharmacol. 238(111835)2019.PubMed/NCBI View Article : Google Scholar | |
|
Huo X, Meng Q, Wang C, Wu J, Zhu Y, Sun P, Ma X, Sun H and Liu K: Targeting renal OATs to develop renal protective agent from traditional Chinese medicines: Protective effect of Apigenin against Imipenem-induced nephrotoxicity. Phytother Res. 34:2998–3010. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Zhuang B, Bi ZM, Wang ZY, Duan L, Lai CJ and Liu EH: Chemical profiling and quantitation of bioactive compounds in Platycladi Cacumen by UPLC-Q-TOF-MS/MS and UPLC-DAD. J Pharm Biomed Anal. 154:207–215. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Ding M, Li J, Zou S, Tang G, Gao X and Chang YX: Simultaneous extraction and determination of compounds with different polarities from Platycladi cacumen by AQ C(18)-Based vortex-homogenized matrix solid-phase dispersion with ionic liquid. Front Pharmacol. 9(1532)2019.PubMed/NCBI View Article : Google Scholar | |
|
Shen Y, Shen X, Cheng Y and Liu Y: Myricitrin pretreatment ameliorates mouse liver ischemia reperfusion injury. Int Immunopharmacol. 89 (Pt A)(107005)2020.PubMed/NCBI View Article : Google Scholar | |
|
Oh TW, Do HJ, Jeon JH and Kim K: Quercitrin inhibits platelet activation in arterial thrombosis. Phytomedicine. 80(153363)2021.PubMed/NCBI View Article : Google Scholar | |
|
Qiu S, Zhou Y, Kim JT, Bao C, Lee HJ and Chen J: Amentoflavone inhibits tumor necrosis factor-alpha-induced migration and invasion through AKT/mTOR/S6k1/hedgehog signaling in human breast cancer. Food Funct. 12:10196–10209. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Zhang T (ed): Effective Prescription for Treating Epilepsy. 1st edition. People's Military Medical Press, Beijing, 1996 (In Chinese). | |
|
Wang Y, Li C, Xiong Z, Chen N, Wang X, Xu J, Wang Y, Liu L, Wu H, Huang C, et al: Up-and-coming anti-epileptic effect of aloesone in Aloe vera: Evidenced by integrating network pharmacological analysis, in vitro, and in vivo models. Front Pharmacol. 13(962223)2022.PubMed/NCBI View Article : Google Scholar | |
|
Tang Y, Li M, Wang J, Pan Y and Wu FX: CytoNCA: A cytoscape plugin for centrality analysis and evaluation of protein interaction networks. Biosystems. 127:67–72. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Sherman BT, Hao M, Qiu J, Jiao X, Baseler MW, Lane HC, Imamichi T and Chang W: DAVID: a web server for functional enrichment analysis and functional annotation of gene lists (2021 update). Nucleic Acids Res. 50(W1):W216–W221. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Wang J, Sun Y, Zhang X, Cai H, Zhang C, Qu H, Liu L, Zhang M, Fu J, Zhang J, et al: Oxidative stress activates NORAD expression by H3K27ac and promotes oxaliplatin resistance in gastric cancer by enhancing autophagy flux via targeting the miR-433-3p. Cell Death Dis. 12(90)2021.PubMed/NCBI View Article : Google Scholar | |
|
Wang Y, Li Y, Liu D, Zheng D, Li X, Li C, Huang C, Wang Y, Wang X, Li Q and Xu J: A potential anti-glioblastoma compound LH20 induces apoptosis and arrest of human glioblastoma cells via CDK4/6 inhibition. Molecules. 28(5047)2023.PubMed/NCBI View Article : Google Scholar | |
|
Wang Y, Li Y, Wang G, Lu J and Li Z: Overexpression of Homer1b/c induces valproic acid resistance in epilepsy. CNS Neurosci Ther. 29:331–343. 2023.PubMed/NCBI View Article : Google Scholar | |
|
Wang Y, Xiong Z, Li C, Liu D, Li X, Xu J, Chen N, Wang X, Li Q and Li Y: Multiple beneficial effects of aloesone from aloe vera on LPS-Induced RAW264.7 cells, including the inhibition of oxidative stress, inflammation, M1 polarization, and apoptosis. Molecules. 28(1617)2023.PubMed/NCBI View Article : Google Scholar | |
|
Livak KJ and Schmittgen TD: Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 25:402–408. 2001.PubMed/NCBI View Article : Google Scholar | |
|
Addie M, Ballard P, Buttar D, Crafter C, Currie G, Davies BR, Debreczeni J, Dry H, Dudley P, Greenwood R, et al: Discovery of 4-amino-N-[(1S)-1-(4-chlorophenyl)-3-hydroxypropyl]-1-(7H-pyrrolo[2,3-d]pyrimidin-4-yl)piperidine-4-carboxamide (AZD5363), an orally bioavailable, potent inhibitor of Akt kinases. J Med Chem. 56:2059–2073. 2013.PubMed/NCBI View Article : Google Scholar | |
|
Yang Y, Yao K, Repasky MP, Leswing K, Abel R, Shoichet BK and Jerome SV: Efficient Exploration of Chemical Space with Docking and Deep Learning. J Chem Theory Comput. 17:7106–7119. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Xu J, Li H, Wang X, Huang J, Li S, Liu C, Dong R, Zhu G, Duan C, Jiang F, et al: Discovery of coumarin derivatives as potent and selective cyclin-dependent kinase 9 (CDK9) inhibitors with high antitumour activity. Eur J Med Chem. 200(112424)2020.PubMed/NCBI View Article : Google Scholar | |
|
Ying J, Huang Y, Ye X, Zhang Y, Yao Q, Wang J, Yang X, Yu C, Guo Y, Zhang X, et al: Comprehensive study of clinicopathological and immune cell infiltration and lactate dehydrogenase expression in patients with thymic epithelial tumours. Int Immunopharmacol. 126(111205)2024.PubMed/NCBI View Article : Google Scholar | |
|
Smith E, Williamson E, Zloh M and Gibbons S: Isopimaric acid from Pinus nigra shows activity against multidrug-resistant and EMRSA strains of Staphylococcus aureus. Phytother Res. 19:538–542. 2005.PubMed/NCBI View Article : Google Scholar | |
|
Wu XW, Wang Q, Li Q, Cui YM, Pu YK, Shi QQ, Bi DW, Zhang JJ, Zhang RH, Li XL, et al: Rubellawus A-D, four new diterpenoids isolated from callicarpa rubella and Their Anti-NLRP3 inflammasome effects. Chem Biodivers. 17(e2000798)2020.PubMed/NCBI View Article : Google Scholar | |
|
Yamamoto K, Ueta Y, Wang L, Yamamoto R, Inoue N, Inokuchi K, Aiba A, Yonekura H and Kato N: Suppression of a neocortical potassium channel activity by intracellular amyloid-beta and its rescue with Homer1a. J Neurosci. 31:11100–11109. 2011.PubMed/NCBI View Article : Google Scholar | |
|
Wang L, Kang H, Li Y, Shui Y, Yamamoto R, Sugai T and Kato N: Cognitive recovery by chronic activation of the large-conductance calcium-activated potassium channel in a mouse model of Alzheimer's disease. Neuropharmacology. 92:8–15. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Salari S, Silvera Ejneby M, Brask J and Elinder F: Isopimaric acid-a multi-targeting ion channel modulator reducing excitability and arrhythmicity in a spontaneously beating mouse atrial cell line. Acta Physiol (Oxf). 222(e12895)2018.PubMed/NCBI View Article : Google Scholar | |
|
Imaizumi Y, Sakamoto K, Yamada A, Hotta A, Ohya S, Muraki K, Uchiyama M and Ohwada T: Molecular basis of pimarane compounds as novel activators of large-conductance Ca(2+)-activated K(+) channel alpha-subunit. Mol Pharmacol. 62:836–846. 2002.PubMed/NCBI View Article : Google Scholar | |
|
Zaugg J, Khom S, Eigenmann D, Baburin I, Hamburger M and Hering S: Identification and characterization of GABA(A) receptor modulatory diterpenes from Biota orientalis that decrease locomotor activity in mice. J Nat Prod. 74:1764–1772. 2011.PubMed/NCBI View Article : Google Scholar | |
|
Rong S, Wan D, Fan Y, Liu S, Sun K, Huo J, Zhang P, Li X, Xie X, Wang F and Sun T: Amentoflavone affects epileptogenesis and exerts neuroprotective effects by inhibiting NLRP3 inflammasome. Front Pharmacol. 10(856)2019.PubMed/NCBI View Article : Google Scholar | |
|
Chang YC, Fong Y, Tsai EM, Chang YG, Chou HL, Wu CY, Teng YN, Liu TC, Yuan SS and Chiu CC: Exogenous C(8)-Ceramide Induces Apoptosis by Overproduction of ROS and the switch of superoxide dismutases SOD1 to SOD2 in human lung cancer cells. Int J Mol Sci. 19(3010)2018.PubMed/NCBI View Article : Google Scholar | |
|
Xu M, Yang Y, Peng J, Zhang Y, Wu B, He B, Jia Y and Yan T: Effects of Alpinae Oxyphyllae Fructus on microglial polarization in a LPS-induced BV2 cells model of neuroinflammation via TREM2. J Ethnopharmacol. 302(Pt A)(115914)2023.PubMed/NCBI View Article : Google Scholar | |
|
Kashyap MP, Singh AK, Kumar V, Yadav DK, Khan F, Jahan S, Khanna VK, Yadav S and Pant AB: Pkb/Akt1 mediates Wnt/GSK3β/β-catenin signaling-induced apoptosis in human cord blood stem cells exposed to organophosphate pesticide monocrotophos. Stem Cells Dev. 22:224–238. 2013.PubMed/NCBI View Article : Google Scholar | |
|
Ravizza T, Scheper M, Di Sapia R, Gorter J, Aronica E and Vezzani A: mTOR and neuroinflammation in epilepsy: Implications for disease progression and treatment. Nat Rev Neurosci. 25:334–350. 2024.PubMed/NCBI View Article : Google Scholar | |
|
Janson MT and Bainbridge JL: Continuing burden of refractory epilepsy. Ann Pharmacother. 55:406–408. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Lin CH and Hsieh CL: Chinese herbal medicine for treating epilepsy. Front Neurosci. 15(682821)2021.PubMed/NCBI View Article : Google Scholar | |
|
Lu H, Luo M, Chen R, Luo Y, Xi A, Wang K and Xu Z: Efficacy and safety of traditional Chinese medicine for the treatment of epilepsy: A updated meta-analysis of randomized controlled trials. Epilepsy Res. 189(107075)2023.PubMed/NCBI View Article : Google Scholar | |
|
Wu J, Cao M, Peng Y, Dong B, Jiang Y, Hu C, Zhu P, Xing W, Yu L, Xu R and Chen Z: Research progress on the treatment of epilepsy with traditional Chinese medicine. Phytomedicine. 120(155022)2023.PubMed/NCBI View Article : Google Scholar | |
|
Block ML, Zecca L and Hong JS: Microglia-mediated neurotoxicity: Uncovering the molecular mechanisms. Nat Rev Neurosci. 8:57–69. 2007.PubMed/NCBI View Article : Google Scholar | |
|
Hernandez VG, Lechtenberg KJ, Peterson TC, Zhu L, Lucas TA, Bradshaw KP, Owah JO, Dorsey AI, Gentles AJ and Buckwalter MS: Translatome analysis reveals microglia and astrocytes to be distinct regulators of inflammation in the hyperacute and acute phases after stroke. Glia. 71:1960–1984. 2023.PubMed/NCBI View Article : Google Scholar | |
|
Butler T, Li Y, Tsui W, Friedman D, Maoz A, Wang X, Harvey P, Tanzi E, Morim S, Kang Y, et al: Transient and chronic seizure-induced inflammation in human focal epilepsy. Epilepsia. 57:e191–194. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Kumar P, Lim A, Hazirah SN, Chua CJH, Ngoh A, Poh SL, Yeo TH, Lim J, Ling S, Sutamam NB, et al: Single-cell transcriptomics and surface epitope detection in human brain epileptic lesions identifies pro-inflammatory signaling. Nat Neurosci. 25:956–966. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Luo C, Koyama R and Ikegaya Y: Microglia engulf viable newborn cells in the epileptic dentate gyrus. Glia. 64:1508–1517. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Cui X, Cheng L, Liu Q and Jia Y: Isolation, identification and HPLC analysis of active component isopimaric acid in leaves of Platycladus orientalis. Lishizhen Med Mater Med Res. 15:78–79. 2004.(In Chinese). | |
|
Michavila Puente-Villegas S, Apaza Ticona L, Rumbero Sanchez A and Acebes JL: Diterpenes of Pinus pinaster aiton with anti-inflammatory, analgesic, and antibacterial activities. J Ethnopharmacol. 318(Pt B)(117021)2024.PubMed/NCBI View Article : Google Scholar | |
|
Li J, Liu X, Chen L, Zhu X, Yu Z, Dong L, Zhao X, Zou H, Wei Q, Feng Y, et al: Isopimaric acid, an ion channel regulator, regulates calcium and oxidative phosphorylation pathways to inhibit breast cancer proliferation and metastasis. Toxicol Appl Pharmacol. 462(116415)2023.PubMed/NCBI View Article : Google Scholar | |
|
Hodges SL and Lugo JN: Therapeutic role of targeting mTOR signaling and neuroinflammation in epilepsy. Epilepsy Res. 161(106282)2020.PubMed/NCBI View Article : Google Scholar | |
|
Hu Y, Mai W, Chen L, Cao K, Zhang B, Zhang Z, Liu Y, Lou H, Duan S and Gao Z: mTOR-mediated metabolic reprogramming shapes distinct microglia functions in response to lipopolysaccharide and ATP. Glia. 68:1031–1045. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Lai D, Gade M, Yang E, Koh HY, Lu J, Walley NM, Buckley AF, Sands TT, Akman CI and Mikati MA: , et al: Somatic variants in diverse genes leads to a spectrum of focal cortical malformations. Brain. 145:2704–2720. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Huang XY, Hu QP, Shi HY, Zheng YY, Hu RR and Guo Q: Everolimus inhibits PI3K/Akt/mTOR and NF-kB/IL-6 signaling and protects seizure-induced brain injury in rats. J Chem Neuroanat. 114(101960)2021.PubMed/NCBI View Article : Google Scholar | |
|
Russo E, Andreozzi F, Iuliano R, Dattilo V, Procopio T, Fiume G, Mimmi S, Perrotti N, Citraro R, Sesti G, et al: Early molecular and behavioral response to lipopolysaccharide in the WAG/Rij rat model of absence epilepsy and depressive-like behavior, involves interplay between AMPK, AKT/mTOR pathways and neuroinflammatory cytokine release. Brain Behav Immun. 42:157–168. 2014.PubMed/NCBI View Article : Google Scholar | |
|
Zhao XF, Liao Y, Alam MM, Mathur R, Feustel P, Mazurkiewicz JE, Adamo MA, Zhu XC and Huang Y: Microglial mTOR is neuronal protective and antiepileptogenic in the pilocarpine model of temporal lobe epilepsy. J Neurosci. 40:7593–7608. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Zhu F, Kai J, Chen L, Wu M, Dong J, Wang Q and Zeng LH: Akt inhibitor perifosine prevents epileptogenesis in a rat model of temporal lobe epilepsy. Neurosci Bull. 34:283–290. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Bai Q, Wang X, Yan H, Wen L, Zhou Z, Ye Y, Jing Y, Niu Y, Wang L, Zhang Z, et al: Microglia-Derived Spp1 promotes pathological retinal neovascularization via activating endothelial Kit/Akt/mTOR signaling. J Pers Med. 13(146)2023.PubMed/NCBI View Article : Google Scholar | |
|
Du M, Sun Z, Lu Y, Li YZ, Xu HR and Zeng CQ: Osthole inhibits proliferation and induces apoptosis in BV-2 microglia cells in kainic acid-induced epilepsy via modulating PI3K/AKt/mTOR signalling way. Pharm Biol. 57:238–244. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Xiao Z, Peng J, Gan N, Arafat A and Yin F: Interleukin-1β plays a pivotal role via the PI3K/Akt/mTOR signaling pathway in the chronicity of mesial temporal lobe epilepsy. Neuroimmunomodulation. 23:332–344. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Wang P, Nan S, Zhang Y and Fan J: Effects of GABA(B) receptor positive allosteric modulator BHF177 and IRS-1 on apoptosis of hippocampal neurons in rats with refractory epilepsy via the PI3K/Akt pathway. Cell Biol Int. 46:1775–1786. 2022.PubMed/NCBI View Article : Google Scholar |