Comparison of the effects of Wild Nutrition Food‑Grown® vitamin D3 formulation with two conventional formulations on increasing plasma vitamin D levels in healthy participants: A 72‑h, randomised, parallel, comparator study
- Authors:
- Published online on: June 17, 2024 https://doi.org/10.3892/ijfn.2024.37
- Article Number: 3
-
Copyright : © Briskey et al. This is an open access article distributed under the terms of Creative Commons Attribution License [CC BY 4.0].
Abstract
Introduction
Vitamin D is a fat-soluble hormone involved in numerous vital physiological functions, including calcium homeostasis, bone and musculoskeletal health, and the regulation of bone and mineral metabolism (1,2). Despite the critical role of vitamin D, a large proportion of the population are deficient (<20 ng/ml) in this vitamin, with an estimated one billion individuals worldwide having low levels of vitamin D (3). Deficiency and insufficiency are generally caused by inadequate sun exposure and/or chronic disease, as vitamin D is naturally produced when the skin is exposed to UVB rays (4). Due to its essential roles, sufficient vitamin D concentrations are vital for general health.
When the natural endogenous production of vitamin D via UVB exposure is not sufficient to meet the required levels, alternative sources of vitamin D may be required. One source of vitamin D is via foods, with or without fortified vitamin D, such as cod liver oil, cheeses and milks. However, the amount of vitamin D provided per serving can be low (5-7) and may not be sufficient to meet demands. A source of a high concentration of vitamin D is via supplementation. Supplementation has been shown to increase vitamin D levels from a single dose ranging from 2,800 to 300,000 IU (8,9). However, a large vitamin D dose may not be sustainable, and could be toxic with long-term use. The current recommended daily intake of vitamin D is a maximum of 1,000 IU/day (or 7,000 IU weekly) (10,11).
A major issue with vitamin D supplementation is that it is typically poorly absorbed due to its lipophilic nature. Vitamin D is a non-polar, hydrophobic lipid with a low solubility in the aqueous environment of the gastrointestinal tract (12). To help increase absorption, new vitamin D formulations incorporating different forms of vitamin D and technologies (e.g., nanoemulsion formulations) have been developed to increase the absorption efficiency of vitamin D.
The forms of vitamin D3 (cholecalciferol) used in the present study incorporate two conventional pharmaceutical-derived formulations in a tablet and buccal spray form, and one form derived from natural Food-Grown® sources. The Food-Grown® formulation is proposed to have superior absorption, as it is derived from natural sources that the human body recognises as food, and therefore may be more readily absorbed. The aim of the present study was to assess the short-term absorption of a Food-Grown® form of vitamin D3 compared to two conventional forms of vitamin D3 in healthy participants over a 72-h period. It was hypothesised that the different forms of vitamin D3 would result in different absorption amounts and rates. The conventional vitamin D3 (tablet) was expected to have the slowest and lowest absorption, the Food-Grown® vitamin D3 (capsule) the greatest absorption and the buccal spray vitamin D3 (spray) the fastest absorption.
Subjects and methods
Study design
A single dose, randomised study was performed to evaluate the absorption of a Food-Grown® vitamin D (Wild Nutrition UK) compared to two conventional vitamin D formulations. The present study included three groups as follows: Group 1 received 5,000 IU Food-Grown® vitamin D in capsule form (group 1); group 2 received 5,000 IU conventional vitamin D in tablet form (conventional commercial product) (group 2); and group 3 received 5,000 IU conventional vitamin D as a buccal spray (conventional commercial product) (group 3). Each capsule, tablet, or spay contained 1,000 IU vitamin D, with a total of five capsules, tablets, or sprays administered to each subject for a total single dose of 5,000 IU. Due to the different forms of vitamin D administration, the blinding of the participants and investigators was not possible. However, sample and statistical analyses were conducted in a blinded manner. The vitamin D administered to group 1 was provided by the manufacturer (Wild Nutrition UK) and encapsulated under Good Manufacturing Practice conditions. The vitamin D products administered to groups 2 and 3 were purchased off the shelf from a local pharmacy.
Participant information
A total of 31 potential participants initially underwent telephone screening for assessment against the specific inclusion and exclusion criteria prior to enrolment. The inclusion criteria were as follows: An age of 18 to 60 years; in generally good health [no known illnesses and a body mass index (BMI) of 18.5-29.9 kg/m2]; capable of providing informed consent; and agreeing to comply with the study requirements, including attendance at all scheduled blood collection time points. Participants were excluded if they had a previous history of haematological diseases, were concomitantly using anticoagulant drugs, were currently pregnant, had regularly used supplements or foods containing vitamin D in the past 3 months, had a history of chronic alcohol consumption (>14 alcoholic beverages per week), were active smokers or substance abusers, had participated in another trial 1 month prior to the start of the present study, or had any other condition that, in the opinion of the investigator, made the participant unsuitable for inclusion. The present study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Bellberry Limited (approval nos 2022-06-607 on 08-08-2022). All participants provided written informed consent prior to inclusion in the study. A total of 31 eligible participants provided written consent for enrolment.
Data collection
Data were collected from September, 2022 to October, 2022. Once enrolled, the participants were required to attend the study clinic on a specific day having fasted for at least 10 h prior to their arrival. Upon arrival, the participants were provided with a randomization number and had a cannula inserted into their arm and a baseline blood sample was obtained. Once a baseline blood sample was obtained, the participants were provided with their randomised study product to consume with water, followed by a breakfast meal (nutritionally balanced) within 10 min. Following dosing, blood samples were obtained from the cannula in the antecubital vein using a 5-ml syringe and transferred to a 6-ml EDTA-containing vacutainer (BD Biosciences) at 0.25, 0.5, 0.75, 1, 2, 4, 6, 8, 10, 12, 24, 48 and 72 h post-supplementation. Following collection, blood samples were kept cold and centrifuged at 4˚C for 10 min (2,100 x g). Once spun, the plasma was separated and stored at -80˚C until analysis.
During the initial 12 h of testing, participants remained at the clinic and provided with standardised meals known to contain no added vitamin D. Participants left the clinic following the 12-h draw and returned each day for their 24, 48 and 72-h blood draws; during this time, they were provided with a list of foods to avoid. Participants were monitored for any adverse effects throughout the study period.
Biochemical analysis
Plasma concentrations of 25-hydroxyvitamin D were measured using ElectroChemiLuminescence technology for immunoassay analysis. Assay kits (cat. no. 09038078190) and calibrators (cat. no. 09038116190) were used as per the manufacturer's protocols (Vitamin D total G3 Elecsys cobas e 100; Roche Diagnostics) with a lower limit of quantitation of <5 ng/ml. The assay does not distinguish between 25-hydroxyvitamin D2 and 25-hydroxyvitamin D3 and interacts equally with either metabolite. Therefore, the 25-hydroxyvitamin D concentrations reported herein represent total vitamin D as a combination of both molecules.
Data analysis
The area under the curve (AUC) and maximum change from baseline (Cmax) were calculated using baseline-corrected concentrations. Any resulting negative values (i.e., concentrations lower than the baseline) were allocated a value of 0. The AUC was calculated for the absorption data of each participant using the trapezoidal method, and the individual AUC was averaged for the group absorption profile. The Cmax (baseline-corrected) and time to reach the maximum concentration (Tmax) were calculated by determining the specific Cmax and Tmax of each participant and averaging the data for each group.
Statistical analysis
Sample size calculations indicated that 10 participants were required per group for power to detect a 15% difference (150±20 vs. 170±23) in the AUC between any two groups at the completion of the study. The alpha error probability was set to 0.05 and powered at 0.80 with a calculated effect size of 1.16. Statistical analysis was conducted by comparing the result of each group to the other using either GraphPad Prism 8.0 (Dotmatics) or SPSS 25 (IBM Corp.) software. All results were first tested for normality using the Kolmogorov-Smirnov test, and based on the distribution of the data, the appropriate statistical tests were used. Inter-group differences in vitamin D absorption were evaluated using one-way analyses of variance (ANOVA) with Holm-Šídák's multiple comparisons test. General linear mixed modelling was also performed on participant data to compare the group dynamics. Comparisons between groups for sex were conducted using a Fisher's exact test. All tests were two-tailed and a P-value of 0.05 was considered to indicate a statistically significant difference. Results are presented as the mean ± SD unless otherwise stated.
Results
A total of 31 participants completed the study, with 10 participants in group 1 (capsule), 11 participants in group 2 (tablet) and 10 participants in group 3 (spray). The supplement was well tolerated and there were no supplement-related adverse events reported. There were no significant differences between the groups as regards participant demographics (Table I). All participants were healthy, with no known medical conditions. The average BMI of each group was at the top of the normal (groups 1 and 3) or bottom of the overweight (group 2) category. There was no significant difference in baseline vitamin D levels between the groups. The plasma vitamin D levels in groups 1 and 2 were slightly below the recommended vitamin D concentration (20 ng/ml) and those in group 3 were just above the recommended value (Table I).
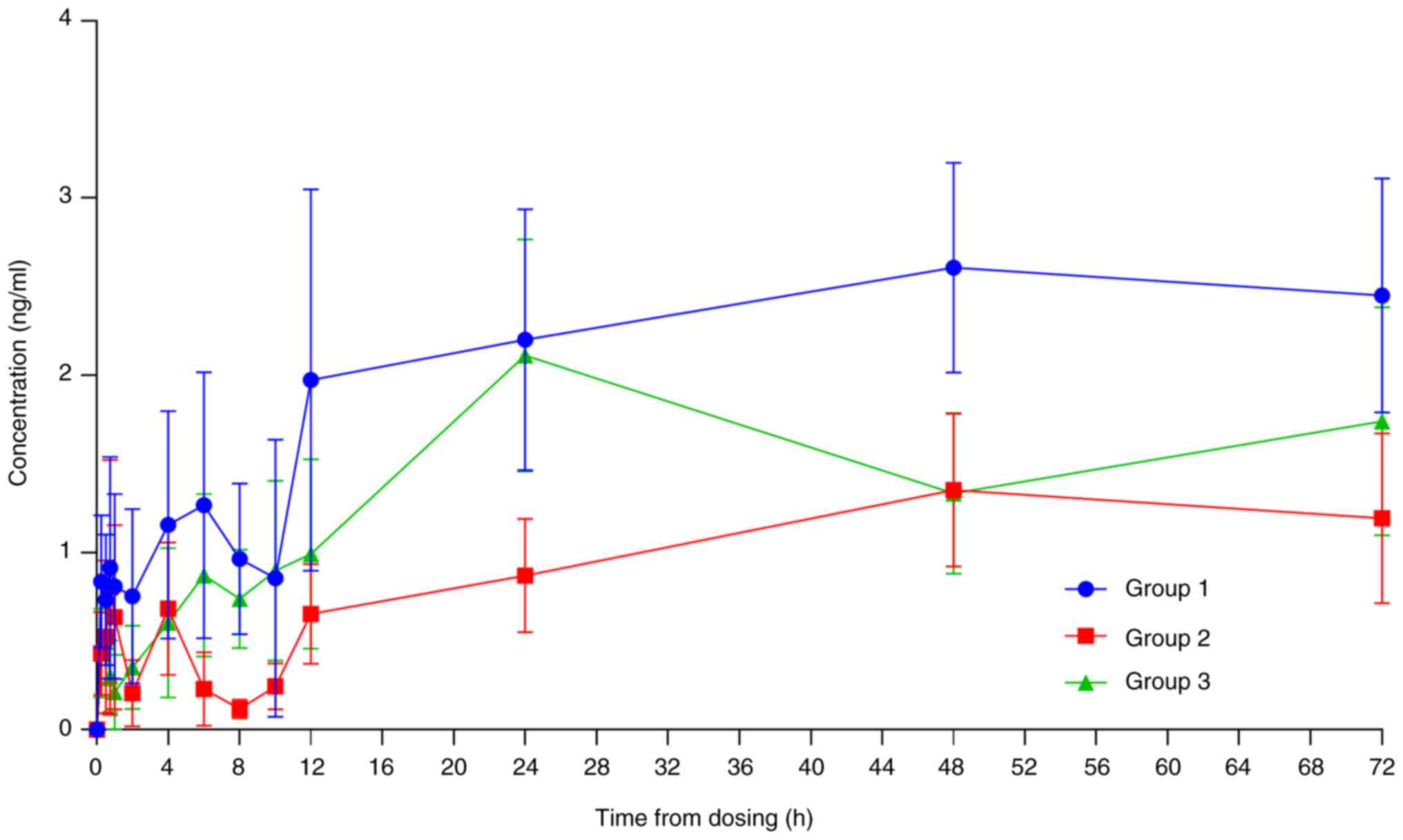
There was a significant increase in total vitamin D absorption (AUC) over the 72-h period in group 1 compared to group 2 (P<0.05; Table II and Fig. 1). There was no statistically significant difference in absorption between the other formulations. The Cmax and Tmax did not differ significantly between the groups (Table II and Fig. 1). There was no statistically significant difference between the groups for the change in vitamin D levels from baseline at any individual time point (Fig. 1). At 72-h post-supplementation, the plasma vitamin D concentrations in groups 1, 2 and 3 remained within 6.0, 17.6 and 11.8% of the Cmax values, respectively.
Table IIGroup average absorption parameters of the three different vitamin D formulations as calculated from individual results. |
Discussion
The aim of the present study was to assess the short-term absorption of a Food-Grown® form of vitamin D compared to two conventional forms of vitamin D in healthy participants. Participants consumed a single 5,000 IU dose with subsequent blood taken over a 72-h period. The analysis of the plasma concentrations of vitamin D revealed the Food-Grown® form of vitamin D to be equivalent to, and even superior to, the existing conventional forms of vitamin D supplementation. The importance of increasing vitamin D absorption from a single small dose is in alignment with the recommended daily intake advised by regulatory authorities. At present, the recommended intake of vitamin D as a supplement varies across countries, although it is generally ~1,000 IU/day (10,11). Higher doses can be sourced as over-the-counter medicines from a pharmacy or when prescribed by a doctor, but are not recommended to be taken regularly.
The significance of increasing the absorption of a low-dose vitamin D supplement also comes from the vast variability in the existing literature, and the inability at times to adequately increase the vitamin D concentrations to the recommended levels. To date, absorption studies have typically supplemented with supramaximal doses well above the recommended weekly intake and have revealed a vast variability in results. Doses of 25,000 to 300,000 IU have been shown to increase peak vitamin D concentrations by as little as 4.8 ng/ml to >100 ng/ml (9,13,14). The highest reported Cmax in the present study (3.8 ng/ml) falls just below the lower level of previously reported concentrations. However, when considering the dosage factor, the present may be considered comparable to the existing literature with regards to the Cmax attained from higher doses.
Peak concentrations from supramaximal doses have also exhibited great variability as regards the time at which they occur, ranging from hours to days. The time to the peak concentration is much more difficult to compare between studies due to the variability in study designs. For example, the present study collected 14 data points over a 72-h period; however, long-term studies tend to collect fewer points over a period of weeks and even months (9), with the focus primarily being on the long-term increase. Therefore, the true Tmax may not have been measured due to the fact that it occurred at a point not measured in the study. Despite this, the present study demonstrated that Tmax occurred at a time equivalent to that reported by other research (14), and later than what might be expected of a low dose of vitamin D.
The Cmax and Tmax of a supplement may not be optimal measurement strategy of the potential therapeutic effects of a vitamin D supplement. Provided blood levels increase sufficiently to reach recommended levels, the time to return to baseline may be a better outcome to consider with vitamin D supplementation. From a single dose, it has been shown that vitamin D levels can return to baseline within hours or can remain elevated for weeks (15-17) and possibly even months. The findings of the present study demonstrated that a single dose effectively elevated vitamin D levels within hours and sustained this elevation for 72 h following a single low dose. While the half-life was unable to be calculated due to the lack of a decline in vitamin D concentrations, the rate of decline between the groups (groups 1, 2 and 3 remained within 6.0, 17.6 and 11.8% of the Cmax values, respectively) suggests that the Food-Grown® formulation may lead to vitamin D concentrations that remain elevated for longer compared with the conventional formulations.
The time a supplement can remain in the blood/body may have a significant impact on the physiological effect achieved. Increased concentrations of vitamin D may allow for increased physiological benefits due to the greater availability for conversion to 1,25-dihydroxyvitamin D. In the present study, while no significant differences were observed between groups, the plasma concentration of vitamin D from the Food-Grown® formulation remained above the conventional formulations for that majority of the study duration (Fig. 1). To help assess this effect, incorporating a greater number of subjects and/or a longer data recording period is required.
One of the few single-dose vitamin D pharmacokinetic studies with a dose administered within the recommended maximum weekly dose was the study by Denker et al (8). Denker et al (8) administered two different vitamin D formulations at either a 2,800 IU or 5,600 IU dose to healthy adults. Following dosing, blood was obtained over an 80- or 120-h period (for 5,600 IU and 2,800 IU doses, respectively) and analysed for total vitamin D concentrations. The analysis revealed the Cmax to be 6.6 and 13.0 ng/ml for the 2,800 and 5,600 IU doses, respectively, with Tmax occurring between 9 and 12 h (8). Denker et al (8) also demonstrated that the serum vitamin D levels had returned to baseline levels within 3 to 4 days of dosing. The results of the study by Denker et al (8) revealed a greater Cmax than that in the present study (Cmax of 2.4 to 3.8 ng/ml); however, the Tmax in the present study occurred at a later stage, and the vitamin D levels remained elevated for the full 72-h study period.
The study by Radicioni et al (14) supplemented healthy participants with 25,000 IU of one of three different vitamin D formulations. Following dosing, blood was obtained for 27 days (648 h) and the peak vitamin D concentrations were observed at 72- to 144-h at a Cmax of 4.8 to 5.3 ng/ml (14). Despite the relatively low Cmax, the plasma vitamin D concentrations remained elevated above baseline levels by 1.2 to 1.5 ng/ml for the full 27-days (14). Although the study by Radicioni et al (14) used doses which were 5-fold higher than those used in the present study, the Cmax did not differ markedly between the studies. However, in the absence of long-term data in the present study, the vitamin D concentrations may have remained elevated for longer periods of time, highlighting the importance of long-term sampling for vitamin D studies.
One factor that may affect the absorption of lipophilic compounds, such as vitamin D is the composition of any food consumed with the supplement. The present study provided participants with a nutritionally balanced breakfast soon after consuming the vitamin D dose. Both the timing and composition of this meal can have an impact on the results of a study and renders the comparison of studies difficult. The study by Raimundo et al (18) supplemented healthy adult participants with 50,000 IU vitamin D followed by either a low- or high-fat meal. At 14 days following supplementation, the high-fat meal increased serum vitamin D levels by approximately 4 ng/ml, whereas the group administered a low-fat meal exhibited a reduction of ~1 ng/ml (18). By contrast, a follow-up study by Raimundo et al (13) demonstrated that the vitamin D concentrations remained elevated for >2 weeks following a single 50,000 IU dose of vitamin D regardless of the food consumed. Healthy 18 to 30-year-old participants were supplemented with 50,000 IU vitamin D before consuming a meal containing no fat, 15 g of fat, or 30 g of fat. Blood was obtained at baseline and on day 14, where it was shown that the vitamin D levels remained elevated above baseline levels by 5.3, 8.6 and 8.6 ng/ml for the groups consuming vitamin D with no fat, and 15 and 30 g of fat in a meal, respectively (13).
In a similar study, Dawson-Hughes et al (15) supplemented participants >50 years of age with 50,000 IU of vitamin D with either no-meal, a high-fat meal or a low-fat meal every 30 days. At 12-h following the consumption of the supplement, the serum vitamin D levels increased by 80, 83 and 96.5 ng/ml for the no-meal, high-fat meal and low-fat meal groups, respectively. At the end of the first 30 days, all vitamin D concentrations increased by ~6 ng/ml and at the end of the 90-day period, the vitamin D concentrations had increased by ~10-12 ng/ml (15) for each group. In a follow-up study, Dawson-Hughes et al (19) supplemented healthy participants >50 years of age with a single 50,000 IU dose of vitamin D (19). The peak plasma vitamin D levels increased by 88 and 116 ng/ml when participants consumed a meal that was fat-free or 30% fat, respectively. However, blood samples were only collected at baseline and at 10, 12 and 14 h post-dosing; thus, the long-term absorption could be established.
The findings from studies conducted by Raimundo et al (13,18) and Dawson-Hughes et al (15,19) highlight the variability in potential absorption, but also the potential impact of food on the absorption of vitamin D. The consumption of high fat foods have been shown to increase the absorption of lipid-based supplements (20). However, due to inconsistencies in results of these studies, particularly for Cmax and Tmax, further research is still required to elucidate the efficacy and optimal dosing regimen of vitamin D.
In a study by by Ilahi et al (16), 30 healthy participants were supplemented with 100,000 IU of vitamin D, and blood samples were collected over a period of 112 days (16). Following supplementation, the serum vitamin D levels increased to a Cmax of 14.9 ng/ml on day 7, declining steadily thereafter; however, the levels remained significantly higher than baseline levels until day 84(16). Similarly, Lark et al (21) administered an equivalent dose of vitamin D to adults with cystic fibrosis and healthy participants resulting in both groups recording Tmax at 24-h post-dosing, with a vitamin D concentration of ~50 and 100 ng/ml for the cystic fibrosis and healthy groups, respectively. By the 36-h post-dosing time point, the serum vitamin D concentrations remained above baseline levels by ~24 and 46 ng/ml for the cystic fibrosis and healthy groups, respectively (21). Overall, Lark et al (21) demonstrated that the participants with cystic fibrosis had approximately half the vitamin D absorption compared to healthy controls. By contrast, von Restorff et al (9) supplemented vitamin D-deficient elderly participants with a single 300,000 IU dose of vitamin D. The serum vitamin D concentrations increased by 26.5 ng/ml from baseline at 3 months (29 patients), remaining at 21.6 ng/ml at 6 months (9). These studies highlight the importance of longitudinal vitamin D studies and the potential for variability of vitamin D absorption. Despite using vitamin D at a dose of 20- and 60-fold to the current study, the studies by Ilahi et al (16) and von Restorff et al (9) demonstrated a a Cmax of ~4- and 7-fold (Cmax of 14.9 and 26.5 ng/ml, respectively) that was observed with the Food-Grown® vitamin D3 formulation (3.8 ngml) in the present study. However, the concentration remained elevated for months. Future studies incorporating low doses of vitamin D would benefit by incorporating regular small doses over a long period of time (months) compared with a large single dose in order to assess the absorption efficacy.
The variations in findings across different studies and populations underscores the imperative, not only to develop highly absorbable vitamin D products, but also to investigate absorption and requirements within specific demographic groups. The observed disparities in study outcomes could stem from several factors. Variations in the absorption of different vitamin D formulations may contribute to this diversity. Since vitamin D needs to undergo emulsification to become water-soluble prior to absorption, certain formulations may exhibit lower emulsification rates than others. Utilising a highly absorbable/easily emulsified formulation could potentially result in higher Cmax levels and in the prolonged elevation of serum vitamin D concentrations. This is the concept behind the Food-Grown® vitamin D3 formulation used herein. By using a formulation that is derived from natural material, the body may better recognize it for use.
Moreover, the food consumed alongside vitamin D supplementation may influence the results. Although the studies by Raimundo et al (18) and Dawson-Hughes et al (19) suggest that high-fat meals generally enhance absorption, there remains some variability in these outcomes. Thus, there may be additional factors beyond merely the composition of food consumed alongside a supplement that affects vitamin D absorption, warranting further investigation.
The demographic composition of participants is another variable and has been observed to influence the absorption of vitamin D. While the precise mechanism behind this phenomenon remains elusive, it likely involves a myriad of factors, such as dietary habits, microbiome composition, body composition and biochemical variability. In the study conducted by Wortsman et al (22), wherein obese and lean adults were supplemented with 50,000 IU vitamin D, it was found that the increase in the serum vitamin D Cmax was notably higher in the lean group compared to the obese group (92 and 72 ng/ml, respectively). Even after 24 h, the serum vitamin D concentrations remained significantly elevated in the lean group.
One potential explanation for this discrepancy may be the storage of vitamin D in adipose tissue. Given that vitamin D is fat-soluble, it may preferentially accumulate in fat stores, resulting in lower serum levels in individuals with higher adiposity. Conversely, individuals with a leaner physique may exhibit increased serum vitamin D levels, as vitamin D could be stored in more metabolically active tissues, such as muscle. Parathyroid hormone (PTH) may also play a role in determining the storage location of vitamin D, as it has been demonstrated to inhibit the uptake of vitamin D into muscle tissue (23). Consistent with this, Wortsman et al (22) reported elevated PTH levels in the obese group compared to the lean group. It is plausible that the rate of vitamin D storage varies among individuals, potentially leading to differences in serum levels despite similar absorption rates.
Although the BMI of the participants in the present study was at a healthy level, the average BMI was at the high end of the normal level, and for group 2, in the low range for what is considered overweight. In addition, although the BMI appeared to have no effect on the comparison of our group data, it may have an effect when making comparisons with other studies that use a leaner or obese group. Future studies could benefit by measuring the lean and fat mass of individuals via body composition analysis. This would allow lean mass to be considered more accurately and warrants further investigation in future studies.
One limitation of the present study was the duration of sample collection. Initially, it was expected that the serum vitamin D concentrations would return to baseline values within 72 h following the single low dose. However, the dose administered was equivalent to 5 days of standard dosing according to local (Australian) standards. Consequently, it would have been insightful to observe whether the concentration remained elevated until the theoretical next dose was administered (i.e., 5 days). In the case that the concentrations persisted above baseline for 5 days, it could result in an accumulation effect from repeated doses, potentially aiding in maintaining elevated serum vitamin D concentrations above the recommended levels. Future studies employing a low dose of vitamin D would benefit from extending the collection period to beyond 5 days as well as conducting long-term (weeks if not months) dosing studies. Since the food-sourced vitamin D formulation exhibited better absorption than the conventional tablet form, it may be feasible to achieve higher Cmax levels and sustain elevated serum vitamin D levels using a Food-Grown® vitamin D3 formulation. Although the present study did not include participants in the obese category, and both groups were well-matched for BMI, future studies could benefit from matching participants for body composition (weight and body fat percentage), thus mitigating body composition as a potential factor influencing the pharmacokinetics of vitamin D.
In conclusion, the results of the present study indicate that a Food-Grown® vitamin D formulation is a potential alternative to current formulation having shown superior absorption to conventional vitamin D tablets and equivalence to a buccal spray. Furthermore, Food-Grown® vitamin D levels remain elevated, near Cmax concentrations, for the duration of the study following dosing.
Acknowledgements
Not applicable.
Funding
Funding: The present study was commercially funded by Wild Nutrition (England).
Availability of data and materials
The data generated in the present study are not publicly available due to commercial interests but may be requested from the corresponding author.
Authors' contributions
DB and AR conceptualized the study. DB and AR were also involved in the investigative aspects of the study, in the study methodology, in project administration, in the provision of resources, study supervision, visualization, and in the writing, review and editing of the manuscript. DB was involved in data validation and in the writing of the original draft. AR was involved in data curation and in the formal analysis, as well as in funding acquisition. DB and AR confirm the authenticity of all the raw data. Both authors have read and approved the final manuscript.
Ethics approval and consent to participate
The present study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Bellberry Limited (approval nos 2022-06-607 on 08-08-2022). All participants provided written informed consent prior to inclusion in the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
|
Pludowski P, Takacs I, Boyanov M, Belaya Z, Diaconu CC, Mokhort T, Zherdova N, Rasa I, Payer J and Pilz S: Clinical practice in the prevention, diagnosis and treatment of vitamin D deficiency: A Central and Eastern European expert consensus statement. Nutrients. 14(1483)2022.PubMed/NCBI View Article : Google Scholar | |
|
Kennel KA, Drake MT and Hurley DL: Vitamin D deficiency in adults: When to test and how to treat. Mayo Clin Proc. 85:752–758. 2010.PubMed/NCBI View Article : Google Scholar | |
|
Palacios C and Gonzalez L: Is vitamin D deficiency a major global public health problem? J Steroid Biochem Mol Biol. 144:138–145. 2014.PubMed/NCBI View Article : Google Scholar | |
|
Pfotenhauer KM and Shubrook JH: Vitamin D deficiency, its role in health and disease, and current supplementation recommendations. J Am Osteopath Assoc. 117:301–305. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Itkonen ST, Erkkola M and Lamberg-Allardt CJE: Vitamin D fortification of fluid milk products and their contribution to vitamin D intake and vitamin D status in observational studies-a review. Nutrients. 10(1054)2018.PubMed/NCBI View Article : Google Scholar | |
|
Pellegrino L, Marangoni F, Muscigiuri G, D'Incecco P, Duval GT, Annweiler C and Colao A: Vitamin D fortification of consumption cow's milk: Health, nutritional and technological aspects. A multidisciplinary lecture of the recent scientific evidence. Molecules. 26(5289)2021.PubMed/NCBI View Article : Google Scholar | |
|
Tippetts M, Martini S, Brothersen C and McMahon DJ: Fortification of cheese with vitamin D3 using dairy protein emulsions as delivery systems. J Dairy Sci. 95:4768–4774. 2012.PubMed/NCBI View Article : Google Scholar | |
|
Denker AE, Lazarus N, Porras A, Ramakrishnan R, Constanzer M, Scott BB, Chavez-Eng C, Woolf E, Maganti L, Larson P, et al: Bioavailability of alendronate and vitamin D3 in an alendronate/vitamin D3 combination tablet. J Clin Pharmacol. 51:1439–1448. 2011.PubMed/NCBI View Article : Google Scholar | |
|
von Restorff C, Bischoff-Ferrari HA and Theiler R: High-dose oral vitamin D3 supplementation in rheumatology patients with severe vitamin D3 deficiency. Bone. 45:747–749. 2009.PubMed/NCBI View Article : Google Scholar | |
|
Ross AC, Taylor CL, Yaktine AL and Del Valle HB: Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium. National Academies Press, Washington, DC, pp1-1115, 2011. | |
|
Australian Government, Department of Health and Aged Care: Vitamin D. Australian Government, Woden, ACT 2606, 2017. https://www.tga.gov.au/resources/publication/scheduling-decisions-interim/scheduling-delegates-interim-decisions-and-invitation-further-comment-accsacms-november-2016/31-vitamin-d#:~:text=Vitamin%20D%20has%20low%20toxicity,is%20very%20difficult%20to%20overdose. Accessed January 2024. | |
|
Marwaha RM and Dabas A: Bioavailability of nanoemulsion formulations vs conventional fat soluble preparations of cholecalciferol (D3)-an overview. J Clin Orthop Trauma. 10:1094–1096. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Raimundo FV, Lang MAB, Scopel L, Marcondes NA, Araújo MG, Faulhaber GA and Furlanetto TW: Effect of fat on serum 25-hydroxyvitamin D levels after a single oral dose of vitamin D in young healthy adults: A double-blind randomized placebo-controlled study. Eur J Nutr. 54:391–396. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Radicioni M, Caverzasio C, Rovati S, Giori AM, Cupone I, Marra F and Mautone G: Comparative bioavailability study of a new vitamin D3 orodispersible film versus a marketed oral solution in healthy volunteers. Clin Drug Investig. 42:151–161. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Dawson-Hughes B, Harris SS, Palermo NJ, Ceglia L and Rasmussen H: Meal conditions affect the absorption of supplemental vitamin D3 but not the plasma 25-hydroxyvitamin D response to supplementation. J Bone Miner Res. 28:1778–1783. 2013.PubMed/NCBI View Article : Google Scholar | |
|
Ilahi M, Armas LAG and Heaney RP: Pharmacokinetics of a single, large dose of cholecalciferol. Am J Clin Nutr. 87:688–691. 2008.PubMed/NCBI View Article : Google Scholar | |
|
Roth DE, Mahmid AA, Raqib R, Black RE and Baqui AH: Pharmacokinetics of a single oral dose of vitamin D3 (70,000 IU) in pregnant and non-pregnant women. Nutr J. 11(114)2012.PubMed/NCBI View Article : Google Scholar | |
|
Raimundo FV, Faulhaber GAM, Menegatti PK, da Silva ML and Furlanetto TW: Effect of high-versus low-fat meal on serum 25-hydroxyvitamin D levels after a single oral dose of vitamin D: A single-blind, parallel, randomized trial. Int J Endocrinol. 2011(809069)2011.PubMed/NCBI View Article : Google Scholar | |
|
Dawson-Hughes B, Harris SS, Lichtenstein AH, Dolnikowski G, Palermo NJ and Rasmussen H: Dietary fat increases vitamin D-3 absorption. J Acad Nutr Diet. 115:225–230. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Chuang J, Briskey D, Dang J, Rajgopal A and Rao A: A randomized double-blind trial to measure the absorption characteristics of eicosapentaenoic acid and docosahexaenoic acid rich oil blend with natural lipid-based delivery system. Food Sci Biotech. 33:1957–1964. 2023.PubMed/NCBI View Article : Google Scholar | |
|
Lark RK, Lester GE, Ontjes DA, Blackwood AD, Hollis BW, Hensler MM and Aris RM: Diminished and erratic absorption of ergocalciferol in adult cystic fibrosis patients. Am J Clin Nutr. 73:602–606. 2001.PubMed/NCBI View Article : Google Scholar | |
|
Wortsman J, Matsuoka LY, Chen TC, Lu Z and Holick MF: Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 72:690–693. 2000.PubMed/NCBI View Article : Google Scholar | |
|
Abboud M, Rybchyn MS, Liu J, Ning Y, Gordon-Thomson C, Brennan-Speranza TC, Cole L, Greenfield H, Fraser DR and Mason RS: The effect of parathyroid hormone on the uptake and retention of 25-hydroxyvitamin D in skeletal muscle cells. J Steroid Biochem Mol Biol. 173:173–179. 2017.PubMed/NCBI View Article : Google Scholar |