Clinical efficacy of laparoscopic surgery used for the excision of villus tissue and the repair of uterine scar in patients with cesarean scar pregnancy‑II
- Authors:
- Published online on: July 26, 2022 https://doi.org/10.3892/mi.2022.48
- Article Number: 23
-
Copyright: © Li et al. This is an open access article distributed under the terms of Creative Commons Attribution License.
Abstract
Introduction
Although cesarean scar pregnancy (CSP) is considerably infrequent among patients with ectopic pregnancy, in which the gestational sac (GS) is implanted into the myometrium at the place of a previous cesarean section scar, it is one of the most dangerous long-term complications following cesarean section (1,2). The approximate incidence of CSP ranges from 1/1,800 to 1/2,200 and the percentage of ectopic pregnancies among women with a history of cesarean section accounts to 6.1% and has exhibited an increasing tendency (3,4).
CSP has been classified as two different pathophysiological types by Vial et al (5). The first type (CSP-I) exhibits a certain success rate of viable birth, although the amniotic sac implants into the previous cesarean section. The amniotic sac grows towards the cervico-isthmic space and the uterine cavity with the progression of pregnancy. A high risk of massive bleeding is possible due to the placenta previa and placenta accrete (5,6). The second type of CSP (CSP-II) is associated with a high risk of bleeding and uterine rupture, in which the GS is deeply implanted into the myometrium with the progression of pregnancy (5,6). However, the CSP has been classified into three types according to the association between the GS and uterine incision scar in 2016 in the Expert opinion of Diagnosis and Treatment of Cesarean Scar Pregnancy (7).
At present, to the best of our knowledge, there are no unified standards available for the diagnosis and treatment of CSP. The available treatments mainly include drug therapy, surgery, uterine artery embolization, high-intensity focused ultrasound (HIFU) ablation and combined therapy. At present, the removal of the pregnancy tissue by surgery is the mainstay treatment.
Patients and methods
General patient information
The clinical data of 25 patients receiving timely treatment with laparoscopic surgery at the Department of Gynecology at Zheng Zhou Yi He Hospital (Zhengzhou, China) were collected between January, 2017 and October, 2020. In addition, a total of 23 patients treated with suction curettage in operative hysteroscopy were followed-up for 6 months. The following selection criteria were used: i) A history of cesarean section delivery; ii) early clinical manifestations of pregnancy; iii) a diagnosis of CSP determined by ultrasound or confirmed by magnetic resonance imaging (MRI) according to the recommended diagnostic criteria (8,9); iv) stable vital signs and the desire to retain the uterus; v) a gestational age <70 days. The clinical data of the patients who received laparoscopic surgery are presented in Tables I and II. The patients were 22-40 years of age. A total of 18 patients had one previous cesarean delivery and 7 patients had two previous cesarean deliveries. All these operations were classified as lower uterine segment transverse incisions. The missed menses of all patients ranged from 35 to 70 days. According to the patient's condition, the surgical method was explained to them, followed by a comprehensive discussion between the patient and the surgeon explaining the pros and cons of the surgical strategy. The patients then signed a surgery consent form as routine clinical practice. The research protocol was approved by the Ethics Committee of Zheng Zhou Yi He Hospital. The informed consent to participate was waived off due to the retrospective nature of the study.
The following clinical findings were observed: i) A total of 15 patients had a history of cesarean section and menolipsis; ii) all patients presented with irregular vaginal bleeding ranging from 3 to 30 days; iii) a total of 6 patients (patients 2, 7, 11, 15, 20, and 23) had received prior curettage or medical treatment in local hospitals 2 weeks to 1 month prior. Patient 15 who was diagnosed with CSP in the local hospitals was initially treated with 150 mg mifepristone, which was received orally and with 600 µg misoprostol. After 1 week, the patient received 50 mg methotrexate (MTX) intramuscularly as the first treatment was not effective. Patients 2, 7, 20, and 23 had received prior curettage. The levels of β-human chorionic gonadotropin (β-HCG) were not reduced and the GS was still present as monitored by ultrasonography. Patient 11 developed heavy bleeding due to the blind curettage and was transferred immediately to our hospital. The other 23 patients were diagnosed by ultrasound and received suction curettage under hysteroscopy due to their relatively stable conditions.
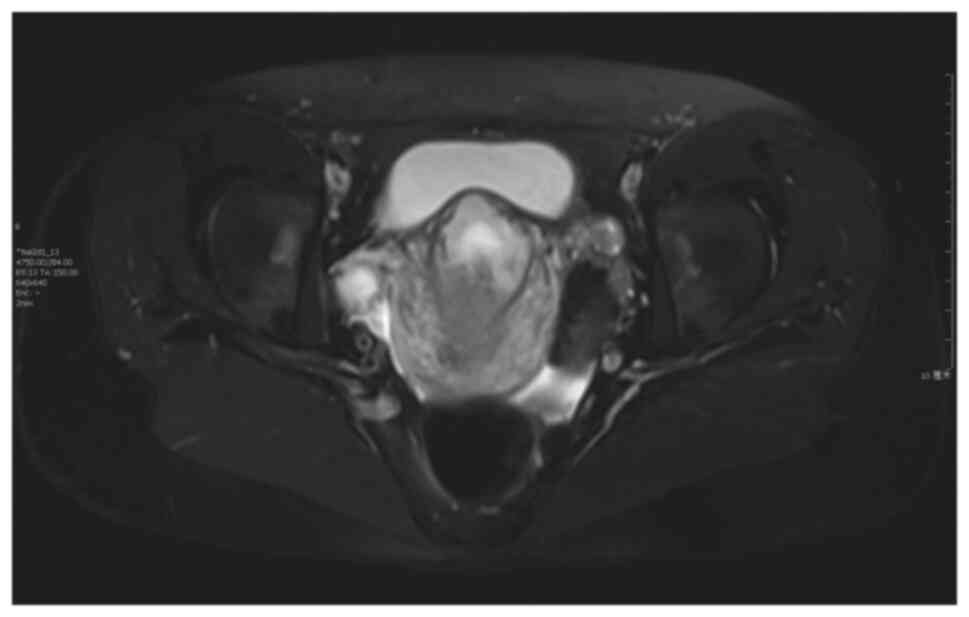
The following laboratory findings and specific examinations were performed: i) The levels of β-HCG were assessed prior to surgery, and ranged between 892 and 84059.9 IU/l; ii) the characteristic ultrasound was an empty uterus and empty cervical canal; iii) the MRI data of patients 1, 5, 12 and 14 were all indicative of prompt GS, which was convex to the bladder.
Treatment
A total of 25 patients with CSP-II diagnosed by ultrasound or MRI underwent laparoscopic surgery resection of the scar with gestational tissue and wound repair to preserve the uterus. The blood loss during the surgery was estimated to be 50-1,000 ml. The range of β-HCG concentration from the 3rd to the 4th day following surgery was reduced to 38-6,674 IU/l.
Pathological diagnosis identified as placenta and villus
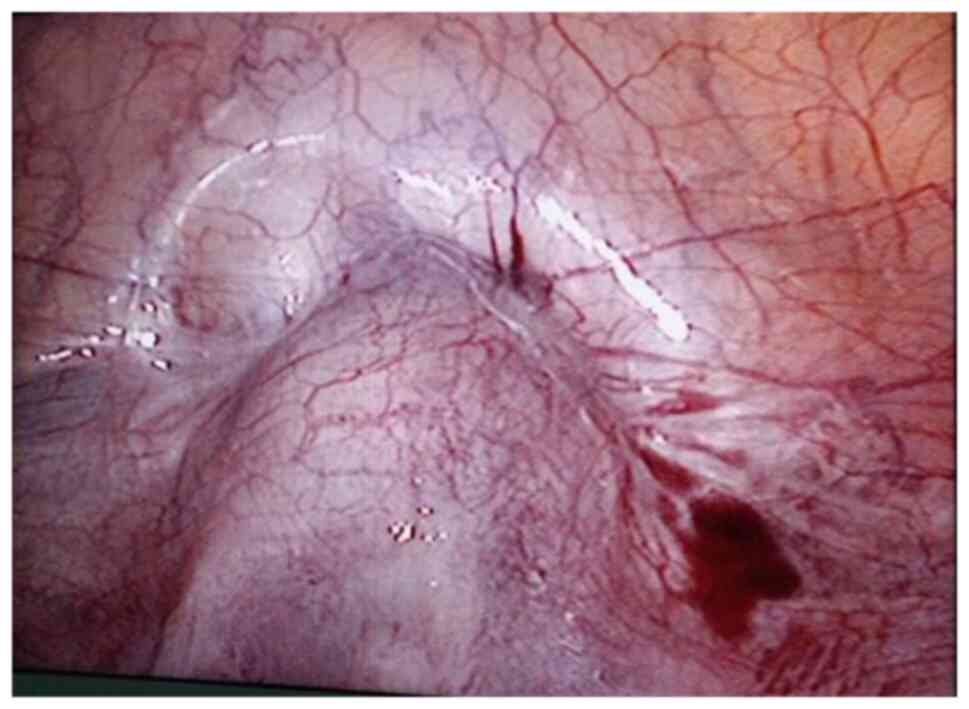
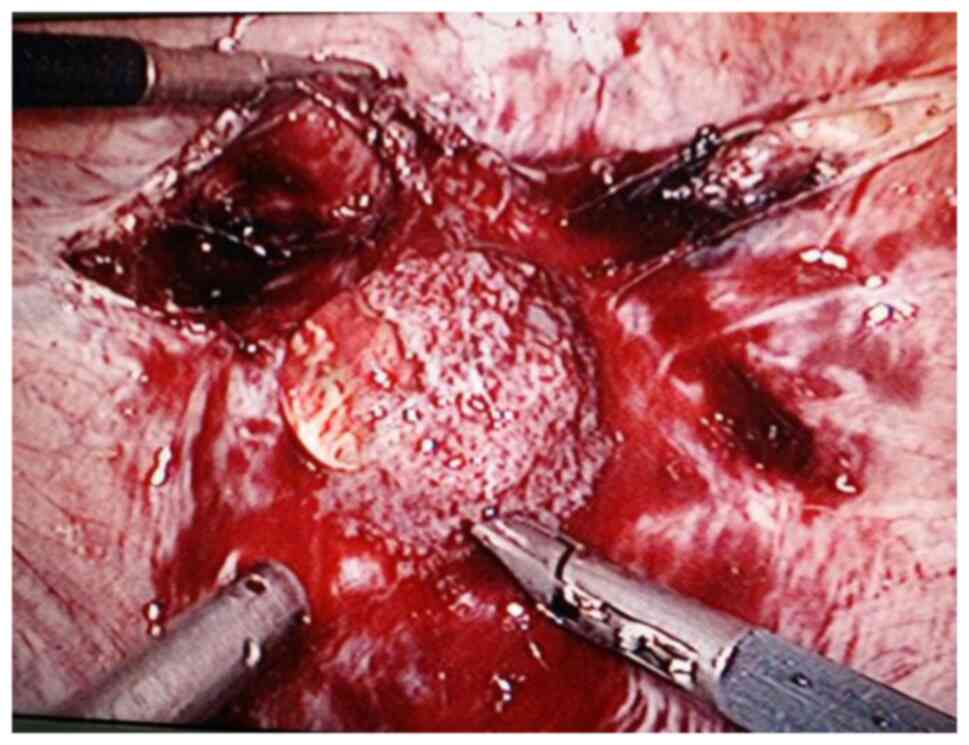
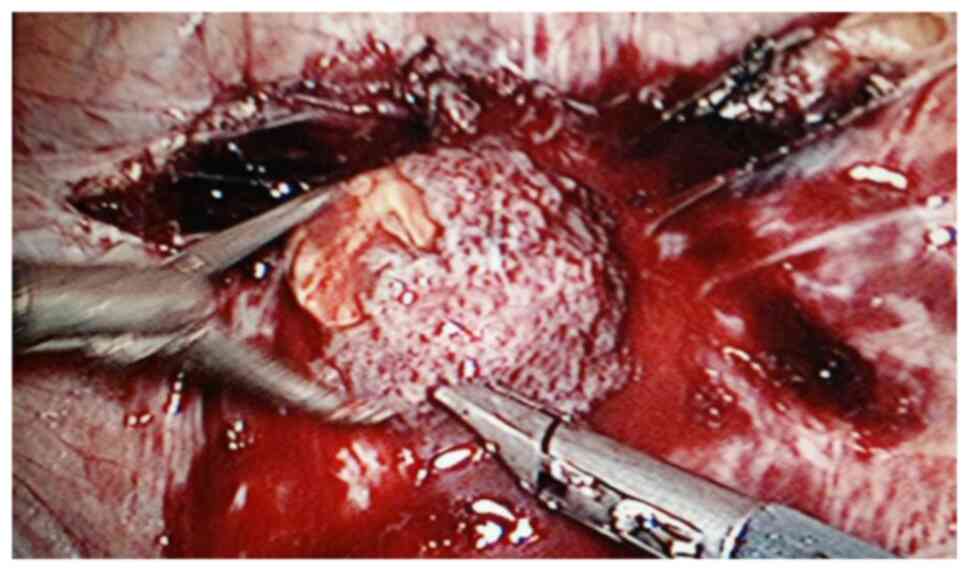
The surgical procedure was as follows: Laparoscopy was performed under general anesthesia in the supine lithotomy position. Laparoscopy displayed a bulging in the lower uterine segment (Fig. 1). Subsequently, a 12 IU vasopressin solution was injected into the uterus. The bladder peritoneum was incised to expose the pregnancy scar; a bulging was noted comprised of blood vessels and gestational tissues. The gestational tissue was rapidly removed with grasping forceps, scissors and an aspirator (Figs. 2 and 3). This procedure was performed as quickly as possible. The myometrial scar was resected and stanched by bipolar coagulation. Finaly, a continuous suture with an absorbable suture (1-0) was used to close the uterine wound (Fig. 4).
A total of 23 patients in the hysteroscopy group underwent hysteroscopic removal of the pregnancy tissues and MTX (50 mg/m2) was administered during surgery. A total of 4 of these patients did not agree to laparoscopic surgical treatment. Uterine arterial embolization (UAE) was used as a pre-treatment to reduce the risk of intraoperative bleeding.
Evaluation of therapeutic effects
The clinical effects of the two protocols were determined based on the evaluation of the following indices: Bleeding, recovery with preserve fertility, the absence of repeated surgical intervention or embolization and the lack of any severe complication. Serum β-HCG levels were measured every 3 to 7 days following treatment until complete recovery. A transvaginal ultrasound was performed every 4 weeks to evaluate the condition of residual lesion and the thickness of the uterine scar.
Statistical analysis
The data were analyzed with SPSS 20.0 software (IBM Corp.). The continuous data with a normal distribution are presented as the mean ± standard deviation. Comparisons between the two groups were analyzed using an unpaired t-test for continuous variables. The significant level (a) was set at 0.05 and a P-value <0.05 was considered to indicate a statistically significant difference.
Results
No significant differences were noted between the two groups as regards baseline characteristics, age, time from last menstruation, the average diameter of the gestation sac, the number of cesarean sections, the period of bleeding and initial human chorionic gonadotropin (HCG) concentrations (all P>0.05, Table III).
All 25 laparoscopy procedures were successful, preserving the uterus without conversion to open laparotomy. The pathological diagnosis was placenta and villus. Following a follow-up period of 6 months, no apparent abnormalities were reported. The time required for the β-HCG levels to reach a normal level ranged from 2 to 4 weeks. The operation time ranged from 60 to 120 min. Intraoperative hemorrhage ranged from 50 to 1,000 ml.
The comparison between the laparoscopy and hysteroscopy groups revealed statistically significant differences (P<0.05, Table IV) as regards the post-operative expression of HCG, the time required for HCG to return to normal levels, the post-operative thickness of the uterine scar and the menstruation recovery time. However, no significant differences were noted in blood loss during the surgery (P>0.05). A total of 4 patients in the hysteroscopy group were treated with UAE to reduce the risk of intraoperative bleeding. The surgery was successfully completed in all patients without any surgical complications, such as hemorrhage. However, 2 patients had residual lesions and 1 patient underwent laparoscopic surgery.
Discussion
CSP is a relatively infrequent type of ectopic pregnancy. The cesarean section infiltrate grows into the myometrium and even penetrates the uterine wall; therefore, in early pregnancy, it can cause uterine hemorrhage, perforation and even rupture. Due to its anatomy and pathology, it often causes uncontrolled bleeding for the blind curettage and may require hysterectomy, and endanger the lives of the patients. Therefore, early detection and timely treatment are instrumental to preserve fertility and avoid severe disease complications.
The imaging criteria for diagnosis (Figs. 5 and 6; patient 5) include the following: An empty uterus and cervical canal; the development of the GS toward the anterior wall of the isthmic portion; the loss of myometrial anterior wall continuity on a sagittal plane of the uterus through the GS; the absence of or diminished healthy myometrium between the bladder and the sac; the monitoring of peri-trophoblastic vascular flow with high velocity and low impedance surrounded by the sac using Doppler examination (10,11). The pathological features included trophoblast invasion and destructive growth to the uterine wall. Since the opened blood vessels do not possess systolic function and the scar tissue cannot contract, a potential misdiagnosis leading to an artificial or spontaneous abortion will result in massive hemorrhage (12).
The therapeutic strategies for CSP include drug therapy, laparotomy surgery resection of gestational tissue, hysteroscopic treatment, laparoscopic management, uterine artery drug infusion and embolization, the transvaginal resection of gestational nidus and repeated HIFU ablation.
The drugs used include mifepristone, MTX and Radix trichosanthis. These can be used alone or in combination. MTX and mifepristone are the main drugs of conservative treatment for ectopic pregnancy. They are mainly suitable for patients at an early gestational age, with a stable condition, reduced bleeding and small lesions. Furthermore, this type of treatment requires a prolonged follow-up period (the HCG levels require a maximum duration of 4 months to return to normal) (13).
Traditional laparotomy for the resection of the lesion is mainly used in patients with critical condition and severe bleeding. This type of treatment is associated with various advantages, such as the ability to directly investigate straight lesions and remove the nidus thoroughly. Patients with barren requirements can have their scars directly resected with the gestational tissue; however, the extent of trauma is greater. It has been reported that open surgery is the optimal treatment option for CSP, since it may be able to reduce the risk of recurrence of this condition (14).
Hysteroscopic treatment has become the primary means of diagnosis and treatment for CSP since the first report of successful hysteroscopy to treat resection in 2005. Wang et al (12) indicated that hysteroscopy could clearly distinguish the GS and implantation area of the vascular distribution in the embryonic sac and could be used to guide or direct treatment. It may be an effective method for the treatment of CSP. Moreover, it has the advantages of a shorter operation time, reduced bleeding, rapid recovery, a shorter hospitalization time, lower costs and the preservation of the uterus. The typical patient with CSP-II may experience the risk of hemorrhage and consequently the treatment is changed to laparotomy or laparoscopic surgery.
Uterine artery chemoembolization is a hotspot investigated in recent years for the treatment of CSP; its advantages are the following: Firstly, focal perfusion MTX may hinder the growth of trophoblast cells and lead to the inhibition of embryonic growth; the increase in the local drug concentration can terminate the bleeding of the bilateral uterine artery caused by embolization, reduce the risk of peri-operative bleeding due to curettage, allow the absorption of the thrombus following vascular embolization, and post-operatively recover the unobstructed uterine artery. The most important advantage is that the uterine functions are not affected. UAE is often used as a pre-treatment.
Kang et al (15) first reported a case of CSP treated successfully with transvaginal resection of the gestational nidus in 2011. Due to its reduced complications, rapid post-operative recovery and smaller trauma, gradually, it is widely used in clinical practice, although it includes the shortcomings of a small surgical field and difficult exposure.
The resection of the gestational tissue and repair scar by laparoscopic surgery is suitable for the GS deep implantation toward the myometrium and bulging from the uterine serosal surface to abdominal cavity and bladder. Lee et al (3) first reported a case of CSP successfully treated with laparoscopy in 1999. Laparoscopic surgery provides greater security; in the case of intraoperative bleeding, the patient can undergo bilateral uterine artery ligation; however, this requires advanced technology. The significant risks of CSP-II include severe bleeding, perforation and rupture. During the blind curettage used for the misdiagnosis of normal pregnancy, massive hemorrhage and uterine rupture can occur, leading to an emergency hysterectomy, which can endanger the lives of the patients. Therefore, surgery should be the first choice for patients with CSP-II. In the present study, all 25 operations were successfully performed using laparoscopy with the surgical resection of the gestational tissue and wound repair to preserve fertility without conversion to open laparotomy. The key point during the operation is to avoid injury to the bladder and ureter following the separation of the bladder from the lower uterine segment. Furthermore, the GS and uterine scar are completely excised as much as possible (16). In the present study, patients 1, 2, 8, 13 and 25 demonstrated a heavy blood loss of almost 1,000 ml during the resection of the scar with the gestational tissue. This was due to long-term bleeding following the last menstruation (~1 month). A high amount of necrotic tissue and obsolete hematoceles were observed in the GS; therefore, a longer time would be required to resect the GS. Furthermore, the operation included a limited time period to undergo bilateral uterine artery ligation and reduce bleeding. Patients 6, 12, 14 and 23 were administered bilateral uterine artery ligation prior to the resection of the scar, since the gestational mass size was >3 cm. Furthermore, the bleeding time of these 4 patients was >20 days. The blood loss during the surgery of these 4 patients was markedly lower than that noted in patients 1, 2, 8, 13 and 25. Therefore, the therapeutic approach to excise the uterine scar and repair the uterine wound would depend on the size of the gestational mass indicated by the ultrasound or the MRI scan. However, considering the dense pre-operative adhesion formation, the selection of transvaginal resection of the gestational nidus may be optimal. This is due to the difficulty in separating the bladder from the lower uterine segment and the possibility to damage the bladder during laparoscopcy.
In conclusion, to reduce the incidence rate of CSP, particular attention should be paid to examine the indication for cesarean section in primiparae (17). The optimal therapeutic strategy for CSP needs to ensure early detection and early treatment to reduce bleeding and avoid the possibility of hysterectomy. Following the diagnosis of CSP, the appropriate treatment needs to be selected by clinicians according to the different types of patients, which includes drug therapy, interventional therapy, surgical or combined therapy. According to the results of the present study, which included 25 patients, and the results reported by similar research (18), laparoscopy is an effective surgical method with limited associated trauma; it is also a safe procedure devoid of complications and an efficient method with which to completely remove the pregnancy tissue in a hysteroscopic manner combined with laparoscopic surgery and the reversible ligation of the uterine artery (18). The resection of the scar with the gestational tissue and the wound repair caused by laparoscopy is considered an effective method for the treatment of CSP-II. It can remove the nidus directly and perform bilateral uterine artery ligation to reduce bleeding; moreover, it removes the old scar and can also increase the success rate of secondary pregnancy. Currently, to the best of our knowledge, only a limited number of reports have been published on the recurrence of laparoscopic management for CSP-II, which may minimize the recurrent risk of CSP through the resection of the old scar and may facilitate the new wound repair by laparoscopy. However, the long-term complications and safety require additional research studies and follow-up observations.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
XML and LY provided the original idea for the study and contributed to the design of the experiments. XML and NNW conducted the experiments and collected the data. XML and XFX analyzed the data and prepared the original draft of the manuscript. LY and XFX confirm the authenticity of all the raw data. All authors contributed to the interpretation and/or discussion of the results, leading to the final version of the manuscript, and all authors have read and approved the final manuscript.
Ethics approval and consent to participate
The research protocol was approved by the Ethics Committee of Zheng Zhou Yi He Hospital. The patients signed a surgery consent form as routine clinical practice. The informed consent to participate was waived off due to the retrospective nature of the study.
Patient consent for publication
The patients provided written informed consent for their data to be published.
Competing interests
The authors declare that they have no competing interests.
References
|
Herman A, Weinraub Z, Avrech O, Maymon R, Ron-El R and Bukovsky Y: Follow up and outcome of isthmic pregnancy located in a previous caesarean section scar. Br J Obstet Gynaecol. 102:839–841. 1995.PubMed/NCBI View Article : Google Scholar | |
|
Seow KM, Hwang JL, Tsai YL, Huang LW, Lin YH and Hsieh BC: Subsequent pregnancy outcome after conservative treatment of a previous cesarean scar pregnancy. Acta Obstet Gynecol Scand. 83:1167–1172. 2004.PubMed/NCBI View Article : Google Scholar | |
|
Lee CL, Wang CJ, Chao A, Yen CF and Soong YK: Laparoscopic management of an ectopic pregnancy in a previous caesarean section scar. Hum Reprod. 14:1234–1236. 1999.PubMed/NCBI View Article : Google Scholar | |
|
Rotas MA, Haberman S and Levgur M: Cesarean scar ectopic pregnancies: Etiology, diagnosis, and management. Obstet Gynecol. 107:1373–1381. 2006.PubMed/NCBI View Article : Google Scholar | |
|
Vial Y, Petignat P and Hohlfeld P: Pregnancy in a cesarean scar. Ultrasound Obstet Gynecol. 16:592–593. 2000.PubMed/NCBI View Article : Google Scholar | |
|
Gurol-Urganci I, Bou-Antoun S, Lim CP, Cromwell DA, Mahmood TA, Templeton A and van der Meulen JH: Impact of Caesarean section on subsequent fertility: A systematic review and meta-analysis. Hum Reprod. 28:1943–1952. 2013.PubMed/NCBI View Article : Google Scholar | |
|
Family Planning Subgroup, Chinese Society of Obstetrics and Gynocology, Chinese Medical Association. Expert opinion of diagnosis and treatment of cesarean scar pregnancy (2016). Zhonghua Fu Chan Ke Za Zhi. 51:568–572. 2016.PubMed/NCBI View Article : Google Scholar : (In Chinese). | |
|
Timor-Tritsch IE, Monteagudo A, Cali G, Vintzileos A, Viscarello R, Al-Khan A, Zamudio S, Mayberry P, Cordoba MM and Dar P: Cesarean scar pregnancy is a precursor of morbidly adherent placenta. Ultrasound Obstet Gynecol. 44:346–353. 2014.PubMed/NCBI View Article : Google Scholar | |
|
Timor-Tritsch IE, Monteagudo A, Cali G, El Refaey H, Kaelin Agten A and Arslan AA: Easy sonographic differential diagnosis between intrauterine pregnancy and cesarean delivery scar pregnancy in the early first trimester. Am J Obstet Gynecol. 215:225.e1–7. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Fylstra DL: Ectopic pregnancy within a caesarean scar: A review. Obstet Gynecol Surv. 57:537–543. 2002.PubMed/NCBI View Article : Google Scholar | |
|
Jurkovic D, Hillaby K, Woelfer B, Lawrence A, Salim R and Elson CJ: First-trimester diagnosis and management of pregnancies implanted into the lower uterine segment Cesarean section scar. Ultrasound Obstet Gynecol. 21:220–227. 2003.PubMed/NCBI View Article : Google Scholar | |
|
Wang YL, Su TH and Chen HS: Laparoscopic management of an ectopic pregnancy in a lower segment cesarean section scar: A review and case report. J Minim Invasive Gynecol. 12:73–79. 2005.PubMed/NCBI View Article : Google Scholar | |
|
Doubilet PM, Benson CB, Frates MC and Ginsburg E: Sonographically guided minimally invasive treatment of unusual ectopic pregnancies. J Ultrasound Med. 23:359–370. 2004.PubMed/NCBI View Article : Google Scholar | |
|
Fylstra DL, Pound-Chang T, Miller MG, Cooper A and Miller KM: Ectopic pregnancy within a cesarean delivery scar: A case report. Am J Obstet Gynecol. 187:302–304. 2002.PubMed/NCBI View Article : Google Scholar | |
|
Kang SY, Park BJ, Kim YW and Ro DY: Surgical management of caesarean scar ectopic pregnancy: Hysterectomy by transvaginal approach. Fertil Steril. 96:E25–E28. 2011.PubMed/NCBI View Article : Google Scholar | |
|
Wang HY, Zhang J, Li YN, Wei W, Zhang DW, Lu YQ and Zhang HF: Laparoscopic management or laparoscopy combined with transvaginal management of type II cesarean scar pregnancy. JSLS. 17:263–272. 2013.PubMed/NCBI View Article : Google Scholar | |
|
Delbaere I, Cammu H, Martens E, Tency I, Martens G and Temmerman M: Limiting the caesarean section rate in low risk pregnancies is key to lowering the trend of increased abdominal deliveries: An observational study. BMC Pregnancy Childbirth. 12(3)2012.PubMed/NCBI View Article : Google Scholar | |
|
Huang L, Zhao L and Shi H: Clinical efficacy of combined hysteroscopic and laparoscopic surgery and reversible ligation of the uterine artery for excision and repair of uterine scar in patients with type II and III cesarean scar pregnancy. Med Sci Monit. 26(e924076)2020.PubMed/NCBI View Article : Google Scholar |