Prognostic analysis of systemic antitumor therapy in young patients with advanced liver cancer: A cohort study
- Authors:
- Published online on: June 28, 2024 https://doi.org/10.3892/ol.2024.14544
- Article Number: 410
-
Copyright: © Zhang et al. This is an open access article distributed under the terms of Creative Commons Attribution License.
Abstract
Introduction
Primary liver cancer (PLC) is one of the most common malignant tumors worldwide. According to the International Cancer Research Institute affiliated to the World Health Organization (1), an estimated 906,000 new cases of liver cancer and 830,000 deaths due to liver cancer are reported each year. Hepatocellular carcinoma (HCC) accounts for 85–90% of all cases of PLC. In China, the main cause of HCC is chronic hepatitis B virus (HBV) infection (2). PLC often occurs in people aged >55 years. However, China and other East Asian countries have a relatively higher prevalence of chronic HBV infection in young people (age ≤18 years) due to the mother-to-child transmission (3,4).
Young patients (age ≤35 years) with cancer differ from elderly patients (>35 years) with respect to disease pathogenesis, treatment and prognosis (5). Previous studies have demonstrated the impact of age at tumor occurrence on the prognosis of gastric, breast and colorectal cancer (6–9). Most patients with HCC are diagnosed at an advanced stage and have lost the opportunity for radical surgery. In addition, patients with early liver cancer are prone to recurrence and metastasis after liver cancer resection and transplantation due to the background of HBV infection (10). Currently, systemic antitumor therapy, including chemotherapy, targeted therapy, immunotherapy and liver protection therapy, is the main treatment method for patients with advanced liver cancer (11).
As PLC in young patients is often associated with the mother-to-child transmission of HBV, it is characterized by rapid disease progression and poor therapeutic efficacy (12,13). There is a paucity of research on the treatment of young patients with liver cancer, and the systemic antitumor therapy of this population has not been well characterized separately. The present study aimed to perform an in-depth analysis of the differences in the efficacy of systemic antitumor therapy in young patients with liver cancer. The findings may provide a clinical treatment reference for this group of patients.
Patients and methods
Research object
The present study was a retrospective cohort study of young patients with liver cancer (≤35 years old) who received systemic antitumor therapy at the Nanjing Jinling Hospital (Nanjing, China) between May 2015 and May 2023. These patients were designated as group A. Elderly patients (≥55 years old) with liver cancer were enrolled as the control group and designated as group B. This study conforms to the ethical principles of the Declaration of Helsinki (2013). Ethical approval was provided by the Ethics Committee of Jinling Hospital (approval no. DZQH-KYLL-23-16).
The required sample size for this study was estimated based on the cohort study design, and the comparison of survival time (OS) between young patients and elderly patients with liver cancer. Considering the low incidence of liver cancer in young patients, patients in group A and group B were enrolled at a ratio of 1:2, and the estimated HR was 2.0 (group A vs. group B). An 80% incidence of end-point events, α=0.05 and β=0.20 were factored in. Based on the simulation under the aforementioned assumptions, at least 31 subjects in group A and 62 subjects in group B were required, and 80% of patient deaths were observed after follow-up. Considering the loss of follow-up and incomplete data collection, 38 subjects were finally included in group A and 79 subjects in group B.
Inclusion and exclusion criteria
The inclusion criteria were as follows: i) A pathological diagnosis of HCC or a clinical diagnosis of PLC; ii) received systemic antitumor therapy; iii) no opportunity for radical surgery; iv) age ≤35 years or ≥55 years; and v) provision of informed consent.
The exclusion criteria were as follows: i) Pathologically confirmed other types of liver cancer, such as intrahepatic cholangiocarcinoma or mixed liver cancer; ii) no systemic drug treatment; and c) patients with a poor general condition and short expected survival time.
The main research population in this study consisted of patients with advanced liver cancer, which is defined as patients whose advanced condition is not suitable for radical surgery and/or local regional therapy (LRT), or patients whose condition has progressed after surgery and/or LRT. The following systemic drug therapies were used in the patients with advanced liver cancer included in this study: 400 mg oral sorafenib twice a day; 12 mg/day oral lenvatinib for a bodyweight of >60 kg or 8 mg/day oral lenvatinib for a bodyweight of <60 kg; 200 mg oral donafenib twice a day; 240 mg intravenous nivolumab once every 2 weeks; 1,200 mg intravenous atezolizumab + 15 mg/kg intravenous bevacizumab once every 3 weeks; 200 mg intravenous tislelizumab once every 3 weeks; and 130 mg/m2 intravenous oxaliplatin + 200 mg/m2 intravenous leucovorin + 400 mg/m2 intravenous 5-fluorouracil once every 3 weeks. Based on the systematic drug therapies in this study, follow-up subgroup analysis was made, including tyrosine kinase inhibitors (TKIs), immune checkpoint inhibitors (ICIs), chemotherapy and the combination of the two treatments.
Data collection
A total of 117 patients entered the final analysis set (Fig. 1). Baseline demographic data and clinical data, such as age, sex, medical record number, contact information and history of liver disease were collected from the hospital medical records. Baseline liver function indices such as serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), total bilirubin (TBIL), Child-Pugh score (14), and α-fetoprotein (AFP) were collected. The indicators of HBV infection were recorded, including HBV surface antigen (HBsAg), HBV surface antibody (HBsAb), HBeAg, HBeAb, HBcAb and HBV DNA. Certain indicators related to liver cancer were collected in the hospital medical record system, namely, whether previous surgery, presence of portal vein tumor thrombus (PVTT) and tumor stage (Barcelona Clinic Liver Cancer) (15). Follow-up information regarding treatment strategy and survival outcomes was also collected. Finally, patients with advanced liver cancer were divided into the young group (group A) and the elderly group (group B).
Survival follow-up
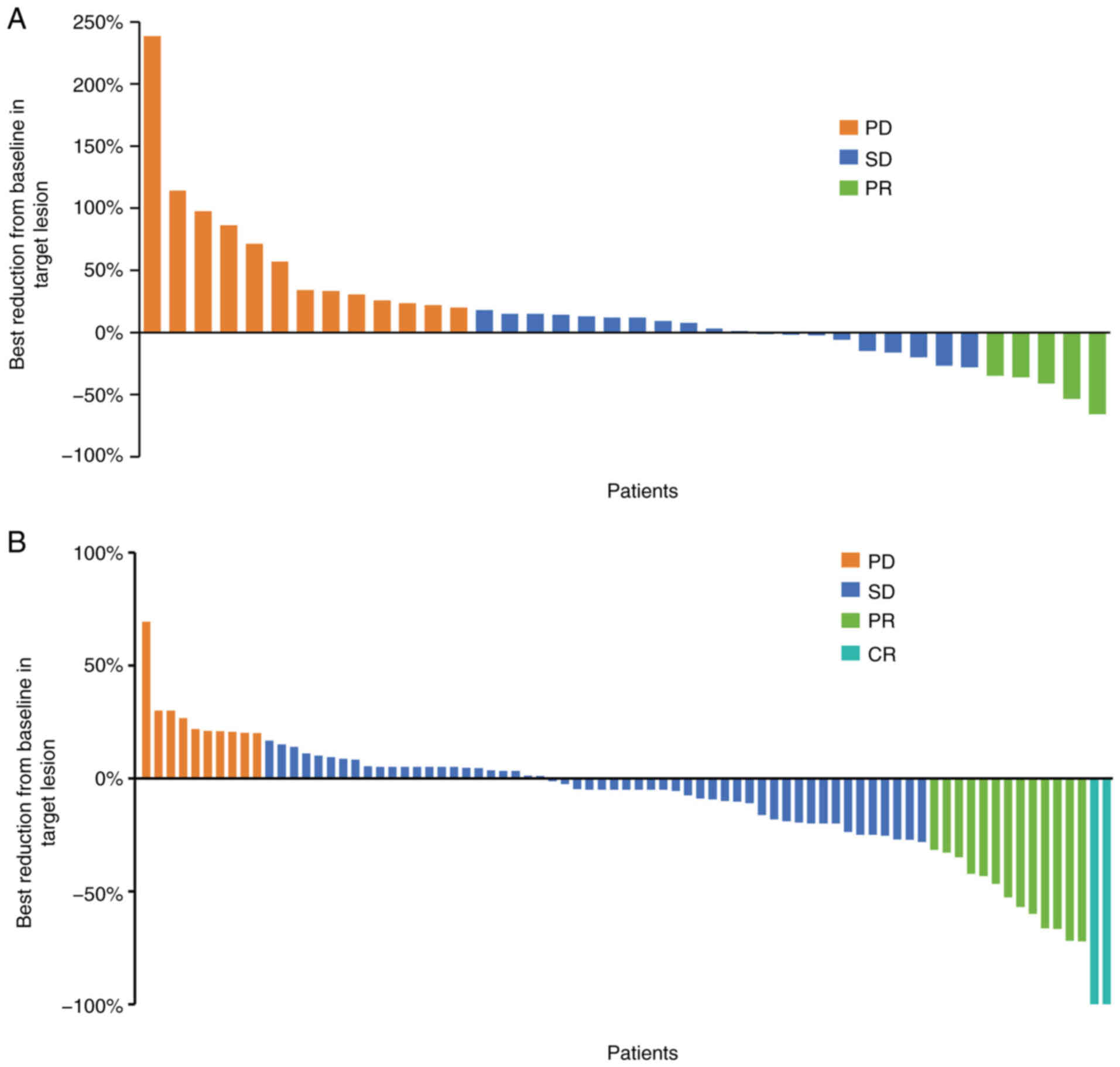
Comprehensive details regarding systemic antitumor therapy, including first-line, second-line and third-line treatment, were collected. After the standardized systemic antitumor therapy, the changes in target lesions in the liver were evaluated based on the Response Evaluation Criteria in Solid Tumors (RECIST) 1.1, such as disease progression (PD), stable disease (SD), partial remission (PR) and complete response (CR). In addition, follow-up information about the patient's condition was also recorded.
Hyper-progressive disease (HPD)
HPD has no uniform standard at present, but it has been widely used in the clinical treatment of tumors. However, within the definition of HPD, a consensus has been reached that the time-to-treatment failure (TTF) is <2 months after systemic drug treatment. Others definitions have some limitations, such as the tumor load being increased by >50% compared with the baseline period and the tumor growth rate after treatment being more than twice the previous rate (16). Currently, there is no clear definition of HPD (17). In the present study, HPD was defined as TTF <2 months.
Statistical analysis
SPSS 21.0 software (IBM Corp.) was used for data processing and analysis. Therapeutic response was evaluated based on RECIST 1.1 standard criteria. Continuous variables are expressed as the mean ± standard deviation and were analyzed using an unpaired t-test. Categorical variables are expressed as n (%) and were analyzed using the χ2 test or Fisher's exact test. Progression-free survival (PFS) and OS were compared using a log-rank test. Hazard ratios (HRs) with 95% confidence intervals (CIs) were estimated using the Cox regression model. Kaplan-Meier curves and median survival times were estimated for each treatment group. Landmark analysis was used to evaluate the effect of treatment intervention at specific time points using R software (version 4.3.1; R Core Team). The test level was α=0.05. P<0.05 was used to indicate a statistically significant difference.
Results
Study population
The present study included 117 patients with advanced liver cancer; of these, 38 patients were in group A (≤35 years old) and 79 patients were in group B (≥55 years old). The mean age in groups A and B was 30.1 years (range, 17–35 years) and 64.1 years (range, 55–86 years), respectively. Men accounted for 86.8% (33/38) in group A and 86.1% (68/79) in group B (P>0.05). There was no statistical difference between group A and group B in terms of etiology, diagnosis, PVTT or tumor stage (P>0.05). However, the previous surgery rate in group A was higher than that in group B (65.8 vs. 39.2%; P=0.007). Among the baseline indices, there was no statistical difference between the two groups with regard to the proportion of patients with increased serum AST, albumin and AFP levels, or high Child-Pugh score (P>0.05). The proportions of patients with increased ALT level (52.6 vs. 26.6%) or rates of HBsAg (92.1 vs. 68.4%) and HBV DNA (36.8 vs. 32.9%) positivity in group A were higher than those in group B (P<0.05). However, the proportions of patients with increased TBIL (7.9 vs. 22.8%) and ECOG score (0.0 vs. 10.1%) were lower in group A than in group B (P<0.05). These findings suggest that the baseline level in group A was worse than that in group B, and that mother-to-child transmission of HBV may be the main cause in group A (Table I).
Clinical efficacy of systemic drug therapy for young patients with PLC
Patients were evaluated by spiral computed tomography every 2 months. In group A, there were 13 (34.2%) patients with PD, 5 (13.2%) patients with PR and 20 (52.6%) patients with SD. None of the patients was evaluated as CR (Fig. 2A). In group B, there were 10 (12.7%) patients with PD, 13 (16.5%) patients with PR, 54 (68.4%) patients with SD, and 2 (2.5%) patients with CR (Fig. 2B). This indicated the poor efficacy of systemic antitumor therapy in young patients with liver cancer compared to elderly patients.
Survival analysis of young patients with liver cancer
Based on the survival analysis, the median PFS (mPFS) time of group A was 3.9 months, while that of group B was 8.3 months, which was 4.4 months shorter (HR, 1.702; P=0.009) (Fig. 3A). A landmark analysis showed that the PFS rate at 12 months of group A was significantly lower than that of group B at 12 months (P=0.001) and 24 months (P<0.001) (Fig. 3C and D). However, there was no significant difference in the HR of PFS between the two groups after the landmarks of 12 and 24 months (P>0.05). The mOS time of group A was 17.6 months, while the mOS time of group B was 30.0 months, which was 12.4 months shorter (HR, 1.799; P=0.010) (Fig. 3B). These findings suggest that young patients with liver cancer show a poor response to treatment and have a short survival time.
Stratified analysis of factors influencing the survival outcomes
Next, the influence of the baseline biochemical and virological indicators on OS was analyzed. The results of the stratified analysis showed that male sex (HR, 1.73; 95% CI, 1.07–2.79), pathological diagnosis (HR, 1.79; 95% CI, 1.10–2.91), previous surgical treatment (HR, 2.16; 95% CI, 1.18–3.95), no PVTT (HR, 2.45; 95% CI, 1.22–4.93), elevated ALT (HR, 2.23; 95% CI, 1.07–4.65), elevated AST (HR, 3.22; 95% CI, 1.62–6.39), normal TBIL (classified as <20.5 µmol/l) (HR, 1.77; 95% CI, 1.09–2.87) and increased AFP (HR, 2.02; 95% CI, 1.19–3.41) were associated with a shorter survival time in group A compared with group B (P<0.05) (Fig. 4). Group A did not show longer OS times compared with group B for any of the subgroups (Fig. 4).
Sensitivity analysis
In the first-line treatment strategy, the longest mPFS time among group B was achieved in the ICIs subgroup, followed by the chemotherapy + ICIs and TKIs + ICIs subgroups. In group A, TKIs + ICIs showed a longer mPFS time of 8.7 months (95% CI, 0.0–18.6 months) compared with that of group B. In the first-line treatment strategy, the longest OS among group B was in the ICIs subgroup, followed by the chemotherapy + ICIs and TKIs + ICIs subgroups. In group A, TKIs + ICIs showed a longer mOS time of 30.9 months (95% CI, 21.3–40.4) compared with that of group B (Table II and Fig. S1).
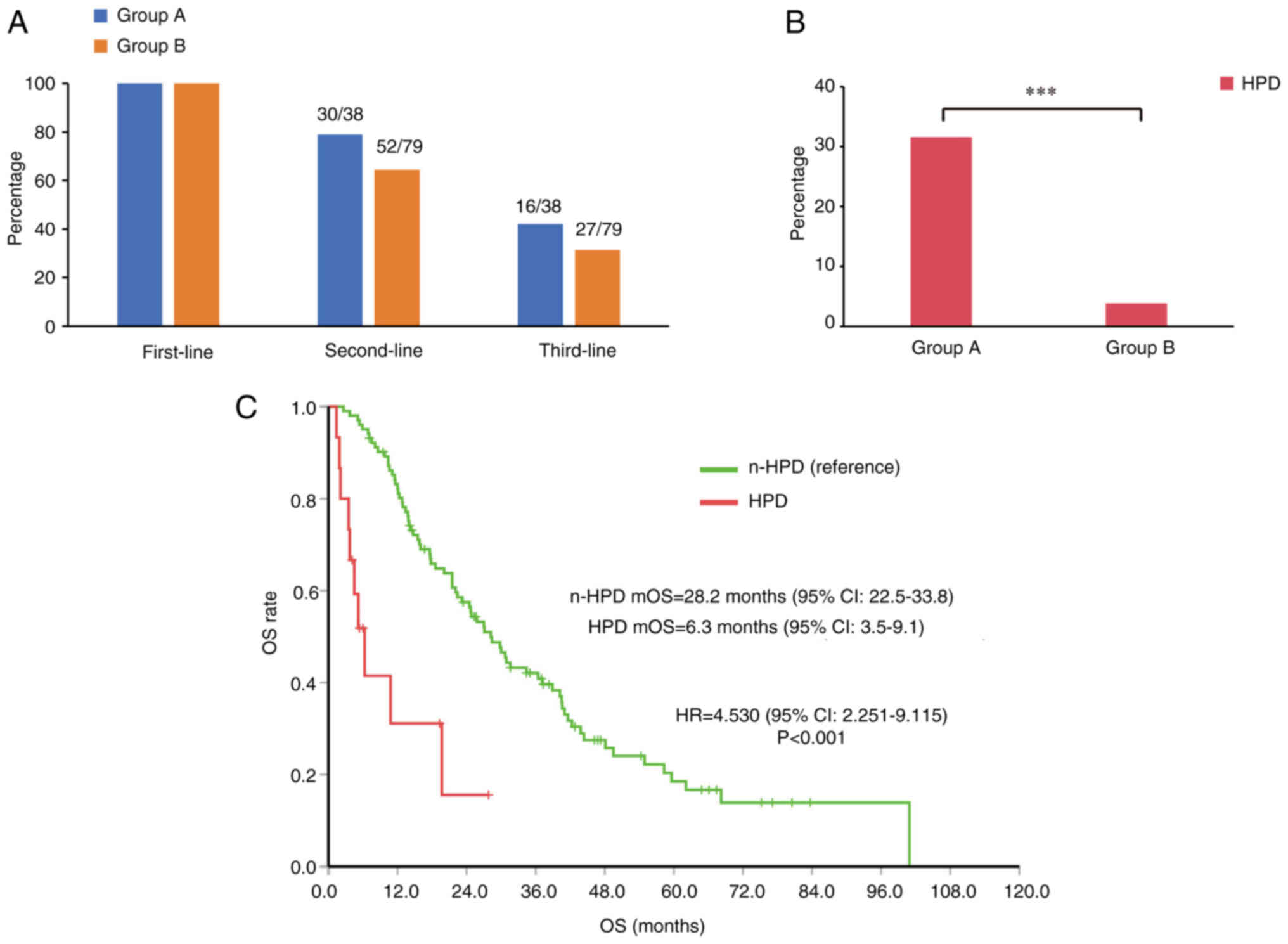
A total of 30 patients in group A and 52 patients in group B received second-line therapy (P>0.05). The number of patients receiving third-line treatment was also higher in group A, but the between-group difference was not statistically significant (P>0.05) (Fig. 5A).
HPD is a key factor affecting survival
HPD is a phenomenon of accelerated tumor growth, which is more common in patients with advanced tumors who use immunosuppressants (17). Most patients with HPD suffer from poor quality of life and a poor prognosis. The incidence of HPD in group A was significantly higher than that in group B (31.6 vs. 3.8%; P<0.001; Fig. 5B). In the total study population, HPD had a significant impact on survival. Analysis showed that HPD was a risk factor for lower mOS time in advanced liver cancer (HR, 4.530; 95% CI, 2.251–9.115; P<0.001; Fig. 5C). These findings suggest that young patients with liver cancer are prone to HPD, and that HPD significantly reduces the survival time of patients.
Discussion
The high prevalence of HBV infection in China has led to a steady increase in the incidence of liver cancer among young people (18). Young cancer patients (≤35 years old) are essentially different from elderly patients (≥55 years old) in terms of disease pathogenesis, treatment and prognosis (19). In the present study, the proportion of patients with elevated ALT levels, HBsAg positivity and HBV DNA positivity were significantly higher in group A. This suggests that the main cause of liver cancer in young patients may be HBV infection. Previous studies have shown that patients with HBV-HCC are characterized by advanced disease at the time of diagnosis. Most of them have lost the opportunity for radical surgery and their survival time is short. In addition, patients with HBV-HCC are prone to recurrence and metastasis after hepatectomy due to the background of HBV infection (10).
For a long time, liver cancer has been considered a disease that mainly affects the elderly, but recent research has shown a change in the age distribution of patients. An increasing number of young people are being diagnosed with liver cancer, which may be related to several factors such as viral hepatitis, heavy alcohol consumption, non-alcoholic fatty liver disease history and excessive consumption of milk/milk substitutes (20). Most young patients with liver cancer have clinical refractory disease (21). In the present study, the mPFS of young patients with liver cancer was shorter by 4.4 months and the mOS was shorter by 12.4 months compared with that of elderly patients. The proportions of patients who received second-line treatment and third-line treatment in group A were higher than those in group B, but the differences were not statistically significant.
HPD is a phenomenon of accelerated tumor growth, which is mostly seen in patients with advanced tumors who use ICI therapies. The incidence of HPD varies in different tumor types, such as non-small cell lung cancer (13.8%), HCC (10.3%) and gastric cancer (16.7%) (16,22,23). This difference is related to the tumor type and the definitions of HPD used in research. Referring to the commonly used research data, the present study defined HPD as TTF <2 months (17). In the present study, the incidence of HPD in group A was significantly higher than that in group B. HPD was found to be a risk factor for advanced liver cancer. Previous studies have also shown that patients with HPD have a worse prognosis and shorter survival time than those without HPD (24–28). Therefore, HPD is a predictor of a poor prognosis in patients with advanced cancer.
Some limitations of the present study should be considered while interpreting the results. This was a single-center cohort study with a small sample size, which may have introduced an element of bias. Moreover, this study was based on real-world data with no standardized protocol for patient selection and treatment follow-up. More robust prospective studies are required to obtain more definitive evidence.
In conclusion, systemic drug therapy showed poor efficacy in young patients with liver cancer. TKIs + ICIs are suitable for first-line treatment. Moreover, young patients with liver cancer are prone to HPD, suggesting the need for close monitoring of these patients to improve the prognosis.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
This study was supported by the Natural Science Foundation of Jiangsu Province (grant no. BK20200275) and the Foundation of Jinling Hospital (grant nos. 22LCZLXJS57, 22LXZLXJS21 and 22LXYY-LH5).
Availability of data and materials
The data generated in the present study may be requested from the corresponding author.
Authors' contributions
JZ and XL conceived and designed the study. ZL, CC and ZX performed data analysis and manuscript preparation. XX, PL and YX assisted with data acquisition and statistical analysis, and confirm the authenticity of all the raw data. All authors read and approved the final manuscript.
Ethics approval and consent to participate
This study involving human participants was reviewed and approved by the Ethics Committee of Nanjing Jinling Hospital (approval no. DZQH-KYLL-23-16).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that that they have no competing interests.
References
|
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A and Bray F: Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 71:209–249. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Tian T, Song C, Jiang L, Dai J, Lin Y, Xu X, Yu C, Ge Z, Ding Y, Wen Y, et al: Hepatitis B virus infection and the risk of cancer among the Chinese population. Int J Cancer. 147:3075–3084. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Li Z, Hou X and Cao G: Is mother-to-infant transmission the most important factor for persistent HBV infection? Emerg Microbes Infect. 4:e302015. View Article : Google Scholar : PubMed/NCBI | |
|
Li Z, Xie Z, Ni H, Zhang Q, Lu W, Yin J, Liu W, Ding Y, Zhao Y, Zhu Y, et al: Mother-to-child transmission of hepatitis B virus: evolution of hepatocellular carcinoma-related viral mutations in the post-immunization era. J Clin Virol. 61:47–54. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Fu J, Yang J, Tan Y, Jiang M, Wen F, Huang Y, Chen H, Yi C, Zheng S and Yuan Y: Young patients (≤35 years old) with colorectal cancer have worse outcomes due to more advanced disease: A 30-year retrospective review. Medicine (Baltimore). 93:e1352014. View Article : Google Scholar : PubMed/NCBI | |
|
Kath R, Fiehler J, Schneider CP and Höffken K: Gastric cancer in very young adults: Apropos four patients and a review of the literature. J Cancer Res Clin Oncol. 126:233–237. 2000. View Article : Google Scholar : PubMed/NCBI | |
|
Wang J, Wang J, Li Q, Zhang P, Yuan P, Ma F, Luo Y, Cai R, Fan Y, Chen S, et al: Young breast cancer patients who develop distant metastasis after surgery have better survival outcomes compared with elderly counterparts. Oncotarget. 8:44851–44859. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Cheng L, Chen S, Wu W, Kuo ZC, Wei Z, Meng S, Chen C, Zhang C and He Y: Gastric cancer in young patients: A separate entity with aggressive features and poor prognosis. J Cancer Res Clin Oncol. 146:2937–2947. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Theuer CP, Kurosaki T, Taylor TH and Anton-Culver H: Unique features of gastric carcinoma in the young: A population-based analysis. Cancer. 83:25–33. 1998. View Article : Google Scholar : PubMed/NCBI | |
|
Li Z, Han N, Ren X, Zhang Y and Chu X: Effectiveness of TKI Inhibitors Combined With PD-1 in Patients With Postoperative Early Recurrence of HCC: A Real-World Study. Front Oncol. 12:8338842022. View Article : Google Scholar : PubMed/NCBI | |
|
Selene II, Ozen M and Patel RA: Hepatocellular Carcinoma: Advances in systemic therapy. Semin Intervent Radiol. 41:56–62. 2024. View Article : Google Scholar : PubMed/NCBI | |
|
Tanaka J, Kurisu A, Ohara M, Ouoba S, Ohisa M, Sugiyama A, Wang ML, Hiebert L, Kanto T and Akita T: Burden of chronic hepatitis B and C infections in 2015 and future trends in Japan: A simulation study. Lancet Reg Health West Pac. 22:1004282022.PubMed/NCBI | |
|
Mogul DB, Ling SC, Murray KF, Schwarzenberg SJ, Rudzinski ER and Schwarz KB: Characteristics of Hepatitis B virus-associated hepatocellular carcinoma in children: A multi-center study. J Pediatr Gastroenterol Nutr. 67:437–440. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Jacob KA, Hjortnaes J, Kranenburg G, de Heer F and Kluin J: Mortality after cardiac surgery in patients with liver cirrhosis classified by the Child-Pugh score. Interact Cardiovasc Thorac Surg. 20:520–530. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Llovet JM, Brú C and Bruix J: Prognosis of hepatocellular carcinoma: The BCLC staging classification. Semin Liver Dis. 19:329–338. 1999. View Article : Google Scholar : PubMed/NCBI | |
|
Kubota Y, Yoshimura K, Hamada K, Hirasawa Y, Shida M, Taniguchi M, Matsui H, Ariizumi H, Ishiguro T, Suzuki N, et al: Rare Nivolumab-associated super hyper progressive disease in patients with advanced gastric cancer. In Vivo. 35:1865–1875. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Ding P, Wen L, Tong F, Zhang R, Huang Y and Dong X: Mechanism underlying the immune checkpoint inhibitor-induced hyper-progressive state of cancer. Cancer Drug Resist. 5:147–164. 2022.PubMed/NCBI | |
|
Ju Y, Han G, Zhang P, Xu J, Chen C, Jiang H, Yuan D, Ye X and Zhou G: Staging and clinical characteristics of pregnant women with chronic hepatitis B virus infection: A retrospective cohort study from Nanjing, China. J Obstet Gynaecol Res. 49:2427–2435. 2023. View Article : Google Scholar : PubMed/NCBI | |
|
Pu JL, Chen Z, Yao LQ, Feng JY, Diao YK, Guan MC, Li JD, Chen ZL, Zhou YH, Wang H, et al: Long-term oncological prognosis after curative-intent liver resection for hepatocellular carcinoma in the young versus the elderly: Multicentre propensity score-matching study. BJS Open. 6:zrab1452022. View Article : Google Scholar : PubMed/NCBI | |
|
Almohaid S and Akhtar S: Diet, lifestyle factors, comorbidities, and hepatocellular carcinoma risk in a middle eastern country: A case-control study. BMC Cancer. 24:6942021. View Article : Google Scholar : PubMed/NCBI | |
|
Zhang W, Jiang R, Hou J and Sun B: Clinicopathological features and prognostic factors of young patients with surgically treated liver cancer. Medicine (Baltimore). 94:e6842015. View Article : Google Scholar : PubMed/NCBI | |
|
Ferrara R, Mezquita L, Texier M, Lahmar J, Audigier-Valette C, Tessonnier L, Mazieres J, Zalcman G, Brosseau S, Le Moulec S, et al: Hyperprogressive disease in patients with advanced non-small cell lung cancer treated with PD-1/PD-L1 inhibitors or with single-agent chemotherapy. JAMA Oncol. 4:1543–1552. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Aoki T, Kudo M, Ueshima K, Morita M, Chishina H, Takita M, Hagiwara S, Ida H, Minami Y, Tsurusaki M and Nishida N: Incidence of hyper progressive disease in combination immunotherapy and anti-programmed cell death protein 1/programmed death-ligand 1 monotherapy for unresectable hepatocellular carcinoma. Liver Cancer. 13:56–69. 2023. View Article : Google Scholar : PubMed/NCBI | |
|
Tanaka T, Koga H, Suzuki H, Iwamoto H, Sakaue T, Masuda A, Nakamura T, Akiba J, Yano H, Torimura T and Kawaguchi T: Anti-PD-L1 antibodies promote cellular proliferation by activating the PD-L1-AXL signal relay in liver cancer cells. Hepatol Int. 18:984–997. 2024. View Article : Google Scholar : PubMed/NCBI | |
|
Zhang L, Feng J, Kuang T, Chai D, Qiu Z, Deng W, Dong K, Zhao K and Wang W: Blood biomarkers predict outcomes in patients with hepatocellular carcinoma treated with immune checkpoint Inhibitors: A pooled analysis of 44 retrospective sudies. Int Immunopharmacol. 118:1100192023. View Article : Google Scholar : PubMed/NCBI | |
|
Li Q, Han J, Yang Y and Chen Y: PD-1/PD-L1 checkpoint inhibitors in advanced hepatocellular carcinoma immunotherapy. Front Immunol. 13:10709612022. View Article : Google Scholar : PubMed/NCBI | |
|
Kim CG, Kim C, Yoon SE, Kim KH, Choi SJ, Kang B, Kim HR, Park SH, Shin EC, Kim YY, et al: Hyperprogressive disease during PD-1 blockade in patients with advanced hepatocellular carcinoma. J Hepatol. 74:350–359. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Zhang L, Wu L, Chen Q, Zhang B, Liu J, Liu S, Mo X, Li M, Chen Z, Chen L, et al: Predicting hyperprogressive disease in patients with advanced hepatocellular carcinoma treated with anti-programmed cell death 1 therapy. EClinicalMedicine. 31:1006732020. View Article : Google Scholar : PubMed/NCBI |