Proteins of the Wnt signaling pathway as targets for the regulation of CD133+ cancer stem cells in glioblastoma
- Authors:
- Published online on: March 5, 2019 https://doi.org/10.3892/or.2019.7043
- Pages: 3080-3088
Abstract
Introduction
Glioblastoma multiforme (GBM) is an aggressive malignant human brain tumor (1). The prognosis for patients with GBM is unfavorable. Despite modern treatment protocols, the median survival time is 15 months, with only 27% of patients living longer than 2 years following diagnosis (2,3). Treatment resistance is commonly associated with cancer stem cells (CSCs) in GBM (4–6). High levels of radiation and chemotherapy, including modern cytostatic agents and targeted drugs, are unable to eliminate CSCs (7). It is therefore, required to develop new approaches for GBM treatment and identify new molecular targets that may assist the regulation of CSCs by inhibiting their proliferative capabilities.
The present study investigated GBM cells that express the cluster of differentiation 133 (CD133) membrane antigen, a well-known CSC marker (8). Cells of this type exhibit a high proliferation rate; therefore, unlike differentiated CD133− cancer cells, CD133+ CSCs are susceptible to radiation and chemotherapy (9). In small quantities, CD133+ CSCs have previously been demonstrated to form large tumors when implanted into the brains or experimental animals (10). More than 60% of intracellular proteins from GBM CD133+ CSCs are identical to proteins present in normal neural stem cells of a human brain (11). This suggests that similarities exist between the main mechanisms regulating the proliferative properties of these cell types.
Proliferation of all types of stem cells depends on the activation of the Wnt signaling pathway (12). In different types of malignant tumors, the activation of this pathway stimulates the proliferation of CSCs, which promotes tumor relapse and the development of therapeutic resistance (13–15). A direct correlation between the aggressive nature of GBM and the activation of the Wnt signaling pathway in CSCs has previously been described (16). Another previous study demonstrated that the suppression of the Wnt cascade decreased the heterogeneity of GBM cells (17). Therefore, differentially expressed proteins (DEPs) of the Wnt signaling pathway are prospective targets for regulating the proliferative properties of CSCs in GBM. The aim of the present study was to compare the expression levels of proteins associated with the Wnt signaling pathway in CD133+ CSCs of human GBM and differentiated СD133− cancer cells.
Materials and methods
Human GBM cells
The present study used the U-87MG GBM cell line obtained from the American Type Culture Collection (cat. no. HTB-14™; ATCC; Manassas, VA, USA). This cell line is not the original U-87 line established at the University of Uppsala, but a human GBM of unknown origin (18). However, as demonstrated in our previous study (11), CD133+ cells of this cell line exhibit similar proteome profiles to neural CD133+ human stem cells and exhibit significant proteomic differences compared with normal mesenchymal stem cells of the human bone marrow. In our previous study, the stimulation of GBM U-87MG cells with transforming growth factor (TGF)-β1 led to a significant increase in the expression of proteins associated with the epithelial-mesenchymal transition (EMT) (19), which greatly increased the invasiveness of the cells. The U-87MG cell line of GBM possesses a significant amount of CD133+ CSCs that actively interact with both cancerous and non-cancerous cells (20). The extensive information that is available regarding this GBM cell line makes it the optimal choice for the present study.
The U-87MG cells were cultured in low glucose Dulbecco's modified Eagle's medium (DMEM; Gibco; Thermo Fisher Scientific, Inc., Waltham, MA, USA) with 10% fetal bovine serum (FBS; Gibco; Thermo Fisher Scientific, Inc.) in standard conditions (5% CO2 and 37°C). The cells were cultured until they reached 80% confluence. To obtain glioma spheres the cells were resuspended in DMEM/F12 (Thermo Fisher Scientific, Inc.) containing L-glutamine, B27, 20 ng/ml bFGF, 20 ng/ml EGF, 100 U/ml penicillin/streptomycin and 5 µg/ml heparin. All chemicals were obtained from Gibco; (Thermo Fisher Scientific, Inc.). Cells were grown in T75 culture flasks. Every 3 days, fresh growth factors were added. The extraction of CD133+ cells was performed via immunosorting using magnetic beads with immobilized antibodies against CD133 (CD133 MicroBead kit; cat. no. 130-100-857; Miltenyi Biotec, Inc., San Diego, CA, USA). The purity of the isolated population was assessed by flow cytometry and CD133/1 (AC133)-VioBright FITC antibodies (cat. no. 130-105-226; Miltenyi Biotec, Inc.). The dye was diluted at a ratio of 1:11 for 107 cells/100 µl of buffer solution [7.2 pH phosphate-buffered saline (PBS), 0.5% bovine serum albumin (BSA) and 2 mM EDTA]. The antigen was labeled by incubation for 10 min in the dark (4°C) to prevent non-specific cell labeling.
Mass spectrometry of samples
High-performance liquid chromatography-mass spectrometry was applied and the label-free method was used to evaluate changes in the protein expression level. Two cell samples (CD133+ CSCs and cancer CD133− non-stem cells) were lysed with Mammalian Cell Lysis kit (MCL1-1KT; Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) and low-molecular compounds were removed. Subsequently, enzymatic cleavage was performed and 4 µl of solution was analyzed by mass spectrometry. The samples were incubated at 30°С in a Labconco CentriVap centrifugal concentrator (Labconco Corp., Kansas City, MI, USA) to remove ammonium bicarbonate. Peptides were diluted during the mobile stage with 30% acetonitrile, 70% water and 0.1% formic acid (рН 2.7) and divided into 24 fractions using a Dionex UltiMate 3000 (Dionex Corp., Sunnyvale, CA, USA), equipped with a fraction collector and cation exchange column MIC-10-CP (Puros 10S; 1 mm × 10 cm; Thermo Fisher Scientific, Inc.). The obtained fractions were concentrated at 30°С in the centrifugal concentrator and diluted with 0.1% formic acid (100 µl).
Peptides were analyzed using Dionex Ultimate 3000 (Dionex Corp.), LTQ Orbitrap XL and Orbitrap Fusion mass spectrometer (Thermo Fisher Scientific, Inc.) with nanospray ionization. Peptide division was performed using an Acclaim C18 PepMap 100 column (75 µm х 150 mm; grit size, 3 µm; Dionex Corp.). Mass spectrometry data were processed using MaxQuant 1.6.1.0 (21–23) and Perseus 1.6.1 software (Max Planck Institute of Biochemistry, Planegg, Germany). Biological processes, molecular functions, cell location and protein signaling pathways were annotated using the following databases: PubMed (http://www.ncbi.nlm.nih.gov/pubmed), Protein Analysis Through Evolutionary Relationships (http://www.pantherdb.org), Gene Ontology (http://www.geneontology.org), Kyoto Encyclopedia of Genes and Genomes (http://www.genome.jp/kegg/) and Search Tool for the Retrieval of Interacting Genes/Proteins v10. (https://string-db.org/).
Statistical analysis
Statistical significance was identified using Student's t-test [STATISTICA 12 (StatSoft, Moscow, Russia]. P<0.05 was considered to indicate a statistically significant difference.
Results
General characteristics of the identified proteins
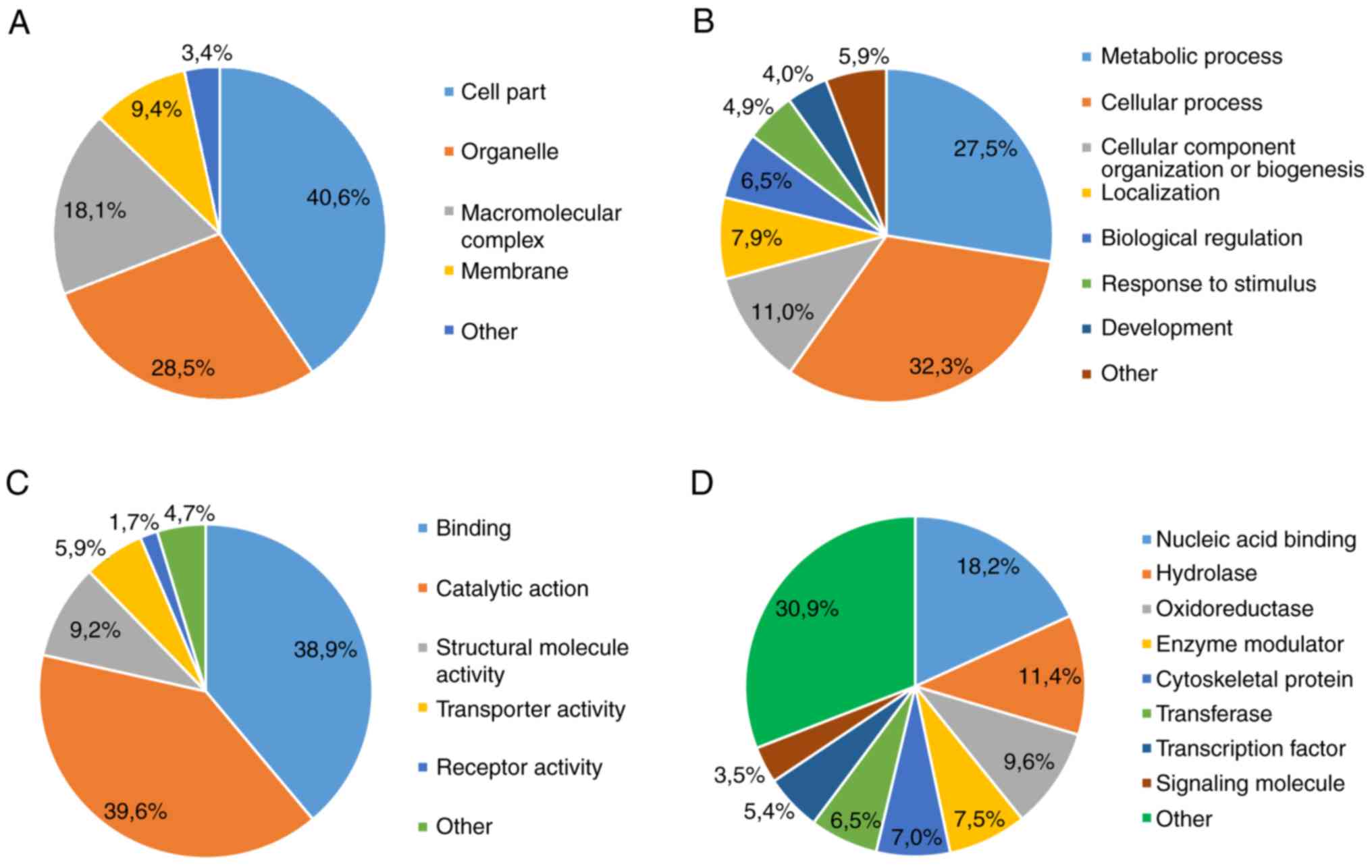
A total of 1,904 proteins were identified in both samples of GBM cells. A total of 1,696 proteins were identified in GBM CD133+ CSCs and 1,435 proteins in GBM CD133− non-stem cells. The molecular mass of the proteins was 4–3,995 kDa. A total of 1,227 proteins (64.4% of the total 1,904 proteins) were detected in all cell lysates, 469 proteins only in CSCs and 208 proteins only in the non-stem cells. A total of 589 (34.7% of 1,904) DEPs were identified to exhibit significantly different expression levels in CSCs, as compared with non-stem cells (P<0.05). The majority of DEPs were: i) Localized intracellularly (Fig. 1A); ii) associated with metabolic and cellular processes (Fig. 1B); iii) functionally heterogeneous (Fig. 1C); and iv) associated with a class of compounds that exhibit active fermentation properties (Fig. 1D).
Bioinformatics analysis of the identified proteins
A total of 116 DEPs were found to be associated with 15 signaling pathways (Table I). Among these 116 DEPs, 88 were upregulated and 28 downregulated in GBM CSCs. The upregulation was observed in proteins associated with intracellular signaling pathways, including proteins involved with the extracellular matrix (cell adhesion molecules, ECM receptor interaction and focal adhesion) and local microenvironment (tight and adherens junctions). The majority of upregulated proteins were associated with the glycolysis pathway and Wnt signaling cascade (Tables I and II). The majority of the downregulated proteins were revealed to be associated with the insulin signaling pathway and MAPK signaling pathway (Table I).
Table I.Participation of differentially expressed proteins of glioblastoma CD133+ stem cells in the intracellular signaling pathways. |
Discussion
Cancer stem cells (CSCs) are an important challenge in the treatment of glioblastoma multiforme (GBM). The absence of drugs and medical technologies for the effective elimination of CSCs in a patient's body has shifted the focus of modern research to molecular genetics. The discovery of certain GBM isotypes based on molecular genetic analysis has provided insights into the pathogenesis of GBM; however, there remains a requirement to identify mechanisms to regulate and control CSCs (7).
The present study characterized CD133+ CSCs as distinct cells with quantitative and qualitative differences, when compared with differentiated cells in GBM. A number of proteins were identified to exhibit a different level of expression in CSCs, as compared with differentiated cells in GBM. Furthermore, it was demonstrated herein that the upregulated proteins in CSCs were associated with the mechanisms of invasion, survival and proliferation. Both of these findings require further in-depth analysis. In addition to the aforementioned mechanisms, a significant change was observed in the expression of proteins associated with the Wnt signaling pathway, which was the main focus of the present study.
Embryonic cells with high levels of Wnt synthesis are known to develop into endodermal and cardiac cells, while cells with a low level of Wnt synthesis form ectoderm layers. Despite GBM being a primary neuroectodermal tumor, a number of studies have suggested its treatment resistance is associated with the activation of the Wnt pathway in CSCs (16). This statement is supported by the presence of CD133 on the surface of normal neural and hematopoietic stem, endothelial progenitor and normal postnatal stem cells, and progenitor cells of other types (21), in which the Wnt signaling pathway plays a key role (12,13). In addition, CD133 is present in the kidneys, mammary glands, trachea, salivary glands, placenta, intestinal cells and ovaries, where the activation of the Wnt/β-catenin signaling pathway is associated with drug resistance and the development of aggressive types of cancer (22–24). Therefore, it can be hypothesized that these mechanisms are similar in GBM.
The upregulation of the Wnt cascade in GBM CSCs was not confirmed in the present study. The expression levels of established proteins of this cascade, including Wnt ligands, frizzled receptors and co-receptor LRP5/6, were not identified to be significantly increased in GBM. However, the upregulation of components of the Wnt signaling pathway was associated with unusual characteristics of CSCs.
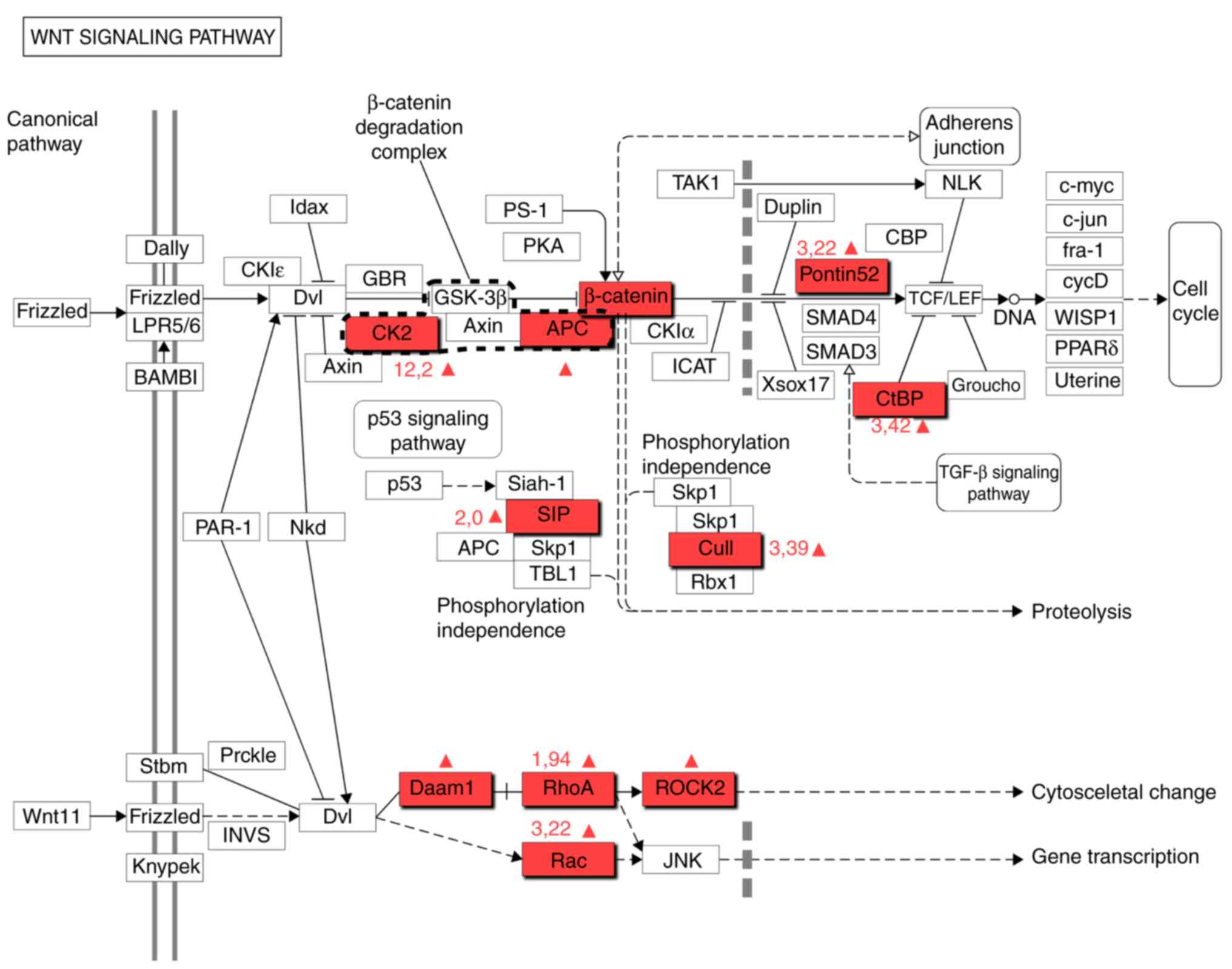
Adenomatous polyposis coli (APC) protein was revealed to be significantly upregulated in GBM CSCs (Fig. 2). This finding had previously been demonstrated in GBM (25). An APC gene mutation encodes a protein that is a key component of Turcot syndrome, a known risk factor for GBM (26). The present study demonstrated that the upregulation of this protein is typical in CSCs, which indicates that these cells may play a critical role in GBM biology.
The expression of calcyclin-binding and Siah-1 interacting (CacyBP/SIP) proteins was found to be 2-fold higher in CSCs, as compared with GBM CD133− cells (Fig. 2). This protein is crucial for the proliferation, differentiation, apoptosis, transcription, ubiquitination and cytoskeleton organization (27). In addition, it regulates the degradation of β-catenin. High levels of CacyBP/SIP are typical in cells of Wnt-associated stomach and colon tumors, as well as neurons. Furthermore, this protein is a component of the p53 signaling pathway that is important for GBM (7). High levels of CacyBP/SIP are important for the proliferation of CSCs, as it can act as an antagonist of p27-selective cyclin-dependent kinase inhibitor 1B (28). The upregulation of CacyBP/SIP has been revealed to be associated with a high resistance to doxorubicin and other cytotoxic agents (29). CacyBP/SIP can be used as a marker of the condition of GBM cell population and serve as a potential target for the regulation of CSCs. Therefore, inhibiting CacyBP/SIP expression can increase the efficiency of therapy against GBM.
Сasein kinase 2 (CK2), a component of the canonical Wnt/β-catenin signaling pathway, regulates the cell cycle, apoptosis and transcription of stem cells (30). CK2, as well as APC, is a crucial component of a β-catenin degrading complex (Fig. 2). Furthermore, this protein is associated with nuclear factor-κB (NF-κB), phosphoinositide 3-kinase/AKT and signal transducer and activation of transcription signaling in GBM cells (31). CK2 consists of two catalytic subunits, CSNK2A2 and CSNK2B. The present study demonstrated a significant increase in CSNK2A2 and CSNK2B expression levels (5.24- and 12.21-fold, respectively) in GBM CSCs. CK2α is a regulator of the Wnt/β-catenin signaling pathway; therefore, the expression levels of this protein are increased in numerous types of tumors.
The expression of CSNK2A2 and CSNK2B has been identified in GBM CSCs. A treatment option that inhibits CK2 has been demonstrated to decrease the expression of CSC markers in a GBM cell culture (32). Compared with temozolomide monotherapy, CX-4945, a specific CK2 inhibitor, was revealed to inhibit the generation of glioma spheres in vitro and significantly increase the survival of animals with acquired GBM (33). Considering the aforementioned results, the CSNK2A2 and CSNK2B subunits may serve as targets for the regulation of CSCs in GBM treatment.
β-catenin is a key element of the Wnt signaling pathway and is associated with the self-renewal of stem cells (34,35). According to the present experimental data, the expression of the β-catenin (CTNNB1) was 6-fold higher in CD133+ CSCs, when compared with CD133− cells in GBM. The inhibition of β-catenin in U87 cells decreased the migration activity of these cancer cells (36). In addition, the expression of this protein was increased in glial tumor cells, which plays a crucial role in CSC invasion (37), survival and proliferation (38). The pharmacological inhibition of the β-catenin expression reduced the ability of GBM cells to create glioma spheres in vitro (39). A combination of the β-catenin inhibitor tetrandrine, an isoquinoline alkaloid, with temozolomide has been demonstrated to increase the efficiency of GBM treatment.
The present study revealed a significant increase in the expression of key components associated with the degradation of β-catenin including APC, CK2α and CK2β. In addition, a 6-fold increase of β-catenin in GBM CSCs was identified, which is a notable finding due to the key roles of β-catenin in CSCs. β-catenin is a central element of the Wnt signaling cascade, as it coordinates and determines the activity of this pathway and other intracellular signaling mechanisms. An increased production of APC and CK2 with high levels of β-catenin in GBM cells suggests a lack of influence of Wnt ligand in glioma spheres rather than a low productivity of these proteins. Furthermore, the upregulation of destruction complex proteins suggests that β-catenin may be associated with the cell membrane, where it coordinates extracellular interaction in glioma spheres.
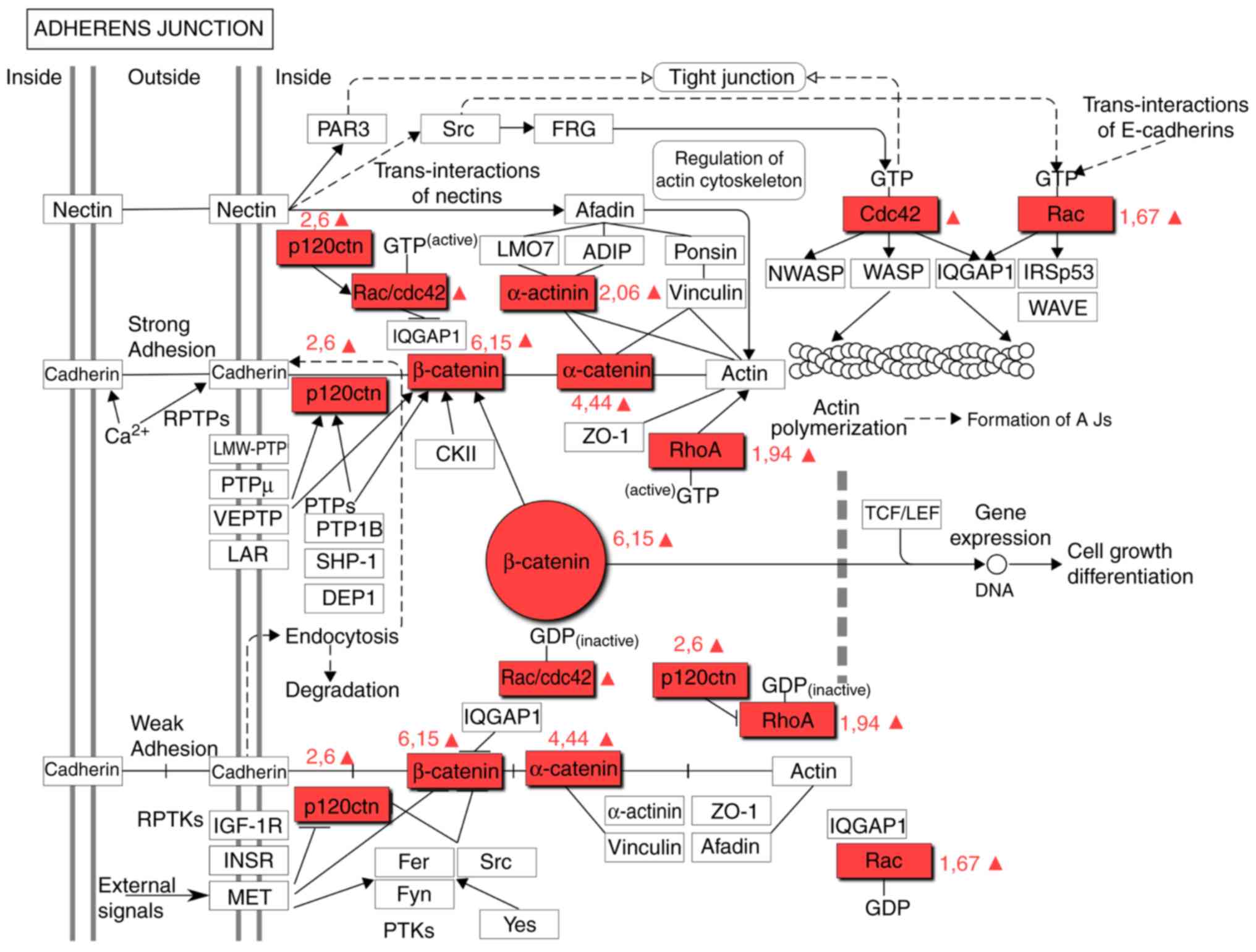
This is supported by the evidence that β-catenin is a component of the adherens junction pathway (Fig. 3). The upregulation of proteins associated with the adherens junction pathway has previously been described as a characteristic of GBM cells (Table III) (25). However, the present results suggested that this is a characteristic attributed only to CD133+ CSCs. α-Catenin (CTNNA1) and δ-catenin (CTNND1), critical components of the adherens junction pathway, were identified to be upregulated in CSCs (4.44- and 2.6-fold, respectively), which was consistent with an increase in CTNNB1. The CTNNA1 tumor-suppressor gene, which encodes α-catenin, is one of the most frequently deleted or mutated genes in cancer (40). α-Catenin is an essential protein in adherens junctions, which are critical for maintaining intercellular adhesion and cellular polarity.
Table III.Changes in the expression of adherens junction signaling proteins in CD133+ CSCs of glioblastoma. |
The fact that α-catenin was also upregulated in CD133+ CSCs suggests that CSCs exhibit denser intercellular connections, as compared with CD133− cells. It is possible that β-catenin is upregulated in GMB cells as a result of transforming non-CSCs into CSCs. CTNNA1 inhibits the proliferation and invasion of cancer cells into different tissues by suppressing the Hippo-Yes-associated protein (YAP) and NF-κB signaling. The depletion of CTNNA1 and CTNND1 promotes the mobility and growth of cancer cells (41). In summary, CTNNA1, CTNNB1 and CTNND1 proteins may be treated as potential targets for regulating the plasticity of GBM cells.
Cullin-1 (CUL1) is a component of the Wnt signaling pathway (Fig. 2). The present study identified that the expression level of CUL1 in CD133+ cells of GBM was 3.39-fold higher than that in CD133− cells of the common pool. CUL1 is involved in different intracellular processes, including proliferation, differentiation and apoptosis. The hyperexpression of CUL1 was revealed to be a marker of poor prognosis for patients with stomach carcinoma, breast cancer and non-small-cell lung carcinoma. The expression of CUL1 has been demonstrated to be significantly higher in glioma cells than in normal brain tissue (42). Theoretically, the inhibition of CUL1 in GBM cells with CUL1 small interfering RNA may prevent the migration and invasion of cancer cells due to a lower level of matrix metallopeptidase (MMP)-2 and MMP-8 expression.
Rac family small GTPase 2 (Rac2), Ras homolog gene family member A (RhoA) and disheveled associated activator of morphogenesis 1 (Daam1) proteins are integrated in the Wnt signaling pathway (Fig. 2). The Rac2 and RhoA proteins are also components of the signaling pathway of adherens junctions (Fig. 3). Rac proteins are a subfamily of Rho small GTPases. The function of this family involves modifying the actin cytoskeleton and proliferation, and regulating key stem cell properties (43). Rac2 is a marker of more aggressive GBM subtypes (44). The present study demonstrated that the expression level of Rac2 in CD133+ cells was 1.67-fold higher. Rho GTPases belong to the Ras superfamily and these proteins, including RhoA, Rac1 and cell division control protein 42 homolog, support the transformation of the cell cytoskeleton during the epithelial-mesenchymal transition (EMT). RhoA is actively expressed in GBM cells, which promotes the migration and invasion of cancer cells. The simultaneous activation of Rac and RhoA was revealed to increase the invasive properties of CSCs (43). The present study revealed that the expression level of RhoA was 1.94-fold higher in CD133+ cell than in the non-CSCs. Simvastin, NSC23766 and specific microRNAs can impact the expression of the aforementioned proteins (44).
C-terminal-binding proteins (CtBP) have two isoforms, CtBP1 and CtBP2, which are involved in the Wnt/β-catenin signaling pathway and other molecular mechanisms determining the development of malignant tumors, invasion of neoplastic cells, apoptosis and response to therapy (45). The present study revealed that the expression levels of CtBP1 and CtBP2 were significantly higher in GBM CD133+ cells (3.42- and 2.24-fold, respectively). CtBP inhibits the expression of tumor suppressor genes (46), serves a role in the epithelial-mesenchymal transition, regulates β-catenin, mediates the transcription factor 4/lymphoid enhancer-binding factor 1 axis and activates targeted genes involved in the self-regeneration of CSCs (47). Combining the CtBP inhibitor MTOB with temozolomide may serve as a potential treatment option for GBM.
RuvB-like AAA ATPase 1 (RUVBL1 or Ponti52) is a component of the Wnt signaling pathway (Fig. 2) that is essential for tumor cell growth and viability. This study identified that the expression level of RUVBL1 was significantly higher in GBM CD133+ than in GBM CD133− cells of the common pool (Table II). RUVBL1 plays a key role in the cell cycle, mitosis, chromatin remodeling, transcription, DNA repair, apoptosis and regulation of development of normal stem cells (48,49). It also participates in oncogenic signaling pathways, including c-Myc and Wnt. RUVBL1 regulates the activity of glucocorticosteroid and estrogen receptors in the nucleus, and is essential in choosing the optimum pharmacological scheme (50). The inhibition of RUVBL1 activity interferes with the expression of genes responsible for the response of GBM to hypoxia and is associated with an aggressive tumor phenotype (51). The inactivation of this gene with microRNA can increase the efficiency of GBM therapy.
Of note, the Wnt-associated proteins CtBP and RUVBL1 regulate key gene expression in CSCs of all types of cancer. These proteins are part of the SMAD signaling cascade, which is mostly activated by TGF-β and is crucial to GBM pathogenesis (19). It can be suggested that via SMAD proteins of the TGF-β pathway, CtBP and RUVBL1 generate a closed system that supports the stemness of GBM cells; however, this requires further investigation.
In conclusion, the present study attempted to identify molecular targets that may assist with the regulation of GBM CSC proliferation. The study focused on selective analysis of proteins associated with the Wnt signaling pathway in CD133+ CSCs. In GBM CD133+ CSCs, an increased expression of 12 proteins that are components of the Wnt signaling pathway was identified; a number of these proteins, including CTNNB1, Daam1, Rac2 and RhoA, are also components of the adherens junction pathway. CacyBP, CSNK2A2, CSNK2B, CtBP1, CtBP2, CUL1 and RUVBL1 may serve as targets for the pharmaceutical regulation of CSCs in GBM treatment. Furthermore, the increased expression of APC, β-catenin, CtBP and RUVBL1 suggested the possibility of alternative activation of genes in CD133+ CSCs; however, this requires further investigation.
It is essential to note that suppressing proteins of the Wnt signaling pathway are required not for producing a cytostatic and cytotoxic effect on GBM cells of the common pool, but in order to inhibit the reproductive function of CSCs and, as a result, extend the remission period. Therefore, conceptually new methods and techniques need to be developed in order to evaluate the efficiency of suppressing these targets. For instance, taking into consideration the fact that β-catenin and certain upregulated Wnt-proteins belong to the signaling pathway of adherens junctions, the efficiency of suppressing this target could be evaluated not just based on the amount of β-catenin in CSCs, but also on the strength of adherens junctions in a gliomasphere, AFM investigation, time of gliomasphere creation if cultivated in serum-free media, speed of cell growth in the standard media with serum and immunophenotype of these cells' progenitors identified by flow cytometry. We plan to attempt this in the nearest future, using CD133+ CSCs from the samples of a human brain with GBM. Furthermore, the efficiency of the targeted therapy on extending the life expectancy of patients may not be very high, since upregulated proteins are involved in several signaling pathways. That is why suppressing one target may have conflicting results. The way to solve this issue is a systemic analysis of survival using the Kaplan-Meier curve for GBM patients with a significant expression of one of the described proteins (CTNNB1, Daam1, Rac, RhoA, CacyBP, CSNK2A2, CSNK2B, CtBP1, CtBP2, CUL1 and RUVBL1) in their CD133+ CSCs. This approach could become a breakthrough targeted therapy for GBM.
Acknowledgements
Not applicable.
Funding
The present study was funded by the Ministry of Education and Science of the Russian Federation (grant no. 14.584.21.0027; ID, RFMEFI58417X0030RFMEFI58417X0027).
Availability of data and materials
All data and materials are available upon request.
Authors' contributions
VS prepared and analyzed the samples, as well as performed the cell lysis, chromatography and mass spectrometry, and contributed to the bioinformatics analysis. NA and MK cultured the cancer cells and isolated the cancer CD133+ stem cells of glioblastoma for the experiment. SZ provided and performed the statistical analysis and was responsible for the mathematical process of the results. YK and HS discussed, analyzed and interpreted the results of the study, and also worked on the manuscript. IB wrote the manuscript, proposed the study idea, designed the study, offered support with the experiments, organized the scientific team, provided scientific guidance and contributed to the bioinformatics analysis. All authors read and approved the manuscript and agree to be accountable for all aspects of the research in ensuring that the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Ethics approval and consent to participate
The present study was approved by the Ethics Committee of the School of Biomedicine, The Far Eastern Federal University (Vladivostok, Russia) and the Academic Council of the School of Biomedicine.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
|
Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella- Branger D, Cavenee WK, Ohgaki H, Wiestler OD, Kleihues P and Ellison DW: The 2016 World Health Organization Classification of Tumors of the central nervous system: A summary. Acta Neuropathol. 131:803–820. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Stupp R, Brada M, van den Bent MJ, Tonn JC and Pentheroudakis G; ESMO Guidelines Working Group, : High-grade glioma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 25 (Suppl 3):iii93–iii101. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, Belanger K, Brandes AA, Marosi C, Bogdahn U, et al: Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med. 352:987–996. 2005. View Article : Google Scholar : PubMed/NCBI | |
|
Rycaj K and Tang DG: Cancer stem cells and radioresistance. Int J Radiat Biol. 90:615–621. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Chang L, Graham P, Hao J, Ni J, Deng J, Bucci J, Malouf D, Gillatt D and Li Y: Cancer stem cells and signaling pathways in radio-resistance. Oncotarget. 7:11002–11017. 2016.PubMed/NCBI | |
|
Friedmann-Morvinski D: Glioblastoma heterogeneity and cancer cell plasticity. Crit Rev Oncog. 19:327–336. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Bryukhovetskiy I, Ponomarenko A, Lyakhova I, Zaitsev S, Zayats Y, Korneyko M, Eliseikina M, Mischenko P, Shevchenko V, Shanker Sharma H, et al: Personalized regulation of glioblastoma cancer stem cells based on biomedical technologies: From theory to experiment (Review). Int J Mol Med. 42:691–702. 2018.PubMed/NCBI | |
|
Bradshaw A, Wickremesekera A, Brasch HD, Chibnall AM, Davis PF, Tan ST and Itinteang T: Cancer stem cells in glioblastoma multiforme. Front Surg. 3:482016. View Article : Google Scholar : PubMed/NCBI | |
|
Brown DV, Filiz G, Daniel PM, Hollande F, Dworkin S, Amiridis S, Kountouri N, Ng W, Morokoff AP and Mantamadiotis T: Expression of CD133 and CD44 in glioblastoma stem cells correlates with cell proliferation, phenotype stability and intra-tumor heterogeneity. PLoS One. 12:e01727912017. View Article : Google Scholar : PubMed/NCBI | |
|
Brown DV, Daniel PM, D'Abaco GM, Gogos A, Ng W, Morokoff AP and Mantamadiotis T: Coexpression analysis of CD133 and CD44 identifies proneural and mesenchymal subtypes of glioblastoma multiforme. Oncotarget. 6:6267–6280. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Bryukhovetskiy A, Shevchenko V, Kovalev S, Chekhonin V, Baklaushev V, Bryukhovetskiy I and Zhukova M: To the novel paradigm of proteome-based cell therapy of tumors: Through comparative proteome mapping of tumor stem cells and tissue-specific stem cells of humans. Cell Transplant. 23 (Suppl 1):S151–S170. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Tan SH and Barker N: Wnt signaling in adult epithelial stem cells and cancer. Prog Mol Biol Transl Sci. 153:21–79. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Kahn M: Wnt signaling in stem cells and cancer stem cells: A tale of two coactivators. Prog Mol Biol Transl Sci. 153:209–244. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Kretzschmar K and Clevers H: Wnt/β-catenin signaling in adult mammalian epithelial stem cells. Dev Biol. 428:273–282. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Mohammed MK, Shao C, Wang J, Wei Q, Wang X, Collier Z, Tang S, Liu H, Zhang F, Huang J, et al: Wnt/β-catenin signaling plays an ever-expanding role in stem cell self-renewal, tumorigenesis and cancer chemoresistance. Genes Dis. 3:11–40. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Kim Y, Kim KH, Lee J, Lee YA, Kim M, Lee SJ, Park K, Yang H, Jin J, Joo KM, et al: Wnt activation is implicated in glioblastoma radioresistance. Lab Invest. 92:466–473. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Kahlert UD, Suwala AK, Koch K, Natsumeda M, Orr BA, Hayashi M, Maciaczyk J and Eberhart CG: Pharmacologic Wnt inhibition reduces proliferation, survival, and clonogenicity of glioblastoma cells. J Neuropathol Exp Neurol. 74:889–900. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Allen M, Bjerke M, Edlund H, Nelander S and Westermark B: Origin of the U87MG glioma cell line: Good news and bad news. Sci Transl Med. 8:354re32016. View Article : Google Scholar : PubMed/NCBI | |
|
Bryukhovetskiy I and Shevchenko V: Molecular mechanisms of the effect of TGF-β1 on U87 human glioblastoma cells. Oncol Lett. 12:1581–1590. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Bryukhovetskiy IS, Dyuizen IV, Shevchenko VE, Bryukhovetskiy AS, Mischenko PV, Milkina EV and Khotimchenko YS: Hematopoietic stem cells as a tool for the treatment of glioblastoma multiforme. Mol Med Rep. 14:4511–4520. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Mizrak D1, Brittan M and Alison M: CD133: Molecule of the moment. J Pathol. 214:3–9. 2008. View Article : Google Scholar : PubMed/NCBI | |
|
Shmelkov SV, St Clair R, Lyden D and Rafii S: AC133/CD133/Prominin-1. Int J Biochem Cell Biol. 37:715–719. 2005. View Article : Google Scholar : PubMed/NCBI | |
|
Zhang LS and Lum L: Chemical modulation of WNT signaling in cancer. Prog Mol Biol Transl Sci. 153:245–269. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Gong A and Huang S: FoxM1 and Wnt/β-catenin signaling in glioma stem cells. Cancer Res. 72:5658–5662. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Nikuseva-Martić T, Beros V, Pećina-Slaus N, Pećina H and Bulić-Jakus F: Genetic changes of CDH1, APC, and CTNNB1 found in human brain tumors. Pathol Res Pract. 203:779–787. 2007. View Article : Google Scholar : PubMed/NCBI | |
|
Dipro S, Al-Otaibi F, Alzahrani A, Ulhaq A and Al Shail E: Turcot syndrome: A synchronous clinical presentation of glioblastoma multiforme and adenocarcinoma of the colon. Case Rep Oncol Med. 2012:7202732012.PubMed/NCBI | |
|
Shi H, Gao Y, Tang Y, Wu Y, Gong H, Du J, Zheng B, Hu J, Shi Q and Yu R: CacyBP/SIP protein is important for the proliferation of human glioma cells. IUBMB Life. 66:286–291. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Yan S, Li A and Liu Y: CacyBP/SIP inhibits the migration and invasion behaviors of glioblastoma cells through activating Siah1 mediated ubiquitination and degradation of cytoplasmic p27. Cell Biol Int. 42:216–226. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Tang Y, Zhan W, Cao T, Tang T, Gao Y, Qiu Z, Fu C, Qian F, Yu R and Shi H: CacyBP/SIP inhibits Doxourbicin-induced apoptosis of glioma cells due to activation of ERK1/2. IUBMB Life. 68:211–219. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Chen Y, Zhang K, Wang X, Li Q, Wu Q and Ning X: Cell cycle-dependent translocation and regulatory mechanism of CacyBP/SIP in gastric cancer cells. Anticancer Drugs. 29:19–28. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Nitta RT, Gholamin S, Feroze AH, Agarwal M, Cheshier SH, Mitra SS and Li G: Casein kinase 2α regulates glioblastoma brain tumor-initiating cell growth through the β-catenin pathway. Oncogene. 34:3688–3699. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Rowse AL, Gibson SA, Meares GP, Rajbhandari R, Nozell SE, Dees KJ, Hjelmeland AB, McFarland BC and Benveniste EN: Protein kinase CK2 is important for the function of glioblastoma brain tumor initiating cells. J Neurooncol. 132:219–229. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Ferrer-Font L, Villamañan L, Arias-Ramos N, Vilardell J, Plana M, Ruzzene M, Pinna LA, Itarte E, Arús C and Candiota AP: Targeting protein kinase CK2: Evaluating CX-4945 potential for GL261 glioblastoma therapy in immunocompetent mice. Pharmaceuticals. 10(pii): E242017. View Article : Google Scholar : PubMed/NCBI | |
|
Chikano Y, Domoto T, Furuta T, Sabit H, Kitano-Tamura A, Pyko IV, Takino T, Sai Y, Hayashi Y, Sato H, et al: Glycogen synthase kinase 3β sustains invasion of glioblastoma via the focal adhesion kinase, Rac1, and c-Jun N-terminal kinase-mediated pathway. Mol Cancer Ther. 14:564–574. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Zhao P, Li Q, Shi Z, Li C, Wang L, Liu X, Jiang C, Qian X, You Y, Liu N, et al: GSK-3β regulates tumor growth and angiogenesis in human glioma cells. Oncotarget. 6:31901–31915. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Zhang Y, Wen YL, Ma JW, Ye JC, Wang X, Huang JX, Meng CY, Xu XZ, Wang SX and Zhong XY: Tetrandrine inhibits glioma stem-like cells by repressing β-catenin expression. Int J Oncol. 50:101–110. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Náger M, Santacana M, Bhardwaj D, Valls J, Ferrer I, Nogués P, Cantí C and Herreros J: Nuclear phosphorylated Y142 β-catenin accumulates in astrocytomas and glioblastomas and regulates cell invasion. Cell Cycle. 14:3644–3655. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Kahlert UD, Mooney SM, Natsumeda M, Steiger HJ and Maciaczyk J: Targeting cancer stem-like cells in glioblastoma and colorectal cancer through metabolic pathways. Int J Cancer. 140:10–22. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Kierulf-Vieira KS, Sandberg CJ, Grieg Z, Günther CC, Langmoen IA and Vik-Mo EO: Wnt inhibition is dysregulated in gliomas and its re-establishment inhibits proliferation and tumor sphere formation. Exp Cell Res. 340:53–61. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Buckley CD, Tan J, Anderson KL, Hanein D, Volkmann N, Weis WI, Nelson WJ and Dunn AR: Cell adhesion. The minimal cadherin-catenin complex binds to actin filaments under force. Science. 346:12542112014. View Article : Google Scholar : PubMed/NCBI | |
|
Ji H, Wang J, Fang B, Fang X and Lu Z: α-Catenin inhibits glioma cell migration, invasion, and proliferation by suppression of β-catenin transactivation. J Neurooncol. 103:445–451. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Xu M, Yang X, Zhao J, Zhang J, Zhang S, Huang H, Liu Y and Liu J: High expression of Cullin1 indicates poor prognosis for NSCLC patients. Pathol Res Pract. 210:397–401. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Lai YJ, Tsai JC, Tseng YT, Wu MS, Liu WS, Lam HI, Yu JH, Nozell SE and Benveniste EN: Small G protein Rac GTPases regulate the maintenance of glioblastoma stem-like cells in vitro and in vivo. Oncotarget. 8:18031–18049. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Serra N, Rosales R, Masana L and Vallvé JC: Simvastatin Increases Fibulin-2 expression in human coronary artery smooth muscle cells via RhoA/Rho-kinase signaling pathway inhibition. PLoS One. 10:e01338752015. View Article : Google Scholar : PubMed/NCBI | |
|
Sizemore ST, Zhang M, Cho JH, Sizemore GM, Hurwitz B, Kaur B, Lehman NL, Ostrowski MC, Robe PA, Miao W, et al: Pyruvate kinase M2 regulates homologous recombination-mediated DNA double-strand break repair. Cell Res. 28:1090–1102. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Wang Y, Che S, Cai G, He Y, Chen J and Xu W: Expression and prognostic significance of CTBP2 in human gliomas. Oncol Lett. 12:2429–2434. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Dcona MM, Morris BL, Ellis KC and Grossman SR: CtBP- an emerging oncogene and novel small molecule drug target: Advances in the understanding of its oncogenic action and identification of therapeutic inhibitors. Cancer Biol Ther. 18:379–391. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Patel J, Baranwal S, Love IM, Patel NJ, Grossman SR and Patel BB: Inhibition of C-terminal binding protein attenuates transcription factor 4 signaling to selectively target colon cancer stem cells. Cell Cycle. 13:3506–3518. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Guo H, Zhang XY, Peng J, Huang Y, Yang Y, Liu Y, Guo XX, Hao Q, An S and Xu TR: RUVBL1, a novel C-RAF-binding protein, activates the RAF/MEK/ERK pathway to promote lung cancer tumorigenesis. Biochem Biophys Res Commun. 498:932–939. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Matias PM, Baek SH, Bandeiras TM, Dutta A, Houry WA, Llorca O and Rosenbaum J: The AAA+ proteins Pontin and Reptin enter adult age: from understanding their basic biology to the identification of selective inhibitors. Front Mol Biosci. 2:172015. View Article : Google Scholar : PubMed/NCBI | |
|
Mao YQ and Houry WA: The role of pontin and reptin in cellular physiology and cancer etiology. Front Mol Biosci. 4:582017. View Article : Google Scholar : PubMed/NCBI |