Enhancing the therapeutic efficacy of NK cells in the treatment of ovarian cancer (Review)
- Authors:
- Published online on: January 26, 2024 https://doi.org/10.3892/or.2024.8709
- Article Number: 50
-
Copyright: © Hou et al. This is an open access article distributed under the terms of Creative Commons Attribution License.
Abstract
Introduction
Ovarian cancer is the leading cause of mortality among females diagnosed with gynecological cancer, ranking as the fifth most common cause of death in females overall. The majority of cases are detected at advanced stages of disease, resulting in unfavorable disease outcomes. Among all gynecological cancers, ovarian cancer exhibits the highest mortality rate, with a 5-year survival rate of <50% (1,2). The latest statistical study indicated that the number of patients with cancer in China exceeds 57,000, and ~27,000 new cancer-associated deaths (3). By 2023, ovarian cancer is projected to be ranked as the fifth leading cause of cancer-related mortality among females in the United States, accounting for 5% (equivalent to a total of 13,270) of all female cancer fatalities (4). In addition, results of a statistical analysis demonstrated that ~40,000 ovarian cancer-related deaths occur in females worldwide each year (5). Therefore, the development of novel innovative therapeutic strategies is required for the treatment of ovarian cancer.
Over the last two decades, adoptive immune cell therapies have been used in the clinical treatment of cancer. NK cells are cytotoxic lymphocytes of the innate immune system that eliminate cancerous cells. The application of immunotherapy mediated by NK cells has emerged as a safe and effective therapeutic approach for cancers (6). Thus, research has focused on the use of NK cells in immunotherapy. However, based on observed clinical treatment outcomes, further refinement of NK therapy is required. The development of therapies targeting NK cells generally focuses on two main aspects: i) Optimizing the quality of therapeutic NK cells through culture prescription optimization and enhancing NK cell cytotoxicity, and ii) gene editing.
The present review article highlighted the diverse approaches to enhancing NK cell properties and augmenting the corresponding antitumor efficacy. Strategies for enhancing the functionality of NK cells include cytokine-based culture prescriptions, immune-checkpoint inhibitors and gene editing techniques. In conclusion, further investigations and clinical evaluations are required to optimize the use of NK cells in cancer immunotherapy.
Additives induce the antitumor activity of NK cells
Results of previous studies demonstrated that NK cells may inhibit numerous types of tumors. To further enhance the antitumor efficacy of therapeutic NK cells, the corresponding cytotoxicity and persistence must be optimized in vivo. The use of cytokine-based agents and other drugs may provide a more stringent method for augmenting the cytotoxicity and longevity of NK cells.
Adding cytokines
Interleukin (IL)-2 has emerged as a pivotal catalyst in cancer immunotherapy, facilitating the expansion of purified NK cells (7) and activated NK cells (8). Results of a previous study revealed that interleukin-2 (IL-2) effectively augments the cytotoxicity of NK cells in the peripheral blood (9). Long-term culture with IL-2 results in a high number of functional NK cells through upregulation of NKp30 and DNAM-1 receptors on the cell (10). Furthermore, IL-2 treatment resulted in a significant expansion of NK cells and the complete regression of ovarian tumors in mice (11). Collectively, these studies highlighted the pivotal role of IL-2 in promoting the expansion of NK cells and enhancing their cytotoxic response against tumors.
Interleukin 15 (IL-15), a cytokine belonging to the common γ-chain family, exerts regulatory control over various aspects of NK cell-mediated immunity (12). Hoogstad-van et al (13) reported that the generation of NK cells in the presence of IL-15 may exert efficient cytotoxicity and interferon-γ (IFNγ) secretion towards ovarian cancer cells. In addition, NK cells actively migrate, infiltrate and execute tumor cell apoptosis within a three-dimensional multicellular ovarian cancer spheroid, thereby significantly inhibiting the progression of ovarian carcinoma in vivo (13). Moreover, IL-15 also enhances the survival of NK cells through sequestering the pro-apoptotic transcription factor FOXO3 in the cytoplasm (14). Incubation of NK cells with IL-12, IL-15 and IL-18 generates cytokine-induced memory-like NK cells. Treatment with IL-12, IL-15 and IL-18 promotes activation and proliferation of NK cells, while enhancing IFNγ production and the potent NK cell-induced inhibition of ovarian cancer (15).
Moreover, the functionality of NK cells against ovarian cancer cells was significantly enhanced following treatment with IL-15 super-agonist complexes, such as N-803 or ALT-803, which effectively promoted the proliferation of NK cells, and augmented the secretion of IFNγ, CXCL10, CD107a and TNFα (16–18). These findings demonstrated that IL-15 or IL-15 super-agonist complexes may enhance the functionality of NK cells against ovarian cancer (Fig. 1).
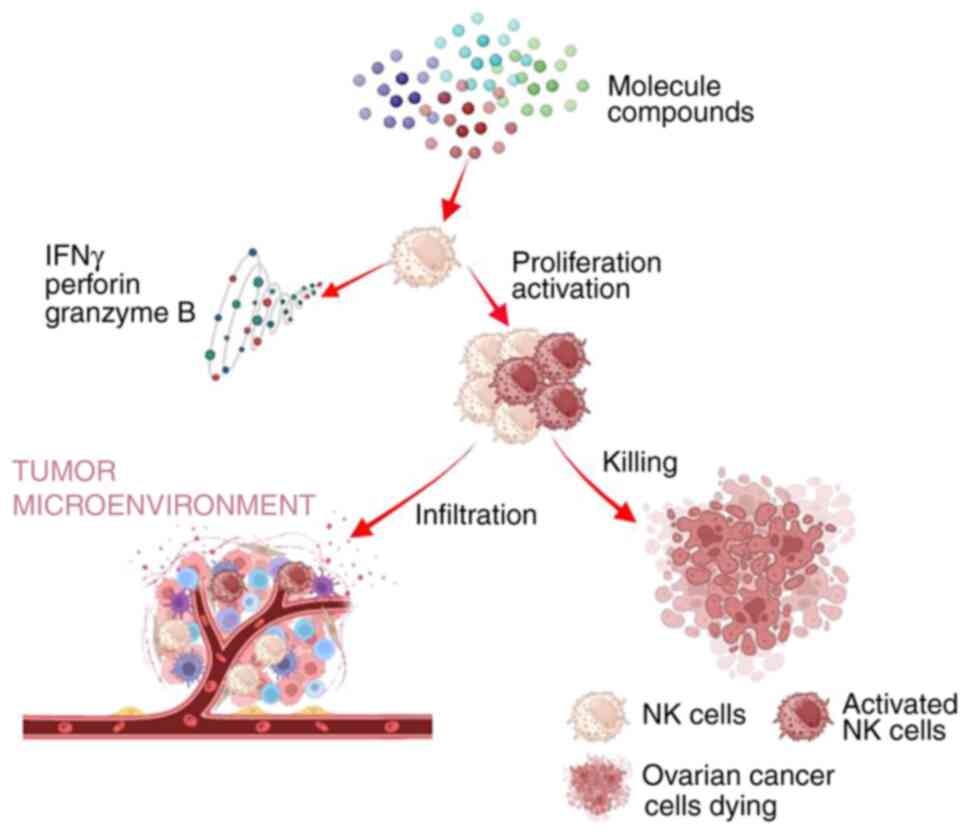
Adding molecule compounds
Results of previous studies demonstrated that certain small molecule compounds exhibit potential in enhancing the antitumor properties of NK cells. For example, cam1615B7H3 effectively promoted NK cell expansion, enhanced the antitumor activity against B7-H3+ carcinomas and inhibited the growth of aggressive ovarian cancer in vivo (19). The oncolytic therapy with HSV-1716 may enhance the antitumor immune response through promoting the recruitment of NK cells, and upregulating the expression of IFNγ, MIG and IP-10 within tumors (20). The expression of CD69 and NKG2D, as well as the secretion of IFNγ, perforin and granzyme B may be modulated by Vitamin C to enhance the properties of NK cells (21). Moreover, the streptococcal preparation, OK432, enhances the cytotoxic activity of NK cells against ovarian tumors (22). Treatment with the combination of CpG oligodeoxynucleotides and LL-37 enhanced the proliferation and activation of NK cells (23).
In addition to the aforementioned natural compounds, Choi et al (24) reported that NK cells chemically primed with 25 kDa branched polyethylenimine (25Kb PEI) exhibit increased expression of activating, adhesion and chemokine receptors. Chemically primed NK cells also promote perforin accumulation, and the subsequent migration and antitumor activity is enhanced (24). SN-38 or metformin activates NK cells to infiltrate the tumor microenvironment (TME), and secrete IFNγ and granzyme B, resulting in the elimination of cancer cells (25). Moreover, results of a previous study demonstrated that cimetidine enhanced the activity of NK cells in patients. The augmentation of NK cell function following cimetidine treatment was more pronounced in patients with a large residual tumor, compared with those without any remaining tumor (26).
In conclusion, molecular compounds play a pivotal role in augmenting the antitumor properties of NK cells, and exhibit potential as novel strategies for enhancing cancer immunotherapies (Fig. 2).
Adding natural extracts
Natural plant extracts exhibit potential in the treatment of cancer. Results of a previous study demonstrated that Ashwagandha significantly augments the population of NK cells both in stromal and intra-tumoral compartments. In addition, Ashwagandha enhances the antitumor activity of NK cells in patients with ovarian cancer (27). Moreover, the leaf extracts of L. indica and its phytoconstituent methyl gallate exhibited an augmented cytotoxic effect on ovarian tumor cells through enhancing the activity of NK cells (28). These studies may provide a basis for further clinical investigations aimed at assessing the impact of natural extracts on the immune function of NK cells in patients with cancer.
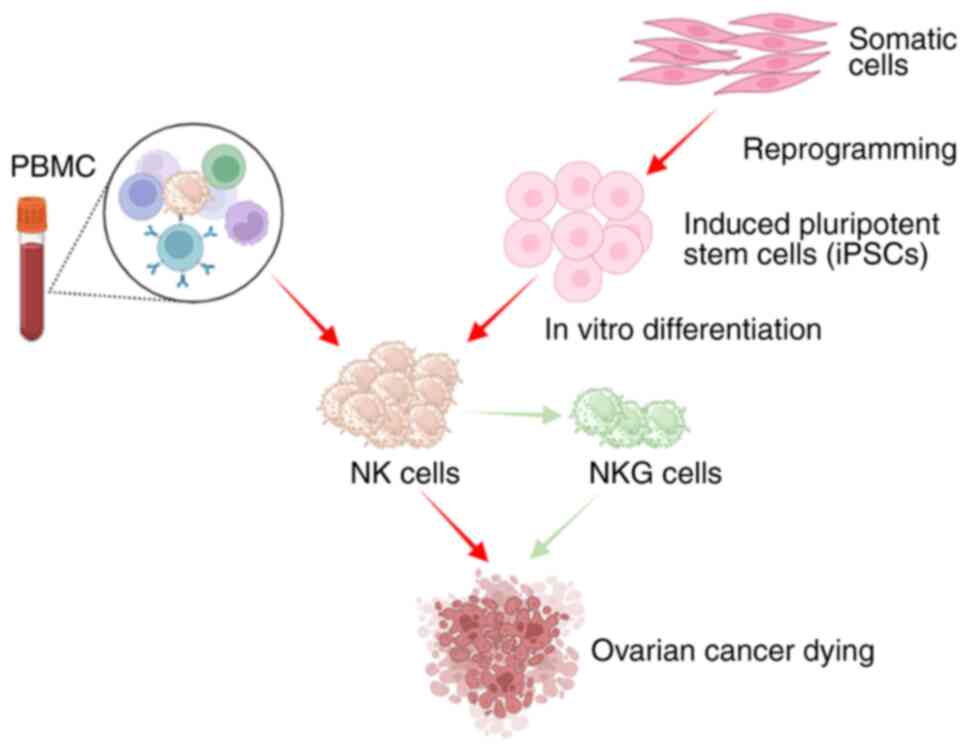
Optimizing the cell source
The proportion of functional NK cells was significantly reduced in patients with cancer (29). Thus, optimizing the source of NK cells is a pivotal determinant for the success or failure of NK cell therapy.
In patients with ovarian cancer, the cytotoxicity of NK cells in tumor-infiltrating lymphocytes was significantly lower, compared with peripheral blood mononuclear cells (PBMCs) or ascitic fluid (30). NK cells derived from PBMCs that are expanded using a feeder cell-free expansion system are referred to as eNKs, and these migrate to the tumor site while retaining cytotoxicity. Moreover, eNKs demonstrate robust proliferation capabilities, ensuring sustained high cell counts in cutaneous xenograft mice models. eNKs effectively suppress tumor growth in diverse ovarian cancer xenograft mouse models and mitigate ascites formation in peritoneal tumor models of ovarian cancer (31). Nham et al (32) used an artificial APC-based ex vivo expansion technique to produce cytotoxic, expanded NK cells from OCPs ascites-NK cells derived from patients with ovarian cancer. These NK cells exhibited increased expression of NKG2D, NKp30 and NKp44, produced increased amounts of antitumor cytokines in the presence of OC cells, and mediated direct tumor cytotoxicity against OC cells (32).
Moreover, Hermanson et al (33) revealed that induced pluripotent stem cell (iPSC)-derived NK cells demonstrate comparable anti-ovarian cancer efficacy to PBMC-NK cells, highlighting their potential as a valuable resource for ovarian cancer immunotherapy. Generating large quantities of well-characterized iPSC-derived NK cells that can be stored in biobanks may be useful in the treatment of a large group of patients (33). NKG, a novel human NK cell line, exhibited robust expression of an array of adhesive molecules, activating receptors, and cytolysis-related receptors and molecules. Irradiated NKG cells demonstrated potent cytotoxicity against ovarian cancer cells in vitro. In addition, these cells effectively suppressed human ovarian cancer growth while exhibiting a suitable safety profile in vivo; however, they did not exhibit increased proliferation (34).
These findings demonstrated the potential of NK cells in the treatment of ovarian cancers when derived from various sources (Fig. 3).
Improving the anticancer efficacy of NK cells using genetic editing
Due to the optimal recognition of cancer cells, NK cells serve as potent effector cells for adoptive cellular therapy in patients with cancer. However, the clinical application of NK cells has been significantly limited by factors such as the TME. Genetically engineered NK cells effectively address these limitations and further augment the antitumor properties of NK cells. The adoptive transfer of genetically modified NK cells for the treatment of ovarian cancer is an emerging and rapidly advancing field that has demonstrated a high level of potential.
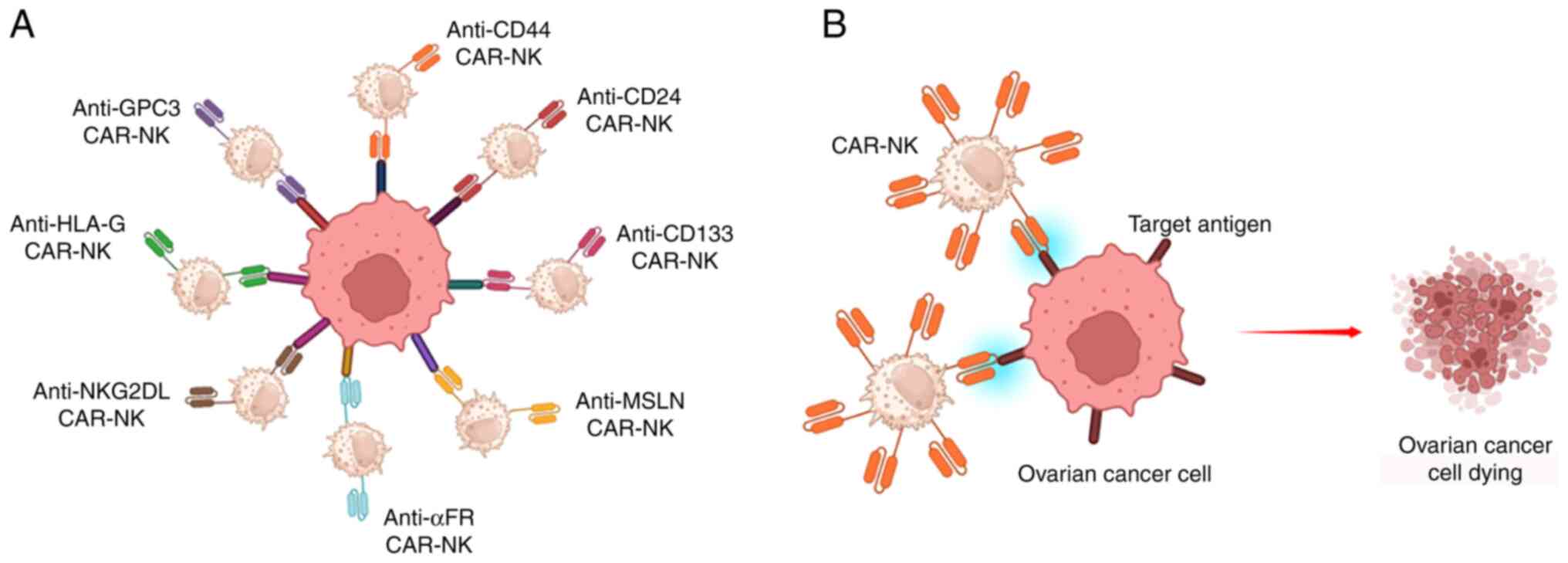
Chimeric antigen receptor (CAR)-NK cells
CARs markedly enhance the antitumor efficacy of immune effector cells. As CAR-engineered T (CAR-T) cells have demonstrated a high level of effectiveness in cancer treatment, research has focused on developing CAR-NK cells for solid tumor therapy, and diverse CAR constructs are being devised to augment NK cell-mediated cytotoxicity (Fig. 4).
CD44 is a widely expressed marker on ovarian cancer cells that is associated with properties of ovarian cancer stem cells and intraperitoneal tumor spread. CD44 demonstrated potent and specific cytotoxic activity against both CD44-positive ovarian cancer cell lines and primary ovarian cancer cells, when targeted by anti-CD44-CAR-NK. Notably, the concurrent administration of anti-CD44-CAR-NK and cisplatin exhibited enhanced antitumor efficacy compared with sequential treatment (35). Moreover, a third-generation anti-CD133-CAR-NK exhibited specific cytotoxicity against CD133-positive ovarian cancer cell lines and primary ovarian cancer cells. The targeted elimination of ovarian cancer stem cells by anti-CD133-CAR-NK exhibits potential for future clinical trials (36). Furthermore, anti-CD24-CAR-NK demonstrated potent cytotoxicity against CD24-positive ovarian cancer cell lines, and high levels of efficacy against patient-derived primary ovarian cancer cells (37).
Mesothelin (MSLN) is overexpressed in ovarian cancer, and therefore exhibits potential as a target for immunotherapy. MSLN-CAR-NK cells exhibited specific cytotoxicity against MSLN-positive ovarian cancer cells, accompanied by enhanced cytokine secretion. Moreover, in vivo studies demonstrated the effective eradication of ovarian cancer cells by MSLN-CAR-NK cells, leading to significantly prolonged survival of tumor-bearing mice (38). Folate receptor alpha (αFR) is overexpressed in 90% of ovarian cancers. Anti-αFR-CAR-NK cells exhibit specific cytotoxicity against αFR-positive ovarian cancer cells. NK cells expressing αFR-28BBζ demonstrate enhanced antigen-specific cytotoxicity, proliferation, degranulation and cytokine secretion, and reduced antigen-induced apoptosis. Moreover, anti-αFR CAR-NK cells effectively eradicate ovarian cancer cells in vivo, and significantly prolong the survival of tumor-bearing mice (39). The immune checkpoint protein, human leukocyte antigen G (HLA-G), is expressed in the majority of tumor cells as a mechanism to evade immune surveillance. Results of a previous in vitro study demonstrated that anti-HLA-G-CAR-NK cells exhibit potent cytolytic activity against ovarian cancer cells and significantly suppress xenograft tumor growth, leading to prolonged survival (40).
iPSC is a high-quality source of engineered NK cells. Li et al (41) constructed anti-hMesothelin-CAR-iPSC-NK cells, which contain the transmembrane domain of NKG2D, the 2B4 co-stimulatory domain and the CD3ζ signaling domain to mediate strong antigen-specific NK cell signaling. These cells significantly prevented ovarian cancer growth and prolonged the survival of mice with low levels of toxicity (41). In addition, anti-glypican (GPC3)-3-CAR-iPSC-NK cells exhibited consistent effector functions against GPC3-expressing tumor cells, in terms of cytotoxicity and IFN-γ production. Notably, these cells significantly prolonged the survival of mice bearing GPC3-positive ovarian-tumors (42).
Ng et al (43) constructed anti-NKG2D ligand (NKG2DL)-CAR-NK cells that expressed chemokine receptor CXCR1. Enhanced CXCR1 expression in NK cells promoted tumor trafficking and exhibited significantly augmented antitumor responses in a murine model of ovarian cancer (43).
Collectively, these findings demonstrated that the genetic engineering of NK cells may lead to the increased targeting of diverse antigens, enhance proliferation, augment tumor infiltration and selectively eliminate malignant cells. These results provide a method for improving the therapeutic efficacy of NK cells against ovarian cancer, and provide a theoretical basis for future clinical investigations.
Requisite regulation of specific target genes
The antitumor properties of NK cells are regulated by multiple genes derived from both NK cells and tumor cells. Targeted regulation of these genes markedly enhances the antitumor properties of NK cells and sensitizes tumor cells to NK cell treatment.
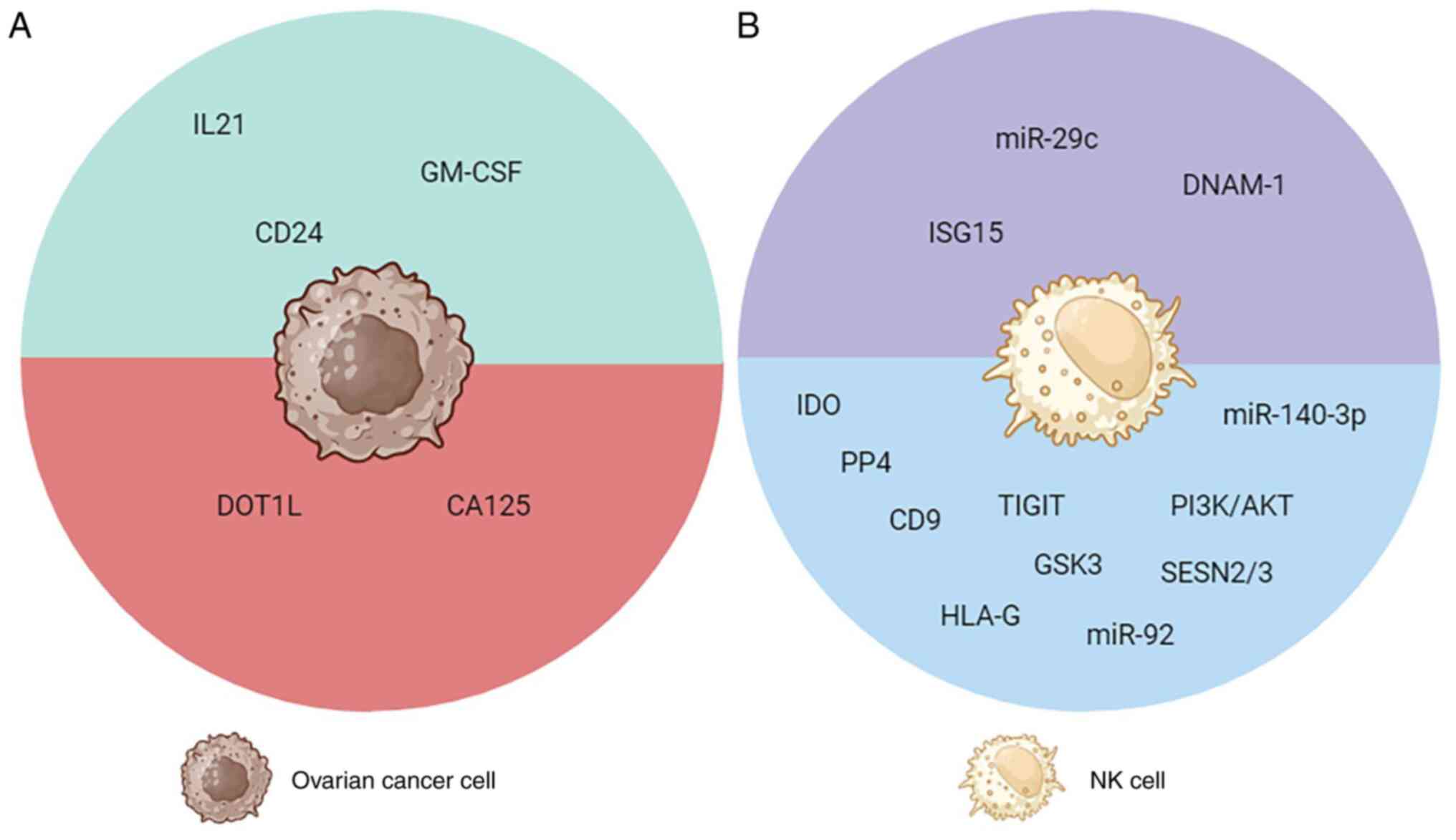
CA125, a fragment of mucin 16 shed from ovarian cancer tumors, exerts significant protective effects on ovarian tumors through evading recognition by NK cells, inhibiting the activation and cytotoxicity of NK cells, and further impairing the corresponding antitumor activity. Therefore, targeted knockdown of mucin 16 may restore the antitumor function of NK cells (44,45). In addition, the downregulation of IDO and PP4 significantly enhanced the infiltrative capacity and cytotoxicity of NK cells, thereby augmenting the anti-ovarian cancer properties (46,47). Inhibition of CD9, TIGIT, GSK3, PI3K/AKT signaling and HLA-G expression restored the cytotoxicity of NK cells against ovarian cancer (48–52). Notably, increasing the expression of NKG2DL, ULBP1, inhibited DOT1L-mediated ovarian cancer eradication, and increased the antitumor functionality of NK cells (53). Knockdown of SESN2 and SESN3 restored the tumoricidal effects of NK cells both in vitro and in vivo (54). These genes may exhibit potential as novel therapeutic targets in NK cell immunotherapy.
MicroRNAs (miRNAs) exhibit potential as therapeutic tools for restoring cellular functions. As potent genetic regulators, miRNAs effectively modulate cellular pathways through direct interactions with target genes (55). Deng et al (56) reported that miR-29c enhanced the antitumor efficacy of NK cells through directly targeting B7-H3, and mitigating NK-cell exhaustion. Conversely, treatment with miR-92 and miR-140-3p resulted in enhanced tumor growth through suppression of NK cell cytotoxicity towards ovarian cancer cells (57,58). These findings elucidated the regulatory role of miRNAs in modulating NK cell activity, and highlighted potential strategies to reactivate NK cells for ovarian cancer immunotherapy.
Dou et al (59) genetically engineered ovarian cancer cells to secrete IL-21 and GM-CSF, which enhanced NK cell cytotoxicity and elicited antitumor immunity. Moreover, interferon-stimulated gene 15 suppressed ovarian cancer progression through activation of NK cells (60). DNAM-1 signaling is essential for NK cells to recognize and target tumor cells (61). Notably, CD24+ ovarian cancer cell lines are more susceptible to NK cell lysis (62). The aforementioned findings suggested that modulation of specific genes effectively impedes the progression of ovarian cancer through the activation of NK cells, thereby highlighting the potential therapeutic value of targeting these genes for the treatment of ovarian cancer (Fig. 5).
Improving the anticancer efficacy of NK cells using combination therapy
Combination therapy has the potential to overcome deficiencies in NK cells, increase the corresponding tumor properties, reverse immunosuppression, and enhance cancer cell susceptibility to NK cell-mediated cytotoxicity.
Oncolytic virus (OV)
OVs elicit robust innate and adaptive immune responses, including contact-dependent activation of NK cells and augmentation of their cytotoxicity against adenovirus-infected ovarian cancer cells (63). Parapoxvirus ovis (Orf virus, OrfV) demonstrated significant efficacy as a monotherapy in an advanced-stage murine model of epithelial ovarian cancer. The therapeutic intervention of OrfV relied on the activation of NK cells, highlighting its potential as an immunotherapeutic agent for the treatment of advanced-stage ovarian cancer (64). These findings provided a theoretical basis for the potential clinical application of OVs in patients diagnosed with ovarian cancer (Fig. 6A).
Monoclonal antibodies (mAbs)
The cytotoxicity of NK cells may be enhanced following the addition of therapeutic mAbs that mediate antibody-dependent cellular cytotoxicity (ADCC). Zhu et al (65) revealed that when combined with anti-HER2 mAb, hnCD16-iNK cells demonstrate enhanced survival outcomes in an ovarian cancer xenograft model. Ovarian cancer cells pretreated with anti-EGFR TKIs demonstrated increased sensitivity towards NK cell-mediated ADCC (66). In addition, the potency of ADCC was further enhanced following the pre-stimulation of NK cells with monocytes and the immunostimulatory mycobacterial protein, PstS-1 (67). The combined treatment with anti-PD-L1 significantly enhanced the antitumor efficacy of NK cells (68). These findings suggested that targeted antibody therapy may confer benefits against ovarian cells by augmenting the functional capacity of supplementary cytolytic NK cells (Fig. 6B).
Small interfering (si)RNA
siRNA is derived from the mechanism of post-transcriptional gene silencing, and it exhibits high specificity and efficacy in suppressing disease-associated genes. HER-2 siRNA-treated tumor cells were efficiently lysed by NK cells in vitro, leading to a significant inhibition of xenografted tumor growth. A combination of HER-2 siRNA with NK cell therapy may exhibit potential in the biological treatment of ovarian cancer with high HER-2 expression (Fig. 6B) (69).
Chemotherapeutic drugs
The combination of NK cell adoptive transfer and tumor-sensitizing chemotherapy may exhibit potential in the treatment of ovarian cancer. In combination, NK cells and gemcitabine exhibited an additive effect in suppressing tumor growth in mice with ovarian cancer. Enhanced cytotoxicity against ovarian cancer is achieved through a synergistic combination of NK cells and gemcitabine, both in vitro and in vivo (70). Oxaliplatin, an immunogenic cell death inducer, increased the cytolysis of ovarian cancer cells mediated by NK cells (71). A combination of cisplatin and NK cell-mediated immunotherapy may overcome the immunoresistance of chemoresistant ovarian cancers (72). Results of a recent study demonstrated that SN-38 and 5-FU acted synergistically to inhibit ovarian cancer cells, and promote the sensitivity of cancer stem cells to NK cells (73). Collectively, these findings presented the potent efficacy of chemotherapeutic agents in conjunction with NK cells against therapy-resistant ovarian cancer cells, thereby establishing the viability of novel combination therapeutic strategies in the treatment of ovarian cancer (Fig. 6B).
Exosomes (EXOs) derived from NK cells
EXOs are membranous vesicles derived from cells that play a crucial role in intercellular material transportation. Moreover, they exhibit potential as drug carriers for targeted delivery to specific cell types or tissues. In addition, immune cell-derived EXOs possess immunomodulatory properties (74). NK-EXOs exhibit potent antitumor activity against ovarian cancer. Moreover, NK-EXOs serve as effective carriers for cisplatin delivery, thereby enhancing the cytotoxic effects in drug-resistant ovarian cancer cells, and reversing the immunosuppressive state of NK cells (75). Collectively, these results highlighted the potential of NK-EXOs in the clinical treatment of ovarian cancer, while also establishing a basis for further investigations into the effects of NK-EXOs in other solid tumors (Fig. 6C).
Conclusions
Ovarian cancer is a prevalent malignancy affecting females, and a lack of effective treatment options contributes to a 5-year survival rate of ~45% (76). NK cells possess distinct cytotoxic properties against cancer cells, highlighting their potential in the treatment of ovarian cancer. However, the limited clinical efficacy of NK cells poses a challenge to their application in treating ovarian cancer. In the present review, innovative strategies that aim to enhance the cytotoxicity of NK cells against ovarian cancer cells were summarized, including the utilization of additives, gene editing techniques and combination therapies.
At present, novel strategies are employed to enhance the antitumor properties of NK cells. However, limitations remain, and it is crucial to develop specific approaches for expanding functional NK cells, achieve accurate delivery of siRNA into targeted cells, and mitigate the side effects associated with combined therapy. Notably, NK cell therapy exhibits potential in the treatment of ovarian cancer. Thus, further investigations into the widespread application of NK cell adoptive transfer are required for the treatment of various solid tumors.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
YH and XN conducted project administration and acquired funding. YH, XZ and XN prepared the original draft of the manuscript. YH and XN wrote, reviewed and edited the manuscript. All authors have read and approved the final version of the manuscript. Data authentication is not applicable.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Glossary
Abbreviations
Abbreviations:
|
NK cells |
natural killer cells |
|
IL-2 |
interleukin 2 |
|
IL-15 |
interleukin 15 |
|
IFNγ |
interferon-γ |
|
TME |
tumor microenvironment |
|
PBMC |
peripheral blood mononuclear cells |
|
CARs |
Chimeric antigen receptors |
|
CAR-NK |
CAR-engineered NK |
|
MSLN |
mesothelin |
|
αFR |
folate receptor alpha |
|
HLA-G |
human leukocyte antigen G |
|
GPC3 |
glypican-3 |
|
iPSC |
induced pluripotent stem cell |
|
NKG2DL |
NKG2D ligands |
|
miRNAs |
microRNAs |
|
OV |
oncolytic viruses |
|
mAbs |
monoclonal antibodies |
|
ADCC |
antibody-dependent cellular cytotoxicity |
|
siRNA |
small interfering RNA |
|
EXO |
exosomes |
References
|
Arora T, Mullangi S and Lekkala MR: Ovarian Cancer. StatPearls StatPearls Publishing; Treasure Island: 2023 | |
|
Kuroki L and Guntupalli SR: Treatment of epithelial ovarian cancer. BMJ. 371:m37732020. View Article : Google Scholar : PubMed/NCBI | |
|
Zheng RS, Zhang SW, Sun KX, Chen R, Wang SM, Li L, Zeng HM, Wei WW and He J: Cancer statistics in China, 2016. Zhonghua Zhong Liu Za Zhi. 45:212–220. 2023.(In Chinese). PubMed/NCBI | |
|
Siegel RL, Miller KD, Wagle NS and Jemal A: Cancer statistics, 2023. CA Cancer J Clin. 73:17–48. 2023. View Article : Google Scholar : PubMed/NCBI | |
|
Penny SM: Ovarian Cancer: An Overview. Radiol Technol. 91:561–575. 2020.PubMed/NCBI | |
|
Myers JA and Miller JS: Exploring the NK cell platform for cancer immunotherapy. Nat Rev Clin Oncol. 18:85–100. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Becker PS, Suck G, Nowakowska P, Ullrich E, Seifried E, Bader P, Tonn T and Seidl C: Selection and expansion of natural killer cells for NK cell-based immunotherapy. Cancer Immunol Immunother. 65:477–484. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Geller MA, Knorr DA, Hermanson DA, Pribyl L, Bendzick L, McCullar V, Miller JS and Kaufman DS: Intraperitoneal delivery of human natural killer cells for treatment of ovarian cancer in a mouse xenograft model. Cytotherapy. 15:1297–1306. 2013. View Article : Google Scholar : PubMed/NCBI | |
|
Lotzová E, Savary CA, Freedman RS, Edwards CL and Wharton JT: Recombinant IL-2-activated NK cells mediate LAK activity against ovarian cancer. Int J Cancer. 42:225–231. 1988. View Article : Google Scholar : PubMed/NCBI | |
|
da Silva RF, Petta CA, Derchain SF, Alici E and Guimarães F: Up-regulation of DNAM-1 and NKp30, associated with improvement of NK cells activation after long-term culture of mononuclear cells from patients with ovarian neoplasia. Human Immunol. 75:777–784. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Pandey V, Oyer JL, Igarashi RY, Gitto SB, Copik AJ and Altomare DA: Anti-ovarian tumor response of donor peripheral blood mononuclear cells is due to infiltrating cytotoxic NK cells. Oncotarget. 7:7318–7328. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Ma S, Caligiuri MA and Yu J: Harnessing IL-15 signaling to potentiate NK cell-mediated cancer immunotherapy. Trends Immunol. 43:833–847. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Hoogstad-van Evert JS, Cany J, van den Brand D, Oudenampsen M, Brock R, Torensma R, Bekkers RL, Jansen JH, Massuger LF and Dolstra H: Umbilical cord blood CD34+ progenitor-derived NK cells efficiently kill ovarian cancer spheroids and intraperitoneal tumors in NOD/SCID/IL2Rgnull mice. Oncoimmunology. 6:e13206302017. View Article : Google Scholar : PubMed/NCBI | |
|
Wilson EB, El-Jawhari JJ, Neilson AL, Hall GD, Melcher AA, Meade JL and Cook GP: Human tumour immune evasion via TGF-β blocks NK cell activation but not survival allowing therapeutic restoration of Anti-Tumour activity. PLoS One. 6:e228422011. View Article : Google Scholar : PubMed/NCBI | |
|
Uppendahl LD, Felices M, Bendzick L, Ryan C, Kodal B, Hinderlie P, Boylan KLM, Skubitz APN, Miller JS and Geller MA: Cytokine-induced memory-like natural killer cells have enhanced function, proliferation, and in vivo expansion against ovarian cancer cells. Gynecol Oncol. 153:149–157. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Van der Meer JMR, Maas RJA, Guldevall K, Klarenaar K, de Jonge PKJD, Evert JSH, van der Waart AB, Cany J, Safrit JT, Lee JH, et al: IL-15 superagonist N-803 improves IFNγ production and killing of leukemia and ovarian cancer cells by CD34+ progenitor-derived NK cells. Cancer Immunol Immunother. 70:1305–1321. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Felices M, Chu S, Kodal B, Bendzick L, Ryan C, Lenvik AJ, Boylan KLM, Wong HC, Skubitz APN, Miller JS and Geller MA: IL-15 super-agonist (ALT-803) enhances natural killer (NK) cell function against ovarian cancer. Gynecol Oncol. 145:453–461. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Hoogstad-van Evert JS, Maas RJ, van der Meer J, Cany J, van der Steen S, Jansen JH, Miller JS, Bekkers R, Hobo W, Massuger L and Dolstra H: Peritoneal NK cells are responsive to IL-15 and percentages are correlated with outcome in advanced ovarian cancer patients. Oncotarget. 9:34810–34820. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Vallera DA, Ferrone S, Kodal B, Hinderlie P, Bendzick L, Ettestad B, Hallstrom C, Zorko NA, Rao A, Fujioka N, et al: NK-Cell-Mediated targeting of various solid tumors using a B7-H3 Tri-Specific killer Engager in vitro and in vivo. Cancers (Basel). 12:26592020. View Article : Google Scholar : PubMed/NCBI | |
|
Benencia F, Courrèges MC, Conejo-García JR, Mohamed-Hadley A, Zhang L, Buckanovich RJ, Carroll R, Fraser N and Coukos G: HSV oncolytic therapy upregulates interferon-inducible Chemokines and recruits immune effector cells in ovarian cancer. Mol Ther. 12:789–802. 2005. View Article : Google Scholar : PubMed/NCBI | |
|
Kim JE, Cho HS, Yang HS, Jung DJ, Hong SW, Hung CF, Lee WJ and Kim D: Depletion of ascorbic acid impairs NK cell activity against ovarian cancer in a mouse model. Immunobiology. 217:873–881. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Colotta F, Rambaldi A, Colombo N, Tabacchi L, Introna M and Mantovani A: Effect of a streptococcal preparation (OK432) on natural killer activity of tumour-associated lymphoid cells in human ovarian carcinoma and on lysis of fresh ovarian tumour cells. Br J Cancer. 48:515–525. 1983. View Article : Google Scholar : PubMed/NCBI | |
|
Chuang CM, Monie A, Wu A, Mao CP and Hung CF: Treatment with LL-37 peptide enhances antitumor effects induced by CpG oligodeoxynucleotides against ovarian cancer. Hum Gene Ther. 20:303–313. 2009. View Article : Google Scholar : PubMed/NCBI | |
|
Choi SH, Kim HJ, Park JD, Ko ES, Lee M, Lee DK, Choi JH, Jang HJ, Kim I, Jung HY, et al: Chemical priming of natural killer cells with branched polyethylenimine for cancer immunotherapy. J Immunother Cancer. 10:e0049642022. View Article : Google Scholar : PubMed/NCBI | |
|
Chung YM, Khan PP, Wang H, Tsai WB, Qiao Y, Yu B, Larrick JW and Hu MC: Sensitizing tumors to anti-PD-1 therapy by promoting NK and CD8+ T cells via pharmacological activation of FOXO3. J Immunother Cancer. 9:e0027722021. View Article : Google Scholar : PubMed/NCBI | |
|
Kikuchi Y, Oomori K, Kizawa I and Kato K: Augmented natural killer activity in ovarian cancer patients treated with cimetidine. Eur J Cancer Clin Oncol. 22:1037–1043. 1986. View Article : Google Scholar : PubMed/NCBI | |
|
Barua A, Bradaric MJ, Bitterman P, Abramowicz JS, Sharma S, Basu S, Lopez H and Bahr JM: Dietary supplementation of Ashwagandha (Withania somnifera, Dunal) enhances NK cell function in ovarian tumors in the laying hen model of spontaneous ovarian cancer. Am J Reprod Immunol. 70:538–550. 2013. View Article : Google Scholar : PubMed/NCBI | |
|
Neo SY, Siew YY, Yew HC, He Y, Poh KL, Tsai YC, Ng SL, Tan WX, Chong TI, Lim CSE, et al: Effects of Leea indica leaf extracts and its phytoconstituents on natural killer cell-mediated cytotoxicity in human ovarian cancer. BMC Complement Med Ther. 23:792023. View Article : Google Scholar : PubMed/NCBI | |
|
Yunusova NV, Stakheyeva MN, Molchanov SV, Afanas'ev SG, Tsydenova AA, Kolomiets LA and Cherdyntseva NV: Functional activity of natural killer cells in biological fluids in patients with colorectal and ovarian cancers. Cent Eur J Immunol. 43:26–32. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Lutgendorf SK, Sood AK, Anderson B, McGinn S, Maiseri H, Dao M, Sorosky JI, De Geest K, Ritchie J and Lubaroff DM: Social support, psychological distress, and natural killer cell activity in ovarian cancer. J Clin Oncol. 23:7105–7113. 2005. View Article : Google Scholar : PubMed/NCBI | |
|
Chen M, Li Y, Wu Y, Xie S, Ma J, Yue J, Lv R, Tian Z, Fang F and Xiao W: Anti-Tumor activity of expanded PBMC-Derived NK cells by feeder-free protocol in ovarian cancer. Cancers. 13:58662021. View Article : Google Scholar : PubMed/NCBI | |
|
Nham T, Poznanski SM, Fan IY, Shenouda MM, Chew MV, Lee AJ, Vahedi F, Karimi Y, Butcher M, Lee DA, et al: Ex vivo-expanded NK cells from blood and ascites of ovarian cancer patients are cytotoxic against autologous primary ovarian cancer cells. Cancer Immunol Immunother. 67:575–587. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Hermanson DL, Bendzick L, Pribyl L, McCullar V, Vogel RI, Miller JS, Geller MA and Kaufman DS: Induced Pluripotent stem Cell-Derived natural killer cells for treatment of ovarian cancer. Stem Cells. 34:93–101. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Cheng M, Ma J, Chen Y, Zhang J, Zhao W, Zhang J, Wei H, Ling B, Sun R and Tian Z: Establishment, characterization, and successful adaptive therapy against human tumors of NKG cell, a new human NK cell line. Cell Transplant. 20:1731–1746. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Klapdor R, Wang S, Morgan MA, Zimmermann K, Hachenberg J, Büning H, Dörk T, Hillemanns P and Schambach A: NK Cell-Mediated eradication of ovarian cancer cells with a novel chimeric antigen receptor directed against CD44. Biomedicines. 9:13392021. View Article : Google Scholar : PubMed/NCBI | |
|
Klapdor R, Wang S, Hacker U, Büning H, Morgan M, Dörk T, Hillemanns P and Schambach A: Improved killing of ovarian cancer stem cells by combining a novel chimeric antigen Receptor-Based immunotherapy and chemotherapy. Hum Gene Ther. 28:886–896. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Klapdor R, Wang S, Morgan M, Dörk T, Hacker U, Hillemanns P, Büning H and Schambach A: Characterization of a Novel Third-Generation Anti-CD24-CAR against ovarian cancer. Int J Mol Sci. 20:6602019. View Article : Google Scholar : PubMed/NCBI | |
|
Cao B, Liu M, Wang L, Liang B, Feng Y, Chen X, Shi Y, Zhang J, Ye X, Tian Y, et al: Use of chimeric antigen receptor NK-92 cells to target mesothelin in ovarian cancer. Biochem Biophys Res Commun. 524:96–102. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Ao X, Yang Y, Li W, Tan Y, Guo W, Ao L, He X, Wu X, Xia J, Xu X and Guo J: Anti-αFR CAR-engineered NK-92 cells display potent cytotoxicity against αFR-positive ovarian cancer. J Immunother. 42:284–296. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Jan CI, Huang SW, Canoll P, Bruce JN, Lin YC, Pan CM, Lu HM, Chiu SC and Cho DY: Targeting human leukocyte antigen G with chimeric antigen receptors of natural killer cells convert immunosuppression to ablate solid tumors. J Immunother Cancer. 9:e0030502021. View Article : Google Scholar : PubMed/NCBI | |
|
Li Y, Hermanson DL, Moriarity BS and Kaufman DS: Human iPSC-Derived natural killer cells engineered with chimeric antigen receptors enhance Anti-tumor activity. Cell Stem Cell. 23:181–192.e5. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Ueda T, Kumagai A, Iriguchi S, Yasui Y, Miyasaka T, Nakagoshi K, Nakane K, Saito K, Takahashi M, Sasaki A, et al: Non-clinical efficacy, safety and stable clinical cell processing of induced pluripotent stem cell-derived anti-glypican-3 chimeric antigen receptor-expressing natural killer/innate lymphoid cells. Cancer Sci. 111:1478–1490. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Ng YY, Tay JCK and Wang S: CXCR1 Expression to Improve Anti-cancer efficacy of intravenously injected CAR-NK cells in mice with peritoneal xenografts. Mol Ther Oncolytics. 16:75–85. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Gubbels JA, Felder M, Horibata S, Belisle JA, Kapur A, Holden H, Petrie S, Migneault M, Rancourt C, Connor JP and Patankar MS: MUC16 provides immune protection by inhibiting synapse formation between NK and ovarian tumor cells. Mol Cancer. 9:112010. View Article : Google Scholar : PubMed/NCBI | |
|
Fraser CC, Jia B, Hu G, Al Johani LI, Fritz-Klaus R, Ham JD, Fichorova RN, Elias KM, Cramer DW, Patankar MS and Chen J: Ovarian Cancer Ascites Inhibits Transcriptional Activation of NK Cells Partly through CA125. J Immunol. 208:2227–2238. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Wang D, Saga Y, Mizukami H, Sato N, Nonaka H, Fujiwara H, Takei Y, Machida S, Takikawa O, Ozawa K and Suzuki M: Indoleamine-2,3-dioxygenase, an immunosuppressive enzyme that inhibits natural killer cell function, as a useful target for ovarian cancer therapy. Int J Oncol. 40:929–934. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Raja R, Wu C, Bassoy EY, Rubino TE Jr, Utagawa EC, Magtibay PM, Butler KA and Curtis M: PP4 inhibition sensitizes ovarian cancer to NK cell-mediated cytotoxicity via STAT1 activation and inflammatory signaling. J Immunother Cancer. 10:e0050262022. View Article : Google Scholar : PubMed/NCBI | |
|
Gonzalez VD, Huang YW, Delgado-Gonzalez A, Chen SY, Donoso K, Sachs K, Gentles AJ, Allard GM, Kolahi KS, Howitt BE, et al: High-grade serous ovarian tumor cells modulate NK cell function to create an immune-tolerant microenvironment. Cell Rep. 36:1096322021. View Article : Google Scholar : PubMed/NCBI | |
|
Maas RJ, Hoogstad-van Evert JS, Van der Meer JM, Mekers V, Rezaeifard S, Korman AJ, de Jonge PK, Cany J, Woestenenk R, Schaap NP, et al: TIGIT blockade enhances functionality of peritoneal NK cells with altered expression of DNAM-1/TIGIT/CD96 checkpoint molecules in ovarian cancer. Oncoimmunology. 9:18432472020. View Article : Google Scholar : PubMed/NCBI | |
|
Cichocki F, Valamehr B, Bjordahl R, Zhang B, Rezner B, Rogers P, Gaidarova S, Moreno S, Tuininga K, Dougherty P, et al: GSK3 inhibition drives maturation of NK cells and enhances their antitumor activity. Cancer Res. 77:5664–5675. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Hahne JC, Kurz A, Meyer SR, Dietl J, Engel JB and Honig A: Anti-tumour activity of phosphoinositide-3-kinase antagonist AEZS-126 in models of ovarian cancer. Arch Gynecol Obstet. 291:131–141. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Lin A, Yan WH, Xu HH, Gan MF, Cai JF, Zhu M and Zhou MY: HLA-G expression in human ovarian carcinoma counteracts NK cell function. Ann Oncol. 18:1804–1809. 2007. View Article : Google Scholar : PubMed/NCBI | |
|
Chava S, Bugide S, Edwards YJK and Gupta R: Disruptor of telomeric silencing 1-like promotes ovarian cancer tumor growth by stimulating pro-tumorigenic metabolic pathways and blocking apoptosis. Oncogenesis. 10:482021. View Article : Google Scholar : PubMed/NCBI | |
|
Wang X, Liu W, Zhuang D, Hong S and Chen J: Sestrin2 and sestrin3 suppress NK-92 cell-mediated cytotoxic activity on ovarian cancer cells through AMPK and mTORC1 signaling. Oncotarget. 8:90132–90143. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Diener C, Keller A and Meese E: Emerging concepts of miRNA therapeutics: From cells to clinic. Trends Genet. 38:613–626. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Deng M, Wu D, Zhang Y, Jin Z and Miao J: MiR-29c downregulates tumor-expressed B7-H3 to mediate the antitumor NK-cell functions in ovarian cancer. Gynecol Oncol. 162:190–199. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Feng S, Sun H and Zhu W: MiR-92 overexpression suppresses immune cell function in ovarian cancer via LATS2/YAP1/PD-L1 pathway. Clin Transl Oncol. 23:450–458. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Wang J, Zhu M, Zhou X, Wang T, Xi Y, Jing Z and Xi W: MiR-140-3p inhibits natural killer cytotoxicity to human ovarian cancer via targeting MAPK1. J Biosci. 45:662020. View Article : Google Scholar : PubMed/NCBI | |
|
Dou J, Wang Y, Wang J, Zhao F, Li Y, Cao M, Hu W, Hu K, He XF, Chu L, et al: Antitumor efficacy induced by human ovarian cancer cells secreting IL-21 alone or combination with GM-CSF cytokines in nude mice model. Immunobiology. 214:483–492. 2009. View Article : Google Scholar : PubMed/NCBI | |
|
Yeung TL, Tsai CC, Leung CS, Au Yeung CL, Thompson MS, Lu KH, Freedman RS, Birrer MJ, Wong KK, Mok SC, et al: ISG15 Promotes ERK1 ISGylation, CD8+ T cell activation and suppresses ovarian cancer progression. Cancers (Basel). 10:4642018. View Article : Google Scholar : PubMed/NCBI | |
|
Labani-Motlagh A, Israelsson P, Ottander U, Lundin E, Nagaev I, Nagaeva O, Dehlin E, Baranov V and Mincheva-Nilsson L: Differential expression of ligands for NKG2D and DNAM-1 receptors by epithelial ovarian cancer-derived exosomes and its influence on NK cell cytotoxicity. Tumour Biol. 37:5455–5466. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Koh J, Lee SB, Park H, Lee HJ, Cho NH and Kim J: Susceptibility of CD24(+) ovarian cancer cells to anti-cancer drugs and natural killer cells. Biochem Biophys Res Commun. 427:373–378. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Leung EYL, Ennis DP, Kennedy PR, Hansell C, Dowson S, Farquharson M, Spiliopoulou P, Nautiyal J, McNamara S, Carlin LM, et al: NK cells augment oncolytic adenovirus cytotoxicity in ovarian cancer. Mol Ther Oncolytics. 16:289–301. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
van Vloten JP, Matuszewska K, Minow MAA, Minott JA, Santry LA, Pereira M, Stegelmeier AA, McAusland TM, Klafuric EM, Karimi K, et al: Oncolytic Orf virus licenses NK cells via cDC1 to activate innate and adaptive antitumor mechanisms and extends survival in a murine model of late-stage ovarian cancer. J Immunother Cancer. 10:e0043352022. View Article : Google Scholar : PubMed/NCBI | |
|
Zhu H, Blum RH, Bjordahl R, Gaidarova S, Rogers P, Lee TT, Abujarour R, Bonello GB, Wu J, Tsai PF, et al: Pluripotent stem cell-derived NK cells with high-affinity noncleavable CD16a mediate improved antitumor activity. Blood. 135:399–410. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Mallmann-Gottschalk N, Sax Y, Kimmig R, Lang S and Brandau S: EGFR-Specific tyrosine kinase inhibitor modifies NK Cell-Mediated antitumoral activity against ovarian cancer cells. Int J Mol Sci. 20:46932019. View Article : Google Scholar : PubMed/NCBI | |
|
Gottschalk N, Kimmig R, Lang S, Singh M and Brandau S: Anti-epidermal growth factor receptor (EGFR) antibodies overcome resistance of ovarian cancer cells to targeted therapy and natural cytotoxicity. Int J Mol Sci. 13:12000–12016. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Oyer JL, Gitto SB, Altomare DA and Copik AJ: PD-L1 blockade enhances anti-tumor efficacy of NK cells. Oncoimmunology. 7:e15098192018. View Article : Google Scholar : PubMed/NCBI | |
|
Zhou Y, Cheng Z, Zhu H, Feng D, Zhao W, Ling B, Wei H and Tian Z: Stable suppression of HER-2 gene expression using siRNA increases the lysis of human ovarian carcinoma cells mediated by NK-92 cell line. Oncol Rep. 20:1425–1431. 2008.PubMed/NCBI | |
|
Van der Meer JMR, de Jonge P, van der Waart AB, Geerlings AC, Moonen JP, Brummelman J, de Klein J, Vermeulen MC, Maas RJA, Schaap NPM, et al: CD34+ progenitor-derived NK cell and gemcitabine combination therapy increases killing of ovarian cancer cells in NOD/SCID/IL2Rgnull mice. Oncoimmunology. 10:19810492021. View Article : Google Scholar : PubMed/NCBI | |
|
Siew YY, Neo SY, Yew HC, Lim SW, Ng YC, Lew SM, Seetoh WG, Seow SV and Koh HL: Oxaliplatin regulates expression of stress ligands in ovarian cancer cells and modulates their susceptibility to natural killer cell-mediated cytotoxicity. Int Immunol. 27:621–632. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Choi SH, Jung D, Kim KY, An HJ and Park KS: Combined use of cisplatin plus natural killer cells overcomes immunoresistance of cisplatin resistant ovarian cancer. Biochem Biophys Res Commun. 563:40–46. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Li G, Nikkhoi SK and Hatefi A: Stem cell-assisted enzyme/prodrug therapy makes drug-resistant ovarian cancer cells vulnerable to natural killer cells through upregulation of NKG2D ligands. Med Oncol. 40:1102023. View Article : Google Scholar : PubMed/NCBI | |
|
Liang Y, Duan L, Lu J and Xia J: Engineering exosomes for targeted drug delivery. Theranostics. 11:3183–3195. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Luo H, Zhou Y, Zhang J, Zhang Y, Long S, Lin X, Yang A, Duan J, Yang N, Yang Z, et al: NK cell-derived exosomes enhance the anti-tumor effects against ovarian cancer by delivering cisplatin and reactivating NK cell functions. Front Immunol. 13:10876892022. View Article : Google Scholar : PubMed/NCBI | |
|
Yoon H, Kim A and Jang H: Immunotherapeutic approaches in ovarian cancer. Curr Issues Mol Biol. 45:1233–1249. 2023. View Article : Google Scholar : PubMed/NCBI |