Expression of programmed death ligand 1 in patients with triple‑negative breast cancer: Association with clinicopathological parameters
- Authors:
- Published online on: June 25, 2024 https://doi.org/10.3892/wasj.2024.259
- Article Number: 44
-
Copyright : © Hasan et al. This is an open access article distributed under the terms of Creative Commons Attribution License [CC BY 4.0].
Abstract
Introduction
Globally, breast cancer ranks highest among all types of malignancies. It is the primary cause of malignancy-related mortality among individuals between the ages of 50 and 55 years. Breast cancer worldwide accounts for ~22% of all cancers affecting women (1). In Iraq, breast cancer has exhibited a significant increase over the past two decades, rendering it the most prevalent type of cancer among women. It constitutes ~50% of all female cancers, followed by thyroid, colon, central nervous system and lung cancers (2-4). Triple-negative breast cancer (TNBC) constitutes 15 to 20% of all cases of breast cancer. This subtype is characterized by the absence of estrogen receptor (ER) and progesterone receptor (PR), as well as human epidermal growth factor receptor-2 (HER-2) (5). This subtype is distinguished from others by a worse prognosis, a higher relapse probability and an earlier age of onset (6,7). Targeted therapies against HER-2 and endocrine medicines can be beneficial for subtypes that test positive for HER-2 and hormone receptors. However, adjuvant and neoadjuvant cytotoxic chemotherapy is commonly employed for the treatment of patients with TNBC. Given the low efficacy and high frequency of harmful side-effects of chemotherapy, it is clear that more targeted therapeutic techniques are required to treat this type of cancer (8). An increasingly common type of immunotherapy, using immune checkpoint inhibitors (ICIs) is finding an increasing number of applications in major therapeutic contexts. Tumor cells can evade immune surveillance by employing immunological checkpoints, the activation of coinhibitory signaling pathways, and promoting immune tolerance. There is presently a notable inclination towards investigating therapeutic alternatives for TNBC through the utilization of ICIs, particularly those that directly target the programmed cell death 1 (PD-1) and programmed death ligand 1 (PD-L1) pathways. Depending on the expression of PD-L1, the use of this type of therapy is commonly advised (8-10). Significant therapeutic advantages have been demonstrated in bladder, lung, skin and kidney malignancies with PD-1/PD-L1 inhibitors (11). There is strong evidence to indicate that immunotherapy has a higher response rate in TNBC compared to other subtypes of breast cancer. This is due to the fact that TNBC is usually characterized by an increased number of mutations, a relatively high expression of PD-L1, and a larger abundance of tumor-infiltrating lymphocytes (TILs) (12). In addition, improved results are observed with higher TIL levels in TNBC (13). Using PD-1/PD-L1 inhibitors as a tactic for combating TNBC is possible, as ICIs can accelerate the elimination process of the immune system (14). Using atezolizumab combined with nab-paclitaxel in treatment of the cases of metastatic TNBC (mTNBC) cases that are positive for PD-L1 expression was approved in 2019 by the European Commission and the Food and Drug Administration (FDA). Next to this license, the first immunotherapy protocol for the treatment of breast cancer was authorized (15). After the promising outcomes in treating mTNBC, researchers investigated the use of the PD-1/PD-L1 monoclonal antibodies for the treatment of early-stage TNBC. More encouraging results have surfaced as of late (16-18). A combination of basic research and clinical trials is required for the effective use of PD-1/PD-L1 inhibitors in early-stage TNBC (11).
Key tenets of PD-1/PD-L1 inhibition
PD-1 and PD-L1, which are transmembrane proteins, have been classified as immunoglobulin (Ig) superfamily members. The activated T-cell membrane surface exhibits the presence of PD-1(13). The existence of PD-L1 in normal tissue has been well-reported, as it functions as the ligand for PD-1. Interactions between PD-1 and PD-L1 decrease the activity of T-cells, resulting in immunological tolerance. The PD-1/PD-L1 pathway plays a central role in maintaining the equilibrium in the body's immune system (19). The aberrant expression of PD-L1 has been observed in several types of cancer, including lung, colorectal and breast cancers, and melanoma. There is a potential association between the cytokines present in the tumor microenvironment (TME), specifically interferon (IFN) (20). IFN serves as the primary soluble cytokine responsible for inducing the production of PD-L1 in tumor cells as part of an immune response. The elevated production of transcription factors in cancer cells leads to the upregulation of PD-L1 transcription and translation, facilitated by the binding of IFN to its receptor (20). The activation of PD-1 and PD-L1 inhibits lymphocyte proliferation via T-cell receptors. Immunosurveillance is initiated. As the expression of PD-L1 increases in malignancies, the TME may become more immunosuppressive (21). Interfering with these co-inhibitory pathways has been shown to be effective in the treatment of various types of cancer. For instance, previous research has demonstrated that the inhibition of the interaction between PD-1 and PD-L1 enhances the T-cell immune response. This objective can be achieved through several mechanisms: i) Stimulating and invigorating lymphocyte activity and the secretion of cytotoxic cytokines; ii) proliferating and activating CD8+ T-cells that exhibit specificity towards tumor antigens; iii) inhibiting lymphocyte apoptosis induced by the PD-1/PD-L1 interaction; and iv) augmenting the capacity of the immune system to differentiate tumor cells (22).
Recent studies have provided evidence that the inclusion of atezolizumab or pembrolizumab, which specifically target PD-L1 or PD-1, in chemotherapeutic regimens leads to enhanced outcomes in patients with both early-stage TNBC and mTNBC (23,24). Among patients diagnosed with mTNBC, the combined use of atezolizumab with nab-paclitaxel has demonstrated a statistically significant benefit in progression-free survival (PFS) and a clinically significant benefit in overall survival. The observed advantage was found when comparing the effects of nab-paclitaxel in patients who tested positive for PD-L1(25), which refers to tumor-infiltrating immune cells that express PD-L1 and cover a minimum of 1% of the tumor area (19). The aforementioned discoveries have resulted in a significant shift in the worldwide benchmarks of healthcare. In patients with tumors positive for PD-L1, and who exhibit a combined positive score (CPS) of at least 10, the administration of pembrolizumab, either in combination with gemcitabine or taxane plus carboplatin, has been demonstrated to lead to a greater benefit in PFS when compared to a placebo combination with chemotherapy. The calculation of the CPS score involves dividing the aggregate count of tumor cells, lymphocytes and macrophages expressing PD-L1 by the overall count of viable tumor cells (23). By contrast, it was observed that the occurrence of a pathological complete response was not influenced by the presence of the PD-L1 status when atezolizumab or pembrolizumab was administered alongside neoadjuvant chemotherapy regimens in the early stage of TNBC (24). This finding implies that evaluating the PD-L1 status may have diminished importance in this particular scenario (24).
Therefore, the assessment of PD-L1 expression in the TNBC is increasingly being incorporated into normal pathological procedures and has become a customary approach in the management of mTNBC. Currently, there is a notable focus on the utilization of PD-L1-targeted therapy in the clinical trials of the Iraqi nation (not registered online yet), particularly in the context of ICIs. The objective of the present study is to investigate the immunohistological analysis of PD-L1 expression in TNBC and to identify the clinicopathological characteristics that can be used to predict positivity. This may enable the publication of an Iraqi data-driven analysis on an intriguing and innovative subject in clinical oncology.
Materials and methods
Study design
The present retrospective study included 40 histological materials provided by core needle biopsies under ultrasound guidance from women with TNBC, together with their relevant pathological reports. The samples were collected from the Pathology Department of Al-Massa Private Center in Baghdad (Iraq) during the period from January, 2021 to December, 2023. The histological materials were formalin-fixed paraffin-embedded tissue blocks of TNBC. The following data were extracted from the pathological reports: The age of the patients, breast laterality, histological grade, calcification, necrosis and cytological reports provided by fine needle aspiration under an ultrasound guide for any radiologically suspicious axillary lymph node status at presentation. The present study was approved by the Al-Massa Center's Ethical Committee (reference no. 141412-23), and it followed its institutional policy. Consent to participate was deemed not applicable as the present study was a retrospective study using data with no violation of patient privacy.
Sample selection
The inclusion criterion was histological materials of breast cancer that were triple-negative for immunohistochemical tests (ER, PR and HER2\NEU) and had complete radiological, histological and cytological reported data in the patient's pathological report in a single center. The exclusion criteria included the following: Histological materials of breast cancer that were positive for one or more of the following immunohistochemical tests: ER, PR and HER2\NEU; those with missing or incomplete relevant data; invalid PDL1 tests; i.e., histological samples that were not compatible with theappropriate PD-L1 test.
Immunohistochemistry
Formalin-fixed paraffin-embedded blocks were submitted for immunohistochemistry. Fixation was performed with 10% neutral-buffered formalin (Pandora Industries Pvt. Ltd.) was 48 h at room temperature. A 4-µM-thick tissue section was created, adhered to a charged slide, and then dried for 30 min at 62˚C. The samples underwent standard heat epitope retrieval at pH 8.0 for 30 min in ethylene diamine tetraacetic acid (Unilong Industry Co., Ltd.). Subsequently, incubation with primary PD-L1 antibody using anti-human PDL1 (PathnSitu Biotechnologies, PDL1-clone B7H1P; isotype monoclonal rabbit IgG; cat. no. PR303) was performed, followed by non-biotinylated anti-mouse immunoglobulin, and peroxidase-labeled streptavidin (PathnSitu Biotechnologies; cat. no. OSH001, 6 ml; ready-to-use). Harris hematoxylin (PathnSitu Biotechnologies; cat. no. PS021 served as the counterstain for the slides by covering tissue sections for 8-10 min at room temperature. The optimal concentrations for the primary antibody and the incubation time were applied according to the specific instructions provided by PathnSitu Biotechnologies, the manufacturer of the product. The recommended dilution was 1:50-1:100 and the incubation time was 30-60 min at room temperature. Graded alcohols and xylenes (Greenwell Biotech/India) were applied, followed by cover-slipping. Each run was conducted with the inclusion of both positive and negative external controls; the positive external control was splenic tissue, while the negative external control was a known case of PD-L1-negative breast cancer. The examination of the staining results was performed using a light microscope (Leica Microsystem GmbH).
Data interpretation
The interpretation of the results was carried out by two independent pathologists in a blinded manner. The assessment of PD-L1 expression was achieved by using the CPS. It was obtained by calculating the number of cells that stained positive (membranous and/or cytoplasmic) with PD-L1, which included tumor cells, lymphocytes and macrophages, divided by the total number of viable tumor cells, then multiplied by 100. The specimen was regarded as having PD-L1 expression if the CPS was ≥10. Accordingly, the total sample was divided into two groups as follows: CPS <10 and CPS ≥10. Each histological sample should contain at least 100 viable tumor cells; degenerated or necrotic cells were excluded (26). Photomicrographs were obtained using a Leica ICC 50E camera (Leica Microsystem GmbH).
Statistical analysis
The analysis of the data in the present study was performed using the Statistical Package for Social Sciences (SPSS) version 25 (IBM Corp.). The range of the patient's age is presented as the mean ± standard deviation (SD). Comparisons between PD-L1 expression and histological grade, calcification, necrosis and axillary lymph node status at presentation were achieved using Fisher's exact and Chi-squared tests. A P-value <0.05 was considered to indicate a statistically significant difference.
Results
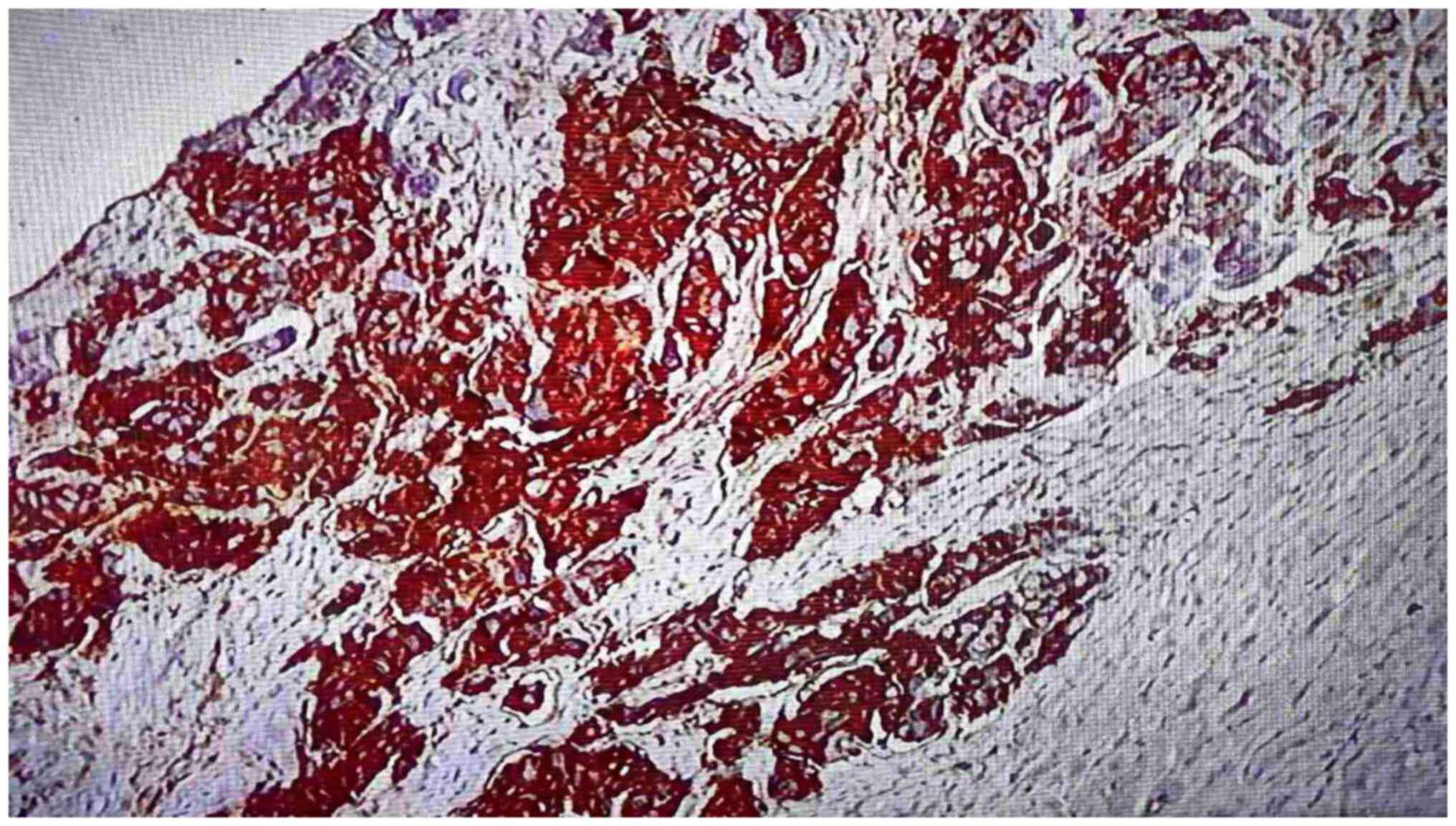
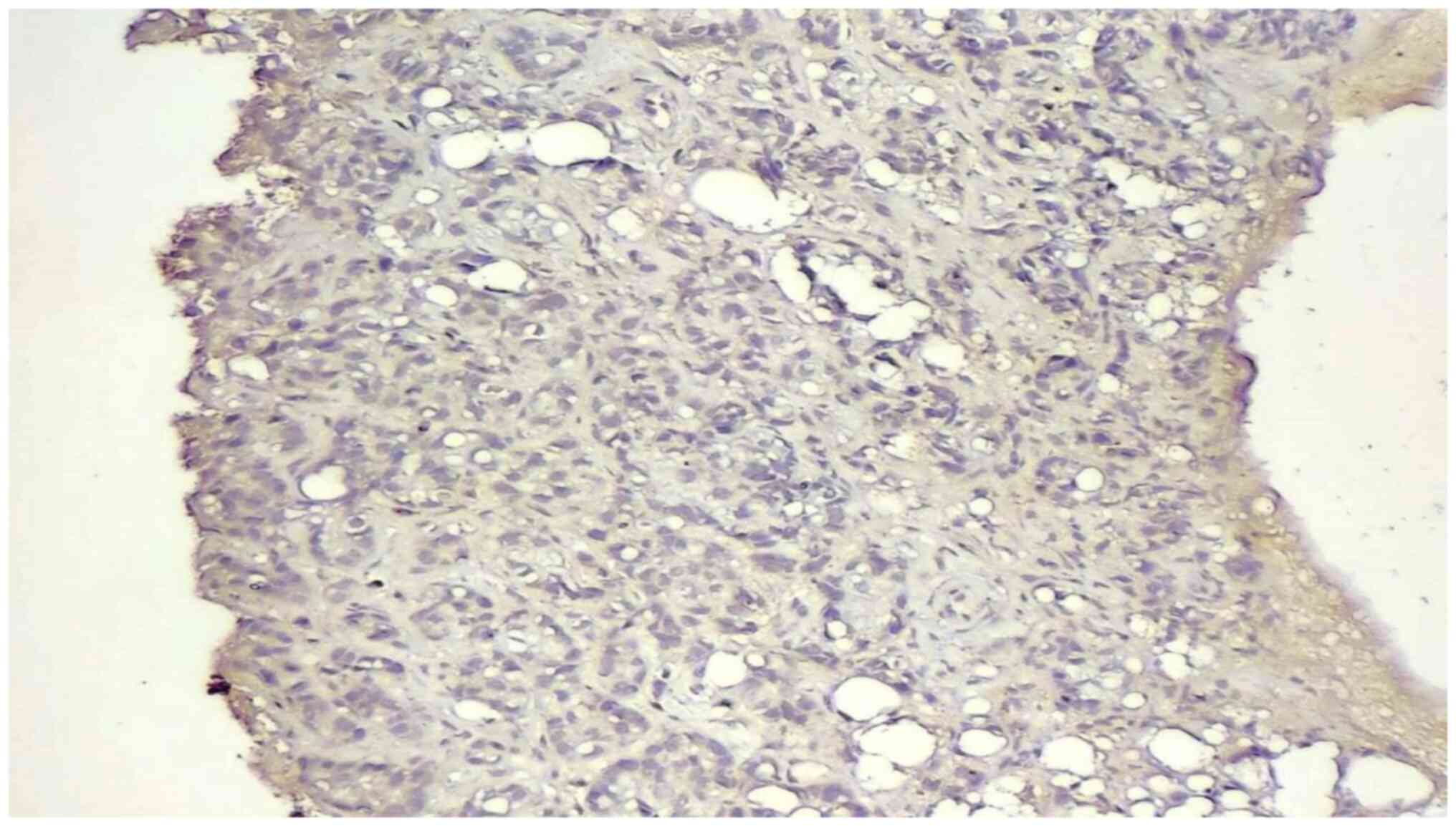
The present study used 40 histological samples of TNBC; 20 were from the right breast and 20 were from the left one; the age range of the patients was from 39 to 78 years. The mean age was 62.825±3.12 years. Of the total number of samples, 16 (40%) were grade I, 8 (20%) were grade II, and 16 (40%) were grade III. Positivity for PD-L1 was found in 24 (60%) of the total number of samples (Figs. 1 and 2). Negativity was observed in 16 (40%) cases (Fig. 3). The mean number of PD-L1-positive cases was 37.8333±21.85. There was a non-statistically significant association between PD-L1 positivity, histological grade and the presence of tissue necrosis. A statistically significant association was found between PD-L1 positivity and the presence of calcification and positive axillary lymph node status at presentation (Table I).
Table IAssociation between PD-L1 expression and histological grade, necrosis, calcification and positive axillary lymph node status at presentation in patients with TNBC. |
Discussion
Although PD-L1 expression is considered a biomarker of response to anti-PD-L1 immunotherapy, the prognostic value of PD-L1 expression in invasive mammary carcinoma remains an issue of debate in clinical oncology, given the presence of a number of different commercially available immunohistochemical clones, variable cut-off points and scoring systems that have been used among all the published data concerning PD-L1 expression in breast cancer (27).
The present study demonstrated that PDL1 expression was present in 60% (24 out of 40) of TNBC samples. There is conflicting recorded data in the literature in this regard; thus, it is irrational to compare the results across studies with a similar aim (22,24,28-31). Different results among these publications are due to variations in methods of detection of PD-L1 expression, the use of microarray techniques, and differences in the applied immunohistochemical clones and scoring systems. In the literature, the recorded cut-off was from 1 to 50%; 1% cut-off scores and (0-3 score) graded scoring systems were frequently applied to test PD-L1 expression in human cancers in the majority of published studies. This variation could affect the prevalence of PD-L1 positivity among these studies (32). Gonzalez-Ericsson et al (33) and Vlajnic et al (8) investigated the differences in the results of PD-L1 expression among three different PD-L1 immunohistochemical clones in TNBC, and confirmed that the use of different PD-L1 immunohistochemical clones was responsible for considerable discrepancies in the results of PD-L1 expression. The present study used a relatively low-cost, frequently used commercially available clone in Iraq.
There is ample number of studies in the literature focusing on the clinical characteristics of PD-L1 expression in TNBC. The present study aimed to investigate the pathological characterization of PD-L1 expression in this aggressive category of breast cancer, which thus clarifies the novelty of the present study. The present study demonstrated that there was a non-statistically significant association between PD-L1 expression, histological grade and the presence of tissue necrosis. However, a statistically significant association was found between PD-L1 expression, tissue calcification and positive cytology for axillary lymph node status at presentation. A similar Iraqi study performed by Keorges (26), which used an approximately similar sample size (n=44) and a similar score (CPS), but with a different PD-L1 clone (Dako kits, PD-L1, clone 22C3), demonstrated that there was a non-statistically significant association between PD-L1 expression, histological grade and positive axillary lymph node status. However, the criteria for the inclusion of samples with associated positive axillary lymph node status were not specified by the author in that study, whether by radiology, fine needle aspiration cytology, or excisional biopsy. This may contribute to the disagreement that was found with the results of the present study. Furthermore, unlike the present study, the study by Keorges (26) found a low prevalence of PD-L1 positivity in TNBC at 25%, despite using the same CPS cut-off value. There are two PD-L1 clones commercially available and these are more frequently used in routine testing (Dako, 22C3, and PathnSitu Biotechnologies, B7H1P). Thus, based on the results, considerable disagreement was present in the results of PD-L1 expression between these popular clones.
The statistically significant association observed in the present study between PD-L1 expression, the presence of tissue calcification and positive axillary lymph node cytology raises a concern about using pathological characteristics either to select or to exclude patients from PD-L1 testing. However, to the best of our knowledge, there are no published studies available to date investigating the association of PD-L1 expression with tissue necrosis and calcification for comparison and discussion.
Further and more extensive investigations are warranted in order to determine the optimal cut-off value and select the optimal clone to apply as a gold standard for PD-L1 testing in TNBC, following confirmation by future life expectancy analyses.
The present study had certain limitations which should be mentioned. The present study was a single-center study with a small number of cases, and examined a cancer subtype with a relatively low prevalence rate. In addition, an immunohistochemical test was used that has a decreasing validity in a very old specimen; very old blocks that were stored for a number of years were avoided in such a retrospective analysis, which may have led to a considerable effect on the sample size. Another limitation is related to a lack of clinical information as with any retrospective analysis.
In conclusion, the present study demonstrates that PD-L1 expression is present at a relatively high prevalence rate in TNBC; thus, it is rational to examine PDL1 expression in TNBC. Pathological characteristics can be used for selecting and excluding patients from PD-L1 testing.
Acknowledgements
The authors would like to thank the Pathology Department of Al-Massa Private Center in Baghdad, Iraq for their great support in data collection.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
FFH, AFH and AQY were involved in the conception and design of the study, and in the analysis and interpretation of the results. MHF and FFH were involved in data collection. AQY, FFH and AFH were involved in the preparation of the draft of the manuscript. MHF and AFH confirm the authenticity of all the raw data. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
On December 19, 2023, the Al-Massa Center's Ethical Committee approved the study (reference no. 141412-23), and it followed its institutional policy. Consent to participate was deemed not applicable as this was a retrospective study using data with no violation of patient privacy.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
|
Dawson AE and Mulford DK: Benign versus malignant papillary neoplasms of the breast. Diagnostic clues in fine-needle aspiration cytology. Acta Cytol. 80:23–28. 1994.PubMed/NCBI | |
|
Lafta RK: Health System in Iraq Post-2003 War. Al-Kindy Col Med J. 19:5–11. 2023. | |
|
Sahu N, Agrahari AK, Parida B and Das S: Radiological Significance of Shear-Wave Elastography Technique for Evaluation of Solid Breast Masses with Histopathological Correlation. Al-Kindy Col Med J. 19:26–30. 2023. | |
|
Aswad N and Abedtwfeq RH: Ultrasound-guided Core Needle Biopsy in the Diagnosis of Suspicious Breast Lesions: Radiologist's Perspectives. Al-Kindy Col Med J. 19:22–29. 2023. | |
|
Foulkes WD, Smith IE and Reis-Filho JS: Triple-negative breast cancer. N Engl J Med. 363:1938–1948. 2010.PubMed/NCBI View Article : Google Scholar | |
|
Garrido-Castro AC, Lin NU and Polyak K: Insights into molecular classifications of triple-negative breast cancer: Improving patient selection for treatment. Cancer Discov. 9:176–198. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Borri F and Granaglia A: Pathology of triple-negative breast cancer. Semin Cancer Biol. 72:136–145. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Vlajnic T, Baur F, Soysal SD, Weber WP, Piscuoglio S and Muenst S: PD-L1 expression in triple-negative breast cancer: A comparative study of 3 different antibodies. Appl Immunohistochem Mol Morphol. 30:726–730. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Li CH, Karantza V, Aktan G and Lala M: Current treatment landscape for patients with locally recurrent inoperable or metastatic triple-negative breast cancer: A systematic literature review. Breast Cancer Res. 21(143)2019.PubMed/NCBI View Article : Google Scholar | |
|
Galluzzi L, Humeau J, Buque A, Zitvogel L and Kroemer G: Immunostimulation with chemotherapy in the era of immune checkpoint inhibitors. Nat Rev Clin Oncol. 17:725–741. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Yang T, Li W, Huang T and Zhou J: Immunotherapy Targeting PD-1/PD-L1 in Early-stage triple-negative breast cancer. J Pers Med. 13(526)2023.PubMed/NCBI View Article : Google Scholar | |
|
Denkert C, von Minckwitz G, Darb-Esfahani S, Lederer B, Heppner BI, Weber KE, Budczies J, Huober J, Klauschen F, Furlanetto J, et al: Tumor-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: A pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 19:40–50. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Han Y, Liu D and Li L: PD-1/PD-L1 pathway: Current research in cancer. Am J Cancer Res. 10:727–742. 2020.PubMed/NCBI | |
|
Yarchoan M, Johnson BR III, Lutz ER, Laheru DA and Jaffee EM: Targeting neoantigens to augment antitumor immunity. Nat Rev Cancer. 17:209–222. 2017. | |
|
Schmid P, Rugo HS, Adams S, Schneeweiss A, Barrios CH, Iwata H, Dieras V, Henschel V, Molinero L, Chui SY, et al: Atezolizumab plus nab-paclitaxel as first-line treatment for unresectable, locally advanced, or metastatic triple-negative breast cancer (IMpassion130): Updated efficacy results from a randomized, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 21:44–59. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Loibl S, Untch M, Burchardi N, Huober J, Sinn BV, Blohmer JU, Grischke EM, Furlanetto J, Tesch H, Hanusch C, et al: A randomised phase II study investigating durvalumab in addition to an anthracycline taxane-based neoadjuvant therapy in early triple-negative breast cancer: Clinical results and biomarker analysis of GeparNuevo study. Ann Oncol. 30:1279–1288. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Loibl S, Schneeweiss A, Huober J, Braun M, Rey J, Blohmer JU, Furlanetto J, Zahm DM, Hanusch C, Thomalla J, et al: Neoadjuvant durvalumab improves survival in early triple-negative breast cancer independent of pathological complete response. Ann. Oncol. 33:1149–1158. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Rizzo A, Cusmai A, Acquafredda S, Giovannelli F, Rinaldi L, Misino A and Palmiotti G: KEYNOTE-522, IMpassion031 and GeparNUEVO: Changing the paradigm of neoadjuvant immune checkpoint inhibitors in early triple-negative breast cancer. Future Oncol. 18:2301–2309. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Sharpe AH and Pauken KE: The diverse functions of the PD1 inhibitory pathway. Nat Rev Immunol. 18:153–167. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Ai L, Xu A and Xu J: Roles of the PD-1/PD-L1 Pathway: Signaling, cancer, and beyond. Adv Exp Med Biol. 1248:33–59. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Jiang X, Wang J, Deng X, Xiong F, Ge J, Xiang B, Wu X, Ma J, Zhou M, Li X, et al: Role of the tumor microenvironment in PD-L1/PD-1-mediated tumor immune escape. Mol Cancer. 18(10)2019.PubMed/NCBI View Article : Google Scholar | |
|
Badve SS, Penault-Llorca F, Reis-Filho JS, Deurloo R, Siziopikou KP, D'Arrigo C and Viale G: Determining PD-L1 Status in Patients With Triple-Negative Breast Cancer: Lessons Learned From IMpassion 130. J Natl Cancer Inst. 114:664–675. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Schmid P, Cortes J, Pusztai L, McArthur H, Kümmel S, Bergh J, Denkert C, Park YH, Hui R, Harbeck N, et al: Pembrolizumab for early triple-negative breast cancer. N Engl J Med. 382:810–821. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Mittendorf EA, Zhang H, Barrios CH, Saji S, Jung KH, Hegg R, Koehler A, Sohn J, Iwata H, Telli ML, et al: Neoadjuvant atezolizumab in combination with sequential nab-paclitaxel and anthracycline-based chemotherapy versus placebo and chemotherapy in patients with early stage triple-negative breast cancer (IMpassion031): A randomised, double-blind, phase 3 trial. Lancet. 396:1090–1100. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Schmid P, Adams S, Rugo HS, Schneeweiss A, Barrios CH, Iwata H, Diéras V, Hegg R, Im SA, Shaw Wright G, et al: Atezolizumab and Nab-Paclitaxel in Advanced Triple-negative breast cancer. N Engl J Med. 379:2108–2121. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Keorges GJ: PD-L1 expression in Triple Negative Breast Cancer: A study of an Iraqi population. J Med Sci. 92(e806)2023. | |
|
Erber R and Hartmann A: Understanding PD-L1 testing in breast cancer: A practical approach. Breast Care (Basel). 15:481–490. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Marletta S, Fusco N, Munari E, Luchini C, Cimadamore A, Brunelli M, Querzoli G, Martini M, Vigliar E, Colombari R, et al: Atlas of PD-L1 for Pathologists: Indications, scores, diagnostic platforms, and reporting systems. J Pers Med. 12(1073)2022.PubMed/NCBI View Article : Google Scholar | |
|
Mittendorf EA, Philips AV, Meric-Bernstam F, Qiao N, Wu Y, Harrington S, Su X, Wang Y, Gonzalez-Angulo AM, Akcakanat A, et al: PD-L1 expression in triple-negative breast cancer. Cancer Immunol Res. 2:361–370. 2014.PubMed/NCBI View Article : Google Scholar | |
|
Beckers RK, Selinger CI, Vilain R, Madore J, Wilmott JS, Harvey K, Holliday A, Cooper CL, Robbins E, Gillett D, et al: Programmed death ligand 1 expression in triple-negative breast cancer is associated with tumor-infiltrating lymphocytes and improved outcome. Histopathology. 69:25–34. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Oner G, Önder S, Karatay H, Ak N, Tükenmez M, Müslümanoğlu M, İğci A, Dincçağ A, Özmen V, Aydiner A, et al: Clinical impact of PD-L1 expression in triple-negative breast cancer patients with residual tumor burden after neoadjuvant chemotherapy. World J Surg Oncol. 19(264)2021.PubMed/NCBI View Article : Google Scholar | |
|
Doğukan R, Uçak R, Doğukan FM, Tanık C, Çitgez B and Kabukcuoğlu F: Correlation between the expression of PD-L1 and clinicopathological parameters in triple negative breast cancer patients. Eur J Breast Health. 15:235–241. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Gonzalez-Ericsson PI, Stovgaard ES, Sua LF, Reisenbichler E, Kos Z, Carter JM, Michiels S, Le Quesne J, Nielsen TO, Laenkholm AV, et al: The path to a better biomarker: Application of a risk management framework for the implementation of PD-L1 and TILs as immuno-oncology biomarkers in breast cancer clinical trials and daily practice. J Pathol. 250:667–684. 2020.PubMed/NCBI View Article : Google Scholar |