Towards effective COVID‑19 vaccines: Updates, perspectives and challenges (Review)
- Authors:
- Published online on: May 6, 2020 https://doi.org/10.3892/ijmm.2020.4596
- Pages: 3-16
-
Copyright: © Calina et al. This is an open access article distributed under the terms of Creative Commons Attribution License.
Abstract
1. Introduction
In December 2019, the first patient with an atypical form of pneumonia was diagnosed in China, a disease that would later be referred to as COVID-19 by the World Health Organization (WHO). One month later, in January 2020, the causative agent of the COVID-19 disease, the SARS-COV-2 virus, was deciphered and identified and its genome was published rapidly (1).
By mid-April, 2020, the extent of impact of COVID-19 on the global population was becoming evident. The most adversely affected region per capita was Western Europe, the most seriously affected population being the elderly, especially those with extensive co-morbidities and weakened immune systems. The causes for regional differences in COVID-19 will require months of analysis, if not years, to ascertain. More focused approaches to reduce the impacts of COVID-19 in the near-term, especially on the most vulnerable populations, need to be pursued, in parallel with longer-term approaches to lessen the impact of COVID-19 (or other coronavirus-driven diseases) across all demographics.
As of mid-April, the very short-term measures that have been implemented to reduce the transmission of SARS-CoV-2 are the same as those that were taken to reduce the transmission of SARS-CoV during the 2002-2003 SARS pandemic: good hygiene and quarantine, with the latter being far more severe and extensive than the quarantine implemented in 2002-2003. Other short-term measures that have been implemented on a very sporadic basis are what can be termed 'tactical treatments'. These tactical treatments do not strengthen the immune system, but rather have the goal of containing the adverse impacts of the viral attack. Some examples of tactical treatments that have been tested are EIDD-2801, remdesivir, favipiravir, chloroquine, hydroxychloroquine, combination of lopinavir and ritonavir, tocilizumab, losartan, to name a few. Tests so far have yielded very mixed results.
A second avenue being pursued to ameliorate/reduce the effects of COVID-19 is development of vaccines to induce viral immunity. The bulk of the present review addresses the status and prospects of this vaccine approach.
The third leg of this triad of approaches to ameliorate the ravaging effects (especially for the most vulnerable) of COVID-19 is what can be called the 'strategic treatment' approach (2). This approach has the goal of strengthening the immune system to allow its adaptive component to neutralize the incoming coronavirus without the need for external support. Strategic treatments eliminate tangible factors that contribute to weaken the immune system. Some examples of such factors, based on existing studies, include titanium dioxide, air pollution, chlorpyrifos, aluminum sulfate, prenatal alcohol exposure, ZnO, oil fly ash, and many others (3-9). Also the real life exposure scenario in which we are exposed continuously to combination of stressors influences in the long term the immune system and the response of the organism to the viral stressors (10-14).
Tsatsakis et al (15) have shown how pollutants can influence the immune system particularly by modulating AhR pathway and how these effects can be prevented by more strict regulations. While some positive impact may result in the short-term from strategic treatments, their main impact will probably be for the long-term, except for those whose immune systems have suffered irreversible damage or those who have an overwhelming genetic predisposition to immune dysfunction. Because strategic treatments appropriate to any specific individual are difficult to identify, and difficult to eliminate because of ingrained habits, some emphasis needs to be placed on those types of treatments that do not require severe lifestyle alterations.
This work aims to analyze the strategies and challenges regarding the development of effective vaccines against SARS-COV-2. The discovery of a vaccine against the novel coronavirus is an important component of the three-pronged approach described initially, given that the pandemic cannot seem to be entirely stopped by social distancing and good hygiene practices. The tactical therapies identified so far have not been entirely effective, especially for the most vulnerable individuals, being unable to prevent severe disability and ultimately death. While healthcare systems are still struggling not to crumble under pressure from coronavirus patients, research laboratories around the world are competing to produce an effective vaccine against SARS-CoV-2 as soon as possible, in order to be able to stop the spread of the new coronavirus.
2. Vaccines: an overview
The development of a vaccine is a complex and time-consuming process, which differs from the development of conventional medicines. Normally, the period of development of a vaccine is 12-15 years (16). While the conventional medicines are oriented towards the treatment of a disease whose symptoms have emerged, vaccines are intended for use in persons not yet exhibiting disease symptoms, in order to prevent the occurrence of diseases (17). Clinical trials to demonstrate the effectiveness of a vaccine focus on demonstrating its ability to prevent the disease, with minimal adverse reactions in the short-term since truly long-term studies in humans are rarely, if ever, conducted (especially on the order of decades), which implies the need to enroll more people than in traditional drug studies (18).
Traditional vaccine development methods, although extremely effective in combating highly contagious diseases such as measles, require large amounts of viruses or bacteria, which can last for months. Those microorganisms then become the key element in a vaccine, the so-called antigen, that warns the human immune system that some foreign organisms have invaded the body and must be eliminated.
Vaccines provide the immune system with the necessary instructions for recognizing and mobilizing lines of defense against disease-causing microorganisms, such as bacteria or viruses. In classical vaccines, antigens (distinctive molecular markers) are introduced into the body, originating from inactivated or half-active bacteria or attenuated viruses. These antigens are capable of causing the disease, but are still capable of activating the immune system, and its cells develop antibodies. If the person comes in contact with the native pathogen, the immune system will already have the necessary antibodies ready and will multiply them much faster because it has already been sensitized by vaccination.
Risk factors for anti-SARS-COV-2 vaccine efficacy
Global immune deficiency is a risk factor for anti-COVID-19 vaccine efficacy, particularly in elderly who have been exposed to a myriad of factors that contribute to weakening of the immune system, as described previously. These factors also result in diseases such as obesity/obesity-related: e.g., type II diabetes, metabolic syndrome and immune-mediated cancers. Mechanistic reasons for these diseases include weakness of antigen recognition, decreased immune cell quantity and functionality, increased level/length and timing of humoral immune alterations of components, reduced initiation of cellular responses, and memory cell disorders. Other associations with immunodeficiency include age-dependent humoral and immune cell alterations; immunosenescence; malnutrition (19); protein-energy-micronutrient deficit and telomere shortening (20). In addition, past or current treatments affect the scalable ineffectiveness of vaccines in both older adults (21) and children (22), especially in immunocompromised (23).
Exposure to immunosuppressive drugs (24) or residence in developing countries (25) with a low socioeconomic status is associated with a higher viral mortality compared to residence in developed countries (26). Current global obesity prevalence in adult and children is also a risk factor for anti-SARS-CoV-2 vaccine inefficacy due to higher levels of IL-6 (27) and decreased IgG concentrations. Parasitic infections, respiratory tract infections such as complicated pneumonia (28), can also affect subsequent immune response to anti-SARS-CoV-2 vaccination (29).
Adjuvant purity and safety, knowledge gaps of the relative contribution of the innate and adaptive responses to protection against individual pathogens, and the precise mode of action of individual adjuvants (30) are existing negative factors in vaccine efficacy. Anti-SARS-CoV-2 vaccines will be available by vaccine market players according to current orphan drug (31) and vaccine legislation (32,33) due to the fight against SARS-CoV-2 pandemic. This means that design defect, failure to warn, and negligence in testing may also affect vaccine efficacy. Under those conditions, long-term safety testing of vaccines in humans will be non-existent. There is no data on whether anti-SARS-CoV-2 vaccines will be first licensed in developed countries (34) or if all vaccine production facilities will be adequate to assure a reliable supply of new anti-SARS-CoV-2 vaccines (35) in a timely manner, and are compatible with specifications and improved adult vaccine design strategy by WHO or immunobiography (36) and heterogeneity of immune responses in the elderly subpopulations (36).
Vaccine safety
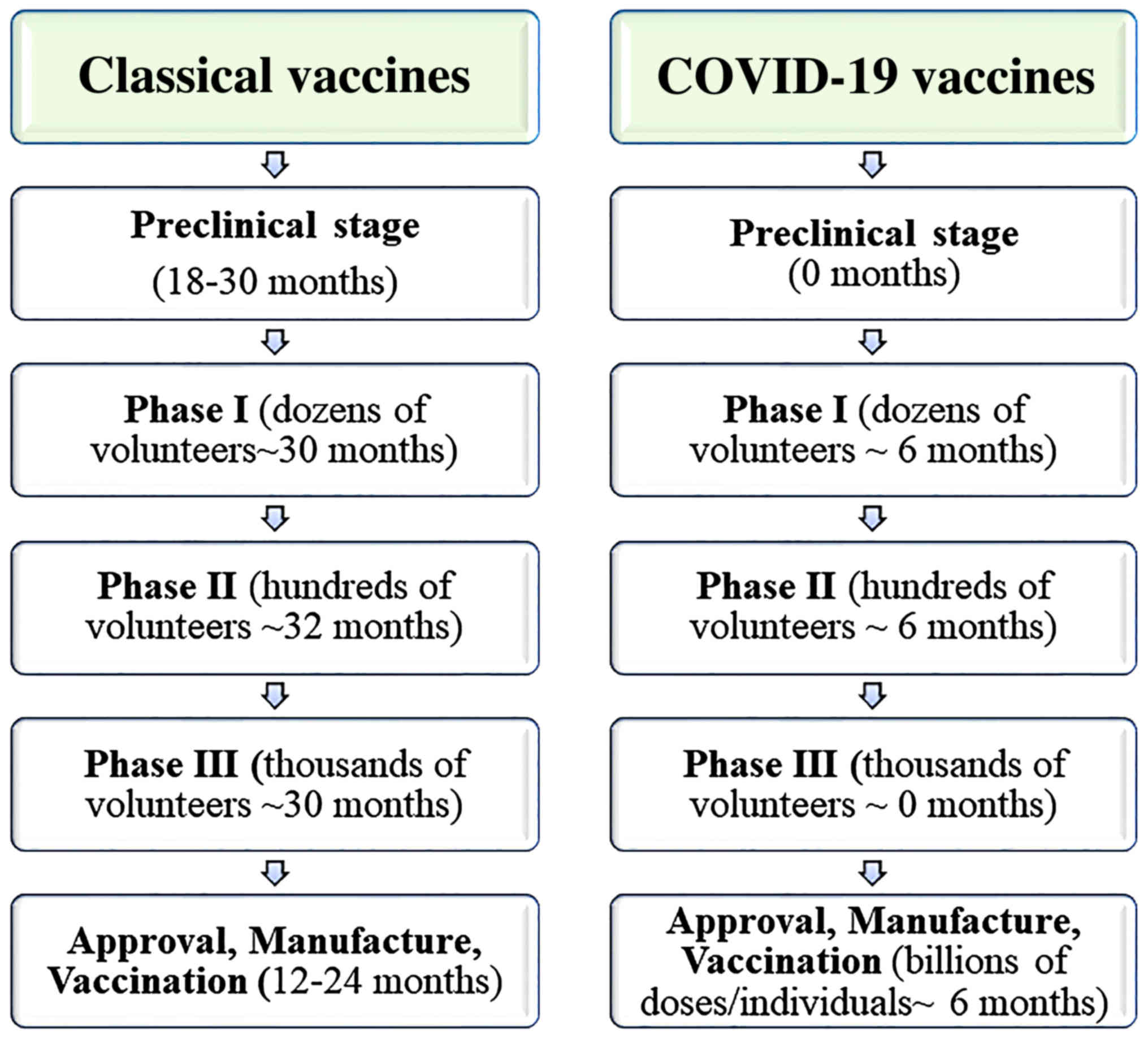
The safety of the vaccine is initially assessed in laboratory studies with mice or rabbits. If the animals do not show signs of disease after receiving the vaccine, then the tests begin in humans, and the number of subjects gradually increases (37). Duration of the clinical trial, on average, for a classical vaccine (after preclinical stage - in vitro and in vivo tests) is as follows (38,39):
In phase I, also called the first human test, the vaccine is given to a small group of healthy volunteers (10 to 100). The purpose is not to test whether the vaccine protects against the disease, but whether it is safe or whether it causes severe side effects.
In phase II, the candidate vaccine is administered to a larger group of subjects (100-1,000), and in phase III, to an even larger group (1,000-100,000). Separate studies may be required in adults, children and the elderly. It sometimes happens that vaccines that seem safe when given to a small number of people, show side effects when given to a larger number of people. This is explained by the fact that any rare complication is less likely to occur when the group of subjects is small. Continuous monitoring is important in case of complications that occur with delayed effect (40). During a pandemic, these sequential studies may be shortened and partially overlapped, but it is important that thousands of vaccinated people are followed for several months before the general purpose vaccine is approved.
If there are more severe signs of inflammation or if the vaccine causes the immune system to malfunction in other ways, the candidate vaccine may not be suitable for widespread use. When such adverse effects are identified, delays in the production process inevitably occur (41). At present, only two potential vaccines against the SARS-CoV-2 virus are in the first phase and this by a derogation from the rule - skipped animal studies (Fig. 1).
The first vaccine that does not follow all research steps is called mRNA-1273 and will be tested in the first phase in Seattle. There is an explanation for the speed of approval, which is related to the fact that the coronavirus is not used in the vaccine development. It is an experimental vaccine, made by a new method, based on RNA. Basically, the RNA molecule in the vaccine teaches the cells to produce the disease-specific antigen and trains the body for the real enemy. But there is also a small problem: to date, no vaccine based mRNA technology has been approved for any disease, although a few have reached the second phase of testing (42).
The second vaccine is Ad5-nCoV. The vaccine is created by genetic engineering and tries to teach the body to recognize the coronavirus protein S, which is delivered via a type-5 adenovirus. Adenoviruses are a family of about one hundred double-stranded DNA viruses that cause various diseases in humans and animals, and type-5 is often used for genetic recombination.
Although clinical trials have begun for these two candidates and are likely to begin soon for other potential vaccines, it is unlikely to move to phase II earlier than a few months.
Vaccine efficacy
Vaccines stimulate immunity to the virus, but can also stimulate inflammation in the body. This can manifest itself either as pain or inflammation at the site where the subject was injected, or as general symptoms such as fever or fatigue (symptoms similar to COVID-19 disease). For most vaccines, these reactions are mild and affect only a small proportion of subjects.
When a vaccine causes the production of antibodies, in mice or in humans, this does not necessarily mean that the vaccine will protect against the disease. Ideally, before moving on to human studies, researchers should be able to demonstrate that the vaccine will protect laboratory animals from the disease when they are experimentally infected with the virus. In the case of diseases caused by previous coronaviruses (SARS and MERS), it was difficult to find an animal species that would be affected by the disease in the same way as humans are affected. However, previous research may help scientists speed up the animal testing process for COVID-19. The protective effect of a human vaccine is assessed using a series of studies similar to the series of safety studies. If the vaccine elicits an immune system response, for example if antibodies can be detected in the phase I study, then larger phase II and phase III studies can be performed to see if the vaccine protects against infection or disease.
Although COVID-19 is a new disease, research on SARS and MERS has helped us understand how the human body responds to coronaviruses and how the response of the immune system generates protection against disease (43). Restricted human studies can also be used to calculate the correct dose and schedule for the vaccine. Some vaccines generate a strong immune response after a single dose, but others require a booster dose after a month or longer. This strategy also increases the duration of studies.
To assess whether a vaccine prevents COVID-19 among those exposed to the infection, it should be tested in phase III studies, in a setting where the infection is actively occurring. In response to the West African Ebola outbreak in 2014/15, the rVSV Ebola vaccine went through all three phases of clinical development in just 12 months, through the centralized coordination of WHO, Médecins Sans Frontières. and manufacturer. During this period, there were still cases of Ebola in Guinea, and the protection of the vaccine was demonstrated by vaccinating the contacts of the residual cases, as they appeared in the community (44).
Vaccine manufacturing
In the case of pandemic vaccines, tens or hundreds of millions of doses are needed. This production process takes at least six months, if the production lines already exist. Any new vaccine involves a new production process, which involves several quality control steps.
The manufacturer must ensure that each vaccine produced is of consistent quality and requires repeated testing. Moreover, because vaccine manufacturing is a biological process, inevitably, some batches of vaccines will fail for reasons that are not always clear, which can further delay production. There are quite a few manufacturers in the world that can produce vaccines on a large enough scale to meet the needs of a pandemic.
Vaccine regulation
Before initiating each stage of the human testing process, the developer must provide evidence that the vaccine has early indications of protection and is safe among those who have been tested. Research ethics committees review clinical trial plans, and authorities such as the European Medicines Agency (EMA) and Food and Drug Administration (FDA) oversee the entire vaccine development process before approving it for general use. These assessments usually take several weeks or months (45). Although such approvals could be shortened in the event of a pandemic, many potential COVID-19 vaccines use new technologies, so regulators will not be able to rely on the experience of similar vaccines to speed up the process. Developers of the COVID-19 vaccine were given a target to produce a vaccine in 12-18 months, while historically, vaccines took 15-20 years to develop. There are diseases against which vaccines do not yet exist, despite decades of work. For example, more than 100,000 children die each year from respiratory diseases caused by another RNA virus, RSV (respiratory syncytial virus), which causes pneumonia. Despite 50 years of research and 18 products developed, there is currently no RSV vaccine available (46).
Numerous scientific research groups are working on the development of a COVID-19 vaccine, using a number of different approaches. Having many groups in the race is important, as most vaccines entering clinical trials will fail for safety or efficacy reasons.
3. The development of a COVID-19 vaccine: current trends and prospects
SARS-COV-2: a brief summary
SARS-COV-2 is part of the coronavirus family, as is SARS-CoV-1 (which generated the 2003 SARS epidemic) and MERS-CoV (which generated the MERS epidemic in 2013) (47).
The new SARS-COV-2 coronavirus (severe acute respiratory syndrome coronavirus 2) causes a respiratory infection called COVID-19 (Coronavirus infectious disease - 2019), with an average incubation period of 5 days (between 2 and 14 days) (48). The disease is characterized by predominant respiratory symptoms (cough, difficulty breathing, fever) of moderate intensity in about 80% of cases, but may have severe manifestations (bilateral interstitial pneumonia), with progression to respiratory failure, acute respiratory distress (ARDS), the main cause of mortality. There are also cases with gastrointestinal manifestations (especially diarrhea), and in some patients (especially in the young ones) hypo/anosmia (loss of sense of smell) and hypo/dysgeusia (alteration of the sense of taste) have been reported as early symptoms (49).
Shortly after the publication of the genetic structure of SARS-COV-2, the first two vaccines were developed. SARS-COV-2 virus structure is composed of an RNA molecule, surrounded by a series of structural and functional proteins (50). Known structural proteins are protein S (or spike - which leads to the characteristic appearance), protein M (membrane), protein E (envelopes), protein N (nucleocapsid). Of these, protein S has the role of attaching to receptors in human cells and facilitating the fusion of viral content with the cell. In the case of SARS-COV-2, the receptor is the angiotensin converting enzyme 2 (ACE2), which is found in large quantities in the respiratory tract and lung parenchyma (51-54). The initial infection of SARS-COV-2 occurs in the ciliary epithelial cells of the bronchi (55,56).
The binding of protein S to ACE2 is greatly favored by the existence of the polybase cleavage site - a protein fragment cleaved by the furin enzyme (commonly found in the human body), allowing protein S fragments (S1, S2 and S3) to perform their function. In addition to fusing the viral envelope with the cell membrane, the virus also infects the human cell through endocytosis (the cell membrane around the portion that binds to the virus forms a vesicle inside the cell, detaches from the membrane and introduces the virus into the cell, via that vesicle). Through the process of entering the cell, the virus loses its envelope (which fuses with the cell membrane) and the viral RNA is free in the cytoplasm, carrying out two processes: replication and transcription. First, the cellular components responsible for RNA transcription produce viral proteins, and the RNA is copied. Subsequently, these proteins and copies of the initial RNA are 'packed' into new virions, released from the cell to spread the infection (57).
Humoral immunity consists of the production of specific antibodies against these antigens. These are: i) antibodies that appear rapidly during infection and disappear rapidly (IgM); and ii) antibodies that appear slower and persist in the body for a long time, even after the infection is cured (IgG) (58).
Cellular immunity requires training certain immune cells to recognize and destroy the virus. It has been observed in SARS-COV-2 infection that the number of CD4+ and CD8+ T lymphocytes is low in the peripheral blood (because they are destroyed in the process of elimination of the virus), but has high concentrations of activation markers (59). Regarding the SARS-CoV virus, memory cells, capable of recognizing it, have been identified in the blood of healed patients, several years after the infection. The persistence of memory cells is an important element to consider in the development of the anti-SARS-CoV-2 vaccine (60). Cases have been described where the SARS-CoV-2 infection recurs after being considered cured (61).
On the other hand, there is evidence that coronaviruses are equipped with mechanisms by which they can sometimes evade immune attack. First, after infection of the cell, the vesicles in which the virus is located are lacking in the receptors that could recognize the virus as an 'invader' of the body. Second, interferon synthesis (with antiviral function) is inhibited by coronaviruses, and the presentation of viral antigens by PCA is low in infected patients (62).
Strategies for COVID-19 vaccine development
Current pandemic of COVID-19, caused by SARS-CoV-2, is a global epidemiological problem, the solution of which will require establishment of large-scale production of the vaccine. Given the experience of previous coronavirus outbreaks, showing a high variability of the virus, it is required to develop a vaccine production platform, providing the scalability, technological flexibility, and versatility. These vaccines must provide high efficacy, safety, and tolerability.
This is due to the time required to prove that the proposed vaccine is safe and effective as well as the time required to produce millions of doses. Many 'candidate' vaccines, which initially look promising, are likely to fail during the testing process. The process of developing a new vaccine begins with a so-called 'candidate' vaccine, which a team of scientists believes to have potential. This is the fastest part of the process and takes up to a few weeks. Thus, some candidate vaccines are being developed in Russia against COVID-19. The Shemyakin and Ovchinnikov Institute of Bioorganic Chemistry is developing Liposome-encapsulated DNA-protein vaccine based on the COVID-19 Spike antigens and its DNA coding sequence and VLP vaccine based on HSB antigen fused with COVID-19 Spike antigens. The vaccine candidates against COVID-19 based on live attenuated recombinant influenza vector platform are developed by FSBSI 'Chumakov Federal Scientific Center for Research and Development of Immune- and Biological Products of Russian Academy of Sciences' and Smorodintsev Research Institute of Influenza (WHO National Influenza Centre). The FSBSI 'Chumakov Federal Scientific Center for Research and Development of Immune- and Biological Products of Russian Academy of Sciences' is developing two vaccines based on an attenuated and an inactivated strain of the COVID-19 virus isolated in Centre Chumakov (personal communication of Professor Egorov).
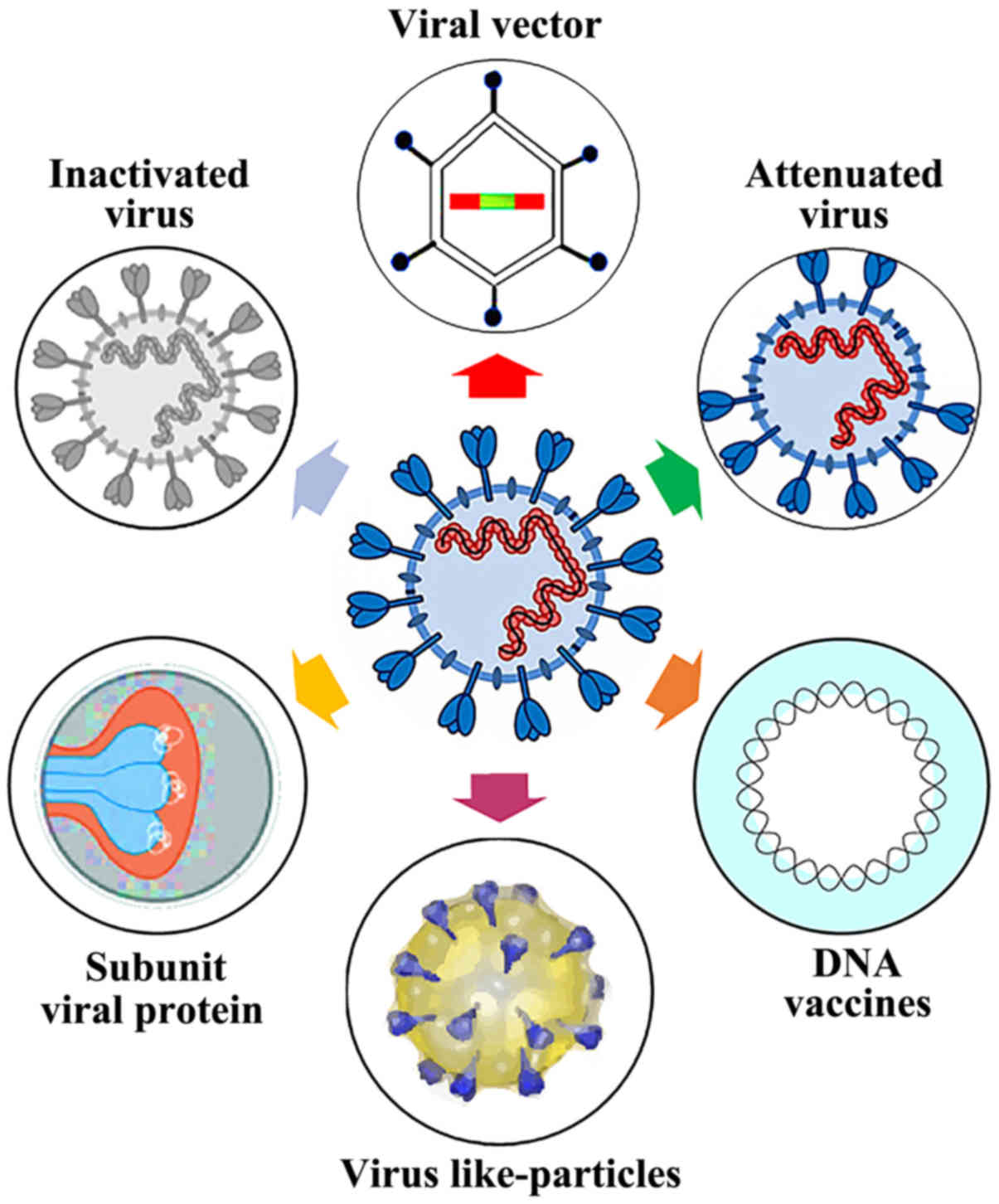
For efficient application of SARS-CoV-2 vaccines, not only the production procedure needs to be developed, but also requires a large-scale production followed by vaccination program targeting muti-million population of different regions. Only such a complex approach will allow combatting of the coronavirus disease pandemic. New technologies do not require the work with live virus, making their production much easier, but still needing further scientific and technological evidence (Fig. 2).
Type of vaccines against SARS-COV-2 RNA vaccines
The mRNA (encoding RiboNucleic Acid) vaccine encodes a stable prefused form (the form before being fused to the cell membrane of the host cell) of Spike protein (S) (63). Protein complex S is required for membrane fusion and host cell infection and has been the target of vaccines against MERS and SARS.
Membrane fusion (viral and cellular) is an essential step when encapsulated viruses enter cells. Fusion of the double lipid layer requires catalysis to overcome a high kinetic barrier, and viral fusion proteins are agents that perform this catalytic function (64). Although coronavirus uses many different proteins to replicate and invade cells, protein S is the main surface protein that it uses to bind to a receptor - this becomes a bridge to the human cell. After protein S binds to the human cell receptor, the viral membrane fuses with the human cell membrane, allowing the viral genome to enter the human cells and initiate infection (49).
The mRNA vaccine against SARS-COV-2 is based on a relatively new genetic method that does not require growing the virus in the laboratory. The technique transforms the human body into a 'living laboratory', because the whole process is no longer carried out in the laboratory, but directly in the body that received the vaccine (65).
The technique is actually based on messenger ribonucleic acid (mRNA) fragments, the genetic material that is copied from DNA and encodes proteins. Moderna company loads its vaccine with viral mRNA, which encodes the proteins of the new coronavirus, and then injects it into the body. Immune cells from the lymph nodes process the mRNA and synthesize specific viral protein antigens so that other immune cells recognize them (66). mRNA is like a software molecule in the body, which then produces viral proteins that can generate an immune response (67). How the body processes the viral protein is often very different from the way it processes the same protein of the vaccine. Thus, one of the theoretical benefits of introducing mRNA into a vaccine is that the body causes the viral protein to behave in exactly the same way that the virus would have directed the host to do (63) (Table I).
DNA vaccines
DNA vaccines represent the latest direction of development in the manufacture of vaccines. Vaccines obtained by recombinant DNA technology are produced by genetic modification.
The DNA encoding the target molecule is introduced via a plasmid or viral vector in a suitable microorganism or cell line, in which DNA is expressed and translated into protein. The product is subsequently recovered by extraction and purification. The injected DNA is a plasmid plus a promoter that provides immunogenic protein synthesis (69).
An advantage of this type of vaccine is that it stimulates both humoral and cellular immunity. Also, this type of vaccine is stable and does not require maintenance under controlled conditions (refrigeration), as is the case for conventional vaccines. In contrast to live attenuated vaccines, the risks arising from a potential inadequate attenuation of vaccine strains are not present in DNA vaccines (70). Other advantages of this new technology are the fact that the plasmids used are easy to manufacture in large quantities, and the immunity conferred is long-term. The disadvantages identified so far with regard to DNA vaccines are due to the fact that this type of vaccine is limited to protein immunogens (71).
A clinical trial for a new DNA vaccine against Coronavirus has begun. This is called ChAdOx1 nCoV-19 and it was initially developed to prevent MERS (72). This vaccine is based on an adenovirus vaccine vector and on SARS-COV-2 spike protein (73). It has been modified so that it cannot be reproduced in the human body and the genetic code that transmits instructions for the production of Coronavirus Spike protein has been added, allowing the adenovirus to produce this protein after vaccination. The result is the formation of antibodies against the Spike protein, known to be on the surface of SARS-COV-2 (74).
The INO-4800 vaccine is another new DNA vaccine to prevent SARS-COV-2 infection. It is entering human phase I testing (75). The Phase I study will enroll up to 40 healthy adult volunteers. Each participant will receive two doses of INO-4800 every four weeks, and initial immune responses and safety data from the study are expected by the end of the summer. Preclinical data have shown promising results in immune response in several animal models. Also, the preclinical results for the INOVIO SARS-COV-2 vaccine were consistent with the results of the Phase I study for the Middle East Respiratory Syndrome (MERS) vaccine, caused by another type of coronavirus. Here, the INOVIO DNA vaccine was well tolerated and induced high levels of antibody response in 95% of subjects, generating T cell-mediated responses in nearly 90% of study participants. Long-term antibody response was maintained for up to 60 weeks in the case of the anti-MERS vaccine (75) (Table II).
Protein subunit
Subunit vaccines contain only certain antigenic determinants of pathogenic microorganisms, and are obtained either starting from conventional cultivation processes, or by recombinant DNA technology (76).
Antigen determinants included in the vaccine increase the efficiency of the immune response, and the presence of a small number of pathogens reduces the risk of side effects. Subunit vaccines mainly contain surface fragments of pathogens. Because these types of structures are weak immunogens, to obtain vaccines with suitable efficacy, the antigens are conjugated with protein molecules (77).
Antigen purifiers sometimes lead to loss of immunogenicity, requiring coupling with a protein carrier or with an aluminum salt. However, adjuvants are associated with the onset of local reactions to the vaccination site. Also, the duration the immunity conferred by vaccination is lower, except for live vaccines (78) (Table III).
Viral vectors
Along with traditional virus vaccines, viral vectors are widely used, in which genome of one virus is used to deliver the antigen of another virus, thus allowing development of a platform technology of virus production. These technologies are available for large-scale production of vaccines. Drawbacks of such vaccines include a large variation of purification methods, need for a reliable confirmation of purity and activity of the virus (79) (Tables IV and V).
VLPs (virus-like particles)
Vaccine development based on the recombinant proteins and virus-like particles (VLPs) is a more innovative approach. Antiviral vaccines are usually developed on the basis of surface proteins that form VLPs. Production of VLPs in the cells with further reconstruction into the stable and immunogenic forms is a multi-stage process. Substantial issues appear for the VLP production for non-enveloped viruses. Nucleic acid based vaccines are very interesting from the platform technology viewpoint, allowing the same process to be used for the production of different antigens. They elicit both humoral and cell immune responses (80).
Production of these vaccines may be based on E. coli cell fermentation and corresponding technologies of extraction and purification of plasmids ensuring their structural integrity (81) (Table VI).
Inactivated virus
Another category of vaccines is vaccines containing whole microorganisms, but inactivated by chemical or physical methods. This type of vaccine has the advantage of higher stability; however, effectiveness is lower and requires reminders of immune system. Vaccines with inactivated live virus require stabilization of the structure in the dry form, separate supply of the solvent, and cold-chain transportation. These factors complicate the production process and lead to increase of their cost (82) (Table VII).
Live attenuated virus
Live attenuated vaccines were the first vaccines utilized. These types of vaccines are obtained through cultivation of microorganisms under suboptimal conditions or through successive passage in cultures, techniques that determine attenuation of virulence while maintaining the capacity to induce the immune response (83).
Although characterized as very effective, live attenuated vaccines have the disadvantages of risks related to the possible occurrence of mutations, leading to the virulence reversal, as well as contra-indication in the case of immunocompromised persons (Table VIII).
Others
The LV-SMENP-DC Vaccine (Lentiviral Minigene Vaccine, Shenzhen Geno-Immune Medical Institute) entered Phase I clinical trial in March 2020. It is a vaccine based on dendritic cells modified with a lentiviral vector expressing synthetic minigens based on selected viral protein domains, and is administered with antigen-specific cytotoxic T lymphocytes (84).
Pathogen-specific aAPC vaccine (Shenzhen Geno-Immune Medical Institute), Phase 1 clinical trial (85) is based on lentiviral vector modified artificial antigen presenting cells (aAPCs) expressing synthetic minigens based on selected viral protein domains.
4. Discussion
The challenges of COVID-19 vaccines. Where do we stand?
The development and manufacture of a COVID-19 vaccine is an urgent issue, but it is likely to take many months to resolve. Although many companies have announced that the COVID-19 vaccine will be ready soon, this will be quite difficult to do in reality (72).
The main reason is that before being put on the market, the vaccine should be safe, both in the short-term and in the long-term. This is very important because, in the history of vaccine production, there have been situations of contamination with other viruses, fortunately without major consequences (16). For example, one third of the polio vaccines administered in the US between 1955 and 1963 also contained simian virus 40 (SV40) and more recently, rotavirus vaccines have been discovered to also have swine circoviruses (86-88).
In order to avoid such situations, everything to be tested on humans should first be checked for purity, and then sterile production lines provided. This takes time. In rare cases, certain antibodies generated by immunization may promote an aggravated form of the disease (a situation called ADE, antibody dependent enhancement) (89). When these antibodies re-establish contact with the virus, they will actually help it enter the cells and cause infection. ADE has been described in many viral infections (influenza, Dengue, Zika, etc.), but also in coronaviruses. The mechanism of ADE has not been confirmed for coronavirus in humans (90).
Several animal studies have shown that some types of anti-SARS and anti-MERS vaccines, although effective in generating antibodies, can lead to more severe forms of disease when the virus is subsequently inoculated (91).
The second reason is that the vaccine must not only be safe, but also effective. It must be able to determine the synthesis of antibodies of a certain type, at a certain concentration (titer) and to provide protection for a reasonable time.
However, vaccines never generate immunity to all vaccinated people (92). The causes are complex and vary from genetic and immunological factors, to the quality of the vaccines themselves and how they are administered.
Age is an important aspect and some influenza studies have shown that aging of the immune system dramatically decreases the effectiveness of vaccination (93). Therefore, for any future anti-SARS-COV-2 vaccine, all these aspects should be evaluated, and the primary immunization failures minimized by adjusting the doses or number of administrations.
Assuming that the vaccine will generate an effective immune response to a sufficient number of individuals among those vaccinated, the time frame of vaccine protection is questionable (94). For example, after measles vaccination, a small percentage of those who initially respond well, lose their protective antibody status within a few years, a phenomenon called secondary immunization failure (95).
This is why it takes time to check the post-vaccination persistence of anti-COVID antibodies. Last but not least, both safety and efficacy are significantly dependent on the type of vaccine, i.e. the technology or platform used.
Some technologies are very new and therefore require more careful testing. Others are old but need to be adapted for COVID-19. Another aspect is not only the ability of a company to develop the technology, but also its large-scale production capacity so that it is quickly accessible globally. Because there is no commercially available anti-SARS-COV-2 vaccine precedent for the proposed platforms, completely new production lines, capable of generating billions of doses in a few months, must be considered. And this must be done without stopping the production of current vaccines, already included in the official protocols and guidelines. At present, this capacity will be reached with difficulty and will represent an unprecedented effort. DNA and RNA vaccines are based on the principle of insertion of these nucleic acids in some cells of the vaccinated ones, forcing them to make immunogenic viral proteins (96). Although some recent data seem encouraging, these concepts have questionable efficiency in humans. Non-replicative vectors are actually common viruses (e.g., adenovirus) genetically modified to display SARS-CoV proteins on the outer surface (97). But they are so common that many of us have already met with them throughout our lives and as a result, we already have immunity and neutralize them before they do their job.
The attenuated viruses would be variants of SARS-CoV-2 made less or not at all pathogenic by genetic engineering. They are by far the most immunogenic, but there is a risk that they will become pathogenic after mutations (98).
Inactivated viruses, viral fragments, and synthetic peptides are all relatively weakly immunogenic.
The analysis of these variables is normally done over 10 years, in the form of a trial. The stages of a trial are inflexible, standardized, intensely regulated for the purpose of maximum safety and efficacy of the final vaccine.
The first stage is the preclinical research, in which the technology that will be included in the vaccine is selected and then the efficacy and safety profile of human cells (in vitro) and animal models (in vivo) is tested. If the expected anti-infectious effect is seen in vitro, and cells do not die excessively, then in vivo animal studies are conducted. Mice are usually the perfect candidate for in vivo studies, because they are about 85% genetically similar to humans, relatively inexpensive, and do not raise major ethical issues (99). However, one of the notable differences between the human and the mouse is fixed in the case of the ACE2 receptor gene (to which SARS viruses bind during infection). Mice simply do not make the respiratory syndromes, they eliminate the virus relatively quickly from the body. This is why it is necessary for either the genetically modified mouse to have a human ACE2 receptor, or to use ferrets and monkeys, and this makes everything much more expensive and more difficult to access.
The preclinical stage lasts between 1½ and 2½ years and is by far the most selective. It is estimated that less than 20% of the vaccines tested are able to progress to human tests. Some fail because the product does not work, others because they can no longer find financing (1,100).
After obtaining the vaccine, the first people vaccinated will be the highest risk categories. For everyone else, the term is sometime in 2022, possibly long after we have naturally acquired immunity.
There are still many unknowns related to coronavirus immunity and that is why obtaining a vaccine is difficult. Future mutations in SARS-COV-2 could occur at any time, which automatically means a high risk of any vaccine becoming useless. No vaccine has been obtained for any other coronavirus so far, and no one can guarantee its success yet. It is possible that we will have the anti-COVID vaccine in a very short time, without having the benefits from long-term testing results. The vaccine will probably not be available to all of us for 18 months.
5. Conclusion and future perspectives
Scientists began working on coronavirus vaccines during SARS and MERS outbreaks, but their efforts did not materialize because of a myriad of difficulties. Since this extremely severe current coronavirus pandemic, COVID-19, the spread of the outbreak appears much broader than was the case for SARS. There is also the possibility of the disease becoming endemic and seasonal in its appearance, according to some investigators. This explains why many research groups and companies are undertaking efforts to develop an effective vaccine against SARS-CoV-2 all over the world, also speeding up all the usual phases needed to develop and test a vaccine in the human.
An important feature in the landscape of vaccine research and development for SARS-COV-2 is represented by the varied range of evaluated technological platforms, including nucleic acids (DNA and RNA), virus-like particles, peptides, viral vector (replicative and non-replicative), recombinant proteins, live attenuated viruses and inactivated viruses. Many of these platforms are not currently the basis of vaccines already authorized, but experience in areas such as oncology encourages developers to exploit new opportunities for increased development and manufacturing speeds.
There is not an effective therapy for severe COVID-19, and social distancing is extremely 'costly' from a social and economic perspective. Therefore, the development of an effective vaccine, along with efforts to implement immune-enhancing strategic treatments and shorter-term efforts to identify tactical repurposed treatments, should be considered major public health priorities. We hope to get this key tool for disease prevention, and to do this quite soon.
It is unknown whether there ever will be a successful SARS-CoV-2 vaccine, but the efforts of the scientific community in attempting to develop such a vaccine is without precedent. Thus, COVID-19 vaccines are a never ending story.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
Conceptualization: DC, AT, AOD and DAS; validation, research, resources, data reviewing, and writing: DP, AME, AAI, AGG, MIS, RK, FC, MV; review and editing: DC, AOD, AT, DP and RK. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
DAS is the Editor-in-Chief for the journal, but had no personal involvement in the reviewing process, or any influence in terms of adjudicating on the final decision, for this article. The other authors declare that they have no competing interests.
Acknowledgments
Not applicable.
References
|
Yuen KS, Ye ZW, Fung SY, Chan CP and Jin DY: SARS-CoV-2 and COVID-19: The most important research questions. Cell Biosci. 10:402020. View Article : Google Scholar : PubMed/NCBI | |
|
Kostoff RN: Combining Tactical and Strategic Treatments for COVID-19. Georgia Institute of Technology; 2020, http://hdl.handle.net/1853/62523 Accessed March 23 2020. | |
|
Hashem MM, Abo-El-Sooud K, Abd-Elhakim YM, Badr YA, El-Metwally AE and Bahy-El-Dien A: The long-term oral exposure to titanium dioxide impaired immune functions and triggered cytotoxic and genotoxic impacts in rats. J Trace Elem Med Biol. 60:1264732020. View Article : Google Scholar : PubMed/NCBI | |
|
Torres M, Carranza C, Sarkar S, Gonzalez Y, Osornio Vargas A, Black K, Meng Q, Quintana-Belmares R, Hernandez M, Angeles Garcia JJF, et al: Urban airborne particle exposure impairs human lung and blood Mycobacterium tuberculosis immunity. Thorax. 74:675–683. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Goumenou M, Sarigiannis D, Tsatsakis A, Anesti O, Docea AO, Petrakis D, Tsoukalas D, Kostoff R, Rakitskii V, Spandidos DA, et al: COVID-19 in Northern Italy: An integrative overview of factors possibly influencing the sharp increase of the outbreak (Review). Mol Med Rep. 22:20–32. 2020.PubMed/NCBI | |
|
Omran GA: Hematological and immunological impairment following in-utero and postnatal exposure to aluminum sulfate in female offspring of albino rats. Immunopharmacol Immunotoxicol. 41:40–47. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Reid N, Moritz KM and Akison LK: Adverse health outcomes associated with fetal alcohol exposure: A systematic review focused on immune-related outcomes. Pediatr Allergy Immunol. 30:698–707. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Engin AB, Nikitovic D, Neagu M, Henrich-Noack P, Docea AO, Shtilman MI, Golokhvast K and Tsatsakis AM: Mechanistic understanding of nanoparticles' interactions with extracellular matrix: The cell and immune system. Part Fibre Toxicol. 14:222017. View Article : Google Scholar : PubMed/NCBI | |
|
Delfosse VC, Tasat DR and Gioffré AK: In vivo short-term exposure to residual oil fly ash impairs pulmonary innate immune response against environmental mycobacterium infection. Environ Toxicol. 30:589–596. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Tsatsakis A, Docea AO, Constantin C, Calina D, Zlatian O, Nikolouzakis TK, Stivaktakis PD, Kalogeraki A, Liesivuori J, Tzanakakis G, et al: Genotoxic, cytotoxic, and cytopathological effects in rats exposed for 18 months to a mixture of 13 chemicals in doses below NOAEL levels. Toxicol Lett. 316:154–170. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Docea AO, Calina D, Goumenou M, Neagu M, Gofita E and Tsatsakis A: Study design for the determination of toxicity from long-term-low-dose exposure to complex mixtures of pesticides, food additives and lifestyle products. Toxicol Lett. 258:S1792016. View Article : Google Scholar | |
|
Docea AO, Gofita E, Goumenou M, Calina D, Rogoveanu O, Varut M, Olaru C, Kerasioti E, Fountoucidou P, Taitzoglou I, et al: Six months exposure to a real life mixture of 13 chemicals' below individual NOAELs induced non monotonic sex-dependent biochemical and redox status changes in rats. Food Chem Toxicol. 115:470–481. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Docea AO, Goumenou M, Calina D, Arsene AL, Dragoi CM, Gofita E, Pisoschi CG, Zlatian O, Stivaktakis PD, Nikolouzakis TK, et al: Adverse and hormetic effects in rats exposed for 12 months to low dose mixture of 13 chemicals: RLRS part III. Toxicol Lett. 310:70–91. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Fountoucidou P, Veskoukis AS, Kerasioti E, Docea AO, Taitzoglou IA, Liesivuori J, Tsatsakis A and Kouretas D: A mixture of routinely encountered xenobiotics induces both redox adaptations and perturbations in blood and tissues of rats after a long-term low-dose exposure regimen: The time and dose issue. Toxicol Lett. 317:24–44. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Tsatsakis A, Petrakis D, Nikolouzakis TK, Docea AO, Calina D, Vinceti M, Goumenou M, Kostoff RN, Mamoulakis C, Aschner M, et al: COVID-19, an opportunity to reevaluate the correlation between long-term effects of anthropogenic pollutants on viral epidemic/pandemic events and prevalence. Food Chem Toxicol. In Press. | |
|
Han S: Clinical vaccine development. Clin Exp Vaccine Res. 4:46–53. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Kamal AM, Mitrut P, Docea AO, Soşoi S, Kamal KC, Mitrut R, Mărgăritescu D, Călina D, Banciu C, Tica OS, et al: Double therapy with pegylated Interferon and Ribavirin for chronic hepatitis C. A pharmacogenenetic guide for predicting adverse events. Farmacia. 65:877–884. 2017. | |
|
Black S: The costs and effectiveness of large Phase III pre-licensure vaccine clinical trials. Expert Rev Vaccines. 14:1543–1548. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Wouters-Wesseling W, Rozendaal M, Snijder M, Graus Y, Rimmelzwaan G, De Groot L and Bindels J: Effect of a complete nutritional supplement on antibody response to influenza vaccine in elderly people. J Gerontol A Biol Sci Med Sci. 57:M563–M566. 2002. View Article : Google Scholar : PubMed/NCBI | |
|
Tsoukalas D, Fragkiadaki P, Docea AO, Alegakis AK, Sarandi E, Vakonaki E, Salataj E, Kouvidi E, Nikitovic D, Kovatsi L, et al: Association of nutraceutical supplements with longer telomere length. Int J Mol Med. 44:218–226. 2019.PubMed/NCBI | |
|
Ventura MT, Casciaro M, Gangemi S and Buquicchio R: Immunosenescence in aging: Between immune cells depletion and cytokines up-regulation. Clin Mol Allergy. 15:212017. View Article : Google Scholar : PubMed/NCBI | |
|
Savy M, Edmond K, Fine PE, Hall A, Hennig BJ, Moore SE, Mulholland K, Schaible U and Prentice AM: Landscape analysis of interactions between nutrition and vaccine responses in children. J Nutr. 139:2154S–2218S. 2009. View Article : Google Scholar : PubMed/NCBI | |
|
Arvas A: Vaccination in patients with immunosuppression. Turk Pediatri Ars. 49:181–185. 2014. View Article : Google Scholar | |
|
Pickering LK, Baker CJ, Kimberlin DW and Long SS: Red Book: 2012 Report of the Committee on Infectious Diseases. | |
|
Keusch GT: Nutritional effects on response of children in developing countries to respiratory tract pathogens: Implications for vaccine development. Rev Infect Dis. 13(Suppl 6): S486–S491. 1991. View Article : Google Scholar : PubMed/NCBI | |
|
Opal SM, Girard TD and Ely EW: The immunopathogenesis of sepsis in elderly patients. Clin Infect Dis. 41(Suppl 7): S504–S512. 2005. View Article : Google Scholar : PubMed/NCBI | |
|
Eliakim A, Schwindt C, Zaldivar F, Casali P and Cooper DM: Reduced tetanus antibody titers in overweight children. Autoimmunity. 39:137–141. 2006. View Article : Google Scholar : PubMed/NCBI | |
|
Calina D, Roșu L, Roșu AF, Ianoşi G, Ianoşi S, Zlatian O, Mitruț R, Docea AO, Rogoveanu O, Mitruț P, et al: Etiological diagnosis and pharmacotherapeutic management of parap-neumonic pleurisy. Farmacia. 64:946–952. 2016. | |
|
Skalny AV, Rink L, Ajsuvakova OP, Aschner M, Gritsenko VA, Alekseenko SI, Svistunov AA, Petrakis D, Spandidos DA, Aaseth J, et al: Zinc and respiratory tract infections: Perspectives for COVID-19 (Review). Int J Mol Med. 46:17–26. 2020. | |
|
Stanberry LR and Strugnell R: Vaccines of the future. Understanding Modern Vaccines: perspectives in Vaccinology. Garçon N, Stern PL and Cunningham AL: Elsevier; pp. 151–199. 2011 | |
|
Scharf SF: Orphan drugs: The question of products liability. Am J Law Med. 10:491–513. 1985.PubMed/NCBI | |
|
Haffner ME and Kelsey JV: Evaluation of orphan products by the U.S. Food and Drug Administration. Int J Technol Assess Health Care. 8:647–657. 1992. View Article : Google Scholar : PubMed/NCBI | |
|
Olliario P: Will the fight against tropical diseases benefit from orphan drug status? Trop Med Int Health. 2:113–115. 1997. View Article : Google Scholar : PubMed/NCBI | |
|
Mahoney RT and Maynard JE: The introduction of new vaccines into developing countries. Vaccine. 17:646–652. 1999. View Article : Google Scholar : PubMed/NCBI | |
|
Milstien J, Batson A and Meaney W: A systematic method for evaluating the potential viability of local vaccine producers. Vaccine. 15:1358–1363. 1997. View Article : Google Scholar : PubMed/NCBI | |
|
Franceschi C, Salvioli S, Garagnani P, de Eguileor M, Monti D and Capri M: Immunobiography and the heterogeneity of immune responses in the elderly: A focus on inflamation and trained immunity. Front Immunol. 8:9822017. View Article : Google Scholar | |
|
DeStefano F, Bodenstab HM and Offit PA: Principal controversies in vaccine safety in the United States. Clin Infect Dis. 69:726–731. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Pronker ES, Weenen TC, Commandeur H, Claassen EH and Osterhaus AD: Risk in vaccine research and development quantified. PLoS One. 8:e577552013. View Article : Google Scholar : PubMed/NCBI | |
|
Goetz KB, Pfleiderer M and Schneider CK: First-in-human clinical trials with vaccines - what regulators want. Nat Biotechnol. 28:910–916. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
Guerra Mendoza Y, Garric E, Leach A, Lievens M, Ofori-Anyinam O, Pirçon JY, Stegmann JU, Vandoolaeghe P, Otieno L, Otieno W, et al: Safety profile of the RTS, S/AS01 malaria vaccine in infants and children: Additional data from a phase III randomized controlled trial in sub-Saharan Africa. Hum Vaccin Immunother. 15:2386–2398. 2019. View Article : Google Scholar : | |
|
Peeples L: News feature: Avoiding pitfalls in the pursuit of a COVID-19 vaccine. Proc Natl Acad Sci USA. 117:8218–8221. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Schlake T, Thess A, Fotin-Mleczek M and Kallen KJ: Developing mRNA-vaccine technologies. RNA Biol. 9:1319–1330. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Yi Y, Lagniton PNP, Ye S, Li E and Xu RH: COVID-19: What has been learned and to be learned about the novel coronavirus disease. Int J Biol Sci. 16:1753–1766. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Wojda TR, Valenza PL, Cornejo K, McGinley T, Galwankar SC, Kelkar D, Sharpe RP, Papadimos TJ and Stawicki SP: The Ebola Outbreak of 2014-2015: From Coordinated Multilateral Action to Effective Disease Containment, Vaccine Development, and Beyond. J Glob Infect Dis. 7:127–138. 2015. View Article : Google Scholar | |
|
Grenham A and Villafana T: Vaccine development and trials in low and lower-middle income countries: Key issues, advances and future opportunities. Hum Vaccin Immunother. 13:2192–2199. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Mazur NI, Higgins D, Nunes MC, Melero JA, Langedijk AC, Horsley N, Buchholz UJ, Openshaw PJ, McLellan JS, Englund JA, et al: Respiratory Syncytial Virus Network (ReSViNET) Foundation: The respiratory syncytial virus vaccine landscape: Lessons from the graveyard and promising candidates. Lancet Infect Dis. 18:e295–e311. 2018. View Article : Google Scholar | |
|
Docea AO, Tsatsakis A, Albulescu D, Cristea O, Zlatian O, Vinceti M, Moschos SA, Tsoukalas D, Goumenou M, Drakoulis N, et al: A new threat from an old enemy: Re-emergence of coronavirus (Review). Int J Mol Med. 45:1631–1643. 2020.PubMed/NCBI | |
|
Goumenou M, Spandidos DA and Tsatsakis A: [Editorial] Possibility of transmission through dogs being a contributing factor to the extreme Covid-19 outbreak in North Italy. Mol Med Rep. 21:2293–2295. 2020.PubMed/NCBI | |
|
Chen Y, Liu Q and Guo D: Emerging coronaviruses: Genome structure, replication, and pathogenesis. J Med Virol. 92:418–423. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Yang P and Wang X: COVID-19: A new challenge for human beings. Cell Mol Immunol. 17:555–557. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, et al: SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 181:271–280.e8. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Wang Q, Zhang Y, Wu L, Niu S, Song C, Zhang Z, Lu G, Qiao C, Hu Y, Yuen KY, et al: Structural and functional basis of SARS-CoV-2 entry by using human ACE2. Cell. Apr 7–2020.Epub ahead of print. | |
|
Li Y, Zhou W, Yang L and You R: Physiological and pathological regulation of ACE2, the SARS-CoV-2 receptor. Pharmacol Res. 157:1048332020. View Article : Google Scholar : PubMed/NCBI | |
|
Lukassen S, Chua RL, Trefzer T, Kahn NC, Schneider MA, Muley T, Winter H, Meister M, Veith C, Boots AW, et al: SARS-CoV-2 receptor ACE2 and TMPRSS2 are primarily expressed in bronchial transient secretory cells. EMBO J. 4:e1051142020. | |
|
Leung JM, Yang CX, Tam A, Shaipanich T, Hackett TL, Singhera GK, Dorscheid DR and Sin DD: ACE-2 expression in the small airway epithelia of smokers and COPD patients: Implications for COVID-19. Eur Respir J. Apr 8–2020.Epub ahead of print. View Article : Google Scholar | |
|
Mousavizadeh L and Ghasemi S: Genotype and phenotype of COVID-19: Their roles in pathogenesis. J Microbiol Immunol. Mar 31–2020.Epub ahead of print. | |
|
Woo PC, Huang Y, Lau SK and Yuen KY: Coronavirus genomics and bioinformatics analysis. Viruses. 2:1804–1820. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
Liu W, Fontanet A, Zhang PH, Zhan L, Xin ZT, Baril L, Tang F, Lv H and Cao WC: Two-year prospective study of the humoral immune response of patients with severe acute respiratory syndrome. J Infect Dis. 193:792–795. 2006. View Article : Google Scholar : PubMed/NCBI | |
|
Ganji A, Farahani I, Khansarinejad B, Ghazavi A and Mosayebi G: Increased expression of CD8 marker on T-cells in COVID-19 patients. Blood Cells Mol Dis. 83:1024372020. View Article : Google Scholar : PubMed/NCBI | |
|
Farsalinos K, Niaura R, Le Houezec J, Barbouni A, Tsatsakis A, Kouretas D, Vantarakis A and Poulas K: Editorial: Nicotine and SARS-CoV-2: COVID-19 may be a disease of the nicotinic cholinergic system. Toxicol Rep. Apr 30–2020.Epub ahead of print. View Article : Google Scholar : PubMed/NCBI | |
|
Zhou G and Zhao Q: Perspectives on therapeutic neutralizing antibodies against the Novel Coronavirus SARS-CoV-2. Int J Biol Sci. 16:1718–1723. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Kikkert M: Innate immune evasion by human respiratory RNA viruses. J Innate Immun. 12:4–20. 2020. View Article : Google Scholar : | |
|
Jackson NAC, Kester KE, Casimiro D, Gurunathan S and DeRosa F: The promise of mRNA vaccines: A biotech and industrial perspective. NPJ Vaccines. 5:112020. View Article : Google Scholar : PubMed/NCBI | |
|
Zhang C, Maruggi G, Shan H and Li J: Advances in mRNA Vaccines for infectious diseases. Front Immunol. 10:5942019. View Article : Google Scholar : PubMed/NCBI | |
|
Pardi N, Hogan MJ, Porter FW and Weissman D: mRNA vaccines - a new era in vaccinology. Nat Rev Drug Discov. 17:261–279. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Maruggi G, Zhang C, Li J, Ulmer JB and Yu D: mRNA as a transformative technology for vaccine development to control infectious diseases. Mol Ther. 27:757–772. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Kramps T and Probst J: Messenger RNA-based vaccines: Progress challenges, applications. Wiley Interdiscip Rev RNA. 4:737–749. 2013. View Article : Google Scholar : PubMed/NCBI | |
|
World Health Organization (WHO): DRAFT landscape of COVID-19 candidate vaccines. WHO; Geneva: 2020, https://www.who.int/blueprint/priority-diseases/key-action/Novel_Coronavirus_Landscape_nCoV_11April2020.PDF?ua=1. Accessed April 11 2020. | |
|
Li L and Petrovsky N: Molecular mechanisms for enhanced DNA vaccine immunogenicity. Expert Rev Vaccines. 15:313–329. 2016. View Article : Google Scholar : | |
|
Hobernik D and Bros M: DNA Vaccines-How Far From Clinical Use? Int J Mol Sci. 19:E36052018. View Article : Google Scholar : PubMed/NCBI | |
|
Ferraro B, Morrow MP, Hutnick NA, Shin TH, Lucke CE and Weiner DB: Clinical applications of DNA vaccines: Current progress. Clin Infect Dis. 53:296–302. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Thanh Le T, Andreadakis Z, Kumar A, Gómez Román R, Tollefsen S, Saville M and Mayhew S: The COVID-19 vaccine development landscape. Nat Rev Drug Discov. Apr 9–2020.Epub ahead of print. View Article : Google Scholar : PubMed/NCBI | |
|
US National Library of Medicine, ClinicalTrials.gov: A Study of a Candidate COVID-19 Vaccine (COV001). https://clinicaltrials.gov/ct2/show/NCT04324606. Accessed March 27 2020. | |
|
Clinical Trials Arena: University of Oxford starts enrolment for Covid-19 vaccine trial. https://www.clinicaltrialsarena.com/news/oxford-university-covid-19-vaccine-trial/ Accessed March 30, 2020. | |
|
Clinical Trials Arena: Inovio commences Phase I trial of DNA vaccine for Covid-19. https://www.clinicaltrialsarena.com/news/inovio-SARS-COV-2-vaccine-trial/. Accessed April 7, 2020. | |
|
Zhang N, Tang J, Lu L, Jiang S and Du L: Receptor-binding domain-based subunit vaccines against MERS-CoV. Virus Res. 202:151–159. 2015. View Article : Google Scholar : | |
|
Lee NH, Lee JA, Park SY, Song CS, Choi IS and Lee JB: A review of vaccine development and research for industry animals in Korea. Clin Exp Vaccine Res. 1:18–34. 2012. View Article : Google Scholar | |
|
Wang M, Jiang S and Wang Y: Recent advances in the production of recombinant subunit vaccines in Pichia pastoris. Bioengineered. 7:155–165. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Choi Y and Chang J: Viral vectors for vaccine applications. Clin Exp Vaccine Res. 2:97–105. 2013. View Article : Google Scholar : PubMed/NCBI | |
|
Sarkar B, Islam SS, Zohora US and Ullah MA: Virus like particles - A recent advancement in vaccine development. Korean J Microbiol. 55:327–343. 2019. | |
|
Huang X, Wang X, Zhang J, Xia N and Zhao Q: Escherichia coli-derived virus-like particles in vaccine development. NPJ Vaccines. 2:32017. View Article : Google Scholar : | |
|
Sridhar S, Brokstad KA and Cox RJ: Influenza vaccination strategies: Comparing inactivated and live attenuated influenza vaccines. Vaccines (Basel). 3:373–389. 2015. View Article : Google Scholar | |
|
Lauring AS, Jones JO and Andino R: Rationalizing the development of live attenuated virus vaccines. Nat Biotechnol. 28:573–579. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
US National Library of Medicine, ClinicalTrials.gov: Immunity and Safety of Covid-19 Synthetic Minigene Vaccine. https://clinicaltrials.gov/ct2/show/NCT04276896. Accessed February 19, 2020. | |
|
US National Library of Medicine, ClinicalTrials.gov: Safety and Immunity of Covid-19 aAPC Vaccine. https://clinicaltrials.gov/ct2/show/NCT04299724. Accessed March 9, 2020. | |
|
Dang-Tan T, Mahmud SM, Puntoni R and Franco EL: Polio vaccines, Simian Virus 40, and human cancer: The epidemiologic evidence for a causal association. Oncogene. 23:6535–6540. 2004. View Article : Google Scholar : PubMed/NCBI | |
|
Strickler HD, Rosenberg PS, Devesa SS, Hertel J, Fraumeni JF Jr and Goedert JJ: Contamination of poliovirus vaccines with simian virus 40 (1955-1963) and subsequent cancer rates. JAMA. 279:292–295. 1998. View Article : Google Scholar : PubMed/NCBI | |
|
Baylis SA, Finsterbusch T, Bannert N, Blümel J and Mankertz A: Analysis of porcine circovirus type 1 detected in Rotarix vaccine. Vaccine. 29:690–697. 2011. View Article : Google Scholar | |
|
Smatti MK, Al Thani AA and Yassine HM: Viral-induced enhanced disease illness. Front Microbiol. 9:29912018. View Article : Google Scholar : PubMed/NCBI | |
|
Tetro JA: Is COVID-19 receiving ADE from other coronaviruses? Microbes Infect. 22:72–73. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Xu J, Jia W, Wang P, Zhang S, Shi X, Wang X and Zhang L: Antibodies and vaccines against Middle East respiratory syndrome coronavirus. Emerg Microbes Infect. 8:841–856. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Colgrove J: Immunity for the people: The challenge of achieving high vaccine coverage in American history. Public Health Rep. 122:248–257. 2007. View Article : Google Scholar : PubMed/NCBI | |
|
Lord JM: The effect of ageing of the immune system on vaccination responses. Hum Vaccin Immunother. 9:1364–1367. 2013. View Article : Google Scholar : PubMed/NCBI | |
|
Boda D, Docea AO, Calina D, Ilie MA, Caruntu C, Zurac S, Neagu M, Constantin C, Branisteanu DE, Voiculescu V, et al: Human papilloma virus: Apprehending the link with carcinogenesis and unveiling new research avenues (Review). Int J Oncol. 52:637–655. 2018.PubMed/NCBI | |
|
Wiedermann U, Garner-Spitzer E and Wagner A: Primary vaccine failure to routine vaccines: Why and what to do? Hum Vaccin Immunother. 12:239–243. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Leitner WW, Ying H and Restifo NP: DNA and RNA-based vaccines: Principles, progress and prospects. Vaccine. 18:765–777. 1999. View Article : Google Scholar : PubMed/NCBI | |
|
Fehr AR and Perlman S: Coronaviruses: An overview of their replication and pathogenesis. Methods Mol Biol. 1282:1–23. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Perlman S and Netland J: Coronaviruses post-SARS: Update on replication and pathogenesis. Nat Rev Microbiol. 7:439–450. 2009. View Article : Google Scholar : PubMed/NCBI | |
|
Vandamme TF: Use of rodents as models of human diseases. J Pharm Bioallied Sci. 6:2–9. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Fogel DB: Factors associated with clinical trials that fail and opportunities for improving the likelihood of success: A review. Contemp Clin Trials Commun. 11:156–164. 2018. View Article : Google Scholar : PubMed/NCBI |