Prognostic value of obesity in patients with cancer treated with immune checkpoint inhibitors: An updated meta‑analysis and systematic review
- Authors:
- Published online on: November 21, 2023 https://doi.org/10.3892/mco.2023.2703
- Article Number: 5
-
Copyright: © Guo et al. This is an open access article distributed under the terms of Creative Commons Attribution License.
Abstract
Introduction
With the development and increased interest in cancer immunotherapy, immune checkpoint inhibitors (ICIs), including targeting programmed cell death-1 (PD-1), PD-1 ligand 1 (PD-L1) and the checkpoint T lymphocyte-associated protein 4 (CTLA-4), have emerged as a novel therapeutic strategy in certain types of cancer. However, the majority of patients showed no response to ICI therapies and numerous responders eventually developed resistance (1,2). Several biomarkers, including tumor-infiltrating lymphocytes (TILs), tumor mutational burden (TMB) and microsatellite instability (MSI), have been used to select potential responders to ICI therapy. However, these biomarkers were solely focused on tumor features and did not reflect the systemic immune status of patients (3). Therefore, exploring simpler, available patient characteristics, such as body mass index (BMI) or body composition, seems feasible to assess the association with outcomes and response to ICI therapy.
In recent years, the efficacy of ICIs in obese populations with cancer has drawn increased interest from researchers. According to statistics from the World Health Organization (WHO) for 2020, the proportion of overweight and obese individuals older than 18 years within the world population accounted for 39 and 13%, respectively (4). Epidemiological studies have established a strong association between obesity and multiple cancer types. Obesity was determined to be a risk factor for the incidence and progression of certain cancer types (5). While previous research has focused predominantly on the effects of obesity on altered endocrine factors, growth factors and signaling pathways, little is known about its impact on cancer immunotherapy (5). As the number of overweight and obese individuals continues to rise, the influence of obesity on cancer treatment efficacy should not be ignored.
The BMI commonly measures obesity as a marker for the nutritional state (6). Previous clinical studies have indicated that an increased BMI is associated with improved survival of patients with cancer receiving immunotherapy (7-9). For instance, obesity improved the progression-free survival (PFS) and overall survival (OS) of patients with metastatic melanoma who received targeted therapy, immunotherapy or chemotherapy (8). By contrast, another study on metastatic melanoma reported no association between obesity and outcome (10). Whether obesity is a predictive factor regarding survival of patients receiving immunotherapy needs to be further studied. Previous meta-analyses have explored the impact of the BMI on the outcomes of ICI treatment for patients with cancer, but the date of their literature search included only studies published up to 2021 (11-14). Thus, based on the latest literature, the present study aimed to evaluate the predictive value of the BMI in patients with cancer receiving immunotherapy.
As the BMI is calculated from the whole-body weight, it is not the most suitable measure for evaluating obesity (6). Recently, imaging-measured adipose distribution has been investigated to estimate the influence of obesity on the efficacy of ICI therapy. It was reported that a higher fat distribution is associated with improved survival of patients with cancer rather than the BMI (15-17). However, the results appeared to be inconsistent due to the different methods used to evaluate the body's composition. Thus, the potential association between adipose distribution and clinical outcomes in patients with cancer treated with immunotherapy remains controversial. Therefore, another objective of the present study was to explore the association between survival and different types of fat in patients treated with immunotherapy.
Materials and methods
Search strategy
A systematic literature search was conducted using the PubMed (https://pubmed.ncbi.nlm.nih.gov/), MEDLINE (https://www.medline.eu/), EMBASE (https://www.embase.com/) and Cochrane Library (https://www.cochranelibrary.com/) databases for entries of studies published between January 2017 and July 2022, with no language restrictions. The main keywords for the literature search included ‘cancer’, ‘tumor’, ‘oncology’, ‘neoplasm’, ‘body mass index’, ‘BMI’, ‘obesity’, ‘overweight’, ‘weight’, ‘mass’, ‘body composition’, ‘body fat distribution’, ‘adiposity’, ‘fat’, ‘PD-1’, ‘PD-L1’, ‘CTLA-4’, ‘nivolumab’, ‘pembrolizumab’, ‘atezolizumab’, ‘avelumab’, ‘durvalumab’, ‘ipilimumab’, ‘tremelimumab’ and ‘immune checkpoint inhibitor’. Any studies missed by the electronic search were manually searched from references of included studies and relevant systematic reviews. The protocol of the current meta-analysis was registered in the International Prospective Register of Systematic Reviews database (https://www.crd.york.ac.uk/PROSPERO/; accession no. CRD42022344713).
Selection criteria
Two investigators, LXY and WC, independently searched and selected articles for eligibility. If there were any disagreements, all authors jointly re-evaluated these studies. Full-text articles of clinical studies were screened. The inclusion criteria for the meta-analysis were as follows: i) Patients had been diagnosed with cancer and treated with ICIs; ii) based on the BMI, patients were categorized into normal (BMI, 18.5-24.9 kg/m2), overweight (BMI, 25.0-29.9 kg/m2) and obese (BMI, ≥30 kg/m2) or into two groups (BMI <25 kg/m2 and BMI ≥25 kg/m2); iii) the survival outcomes included PFS and OS; and iv) associations between the BMI and OS or PFS were analyzed using Cox proportional hazards regression models and were reported as hazard ratio (HR) and 95% confidence interval (CI). The inclusion criteria for systematic reviews were as follows: i) Studies focused on adipose tissue distribution; ii) body fat was measured by computed tomography (CT); and iii) associations between adiposity and patient survival with cancer immunotherapy were evaluated.
Data extraction
Two authors (GH and FS) independently reviewed and extracted data from the included studies. Any discrepancy was resolved through discussion with all authors. The following data were extracted from each of the included studies in the meta-analysis: i) Name of first author, year of publication, country, sample size, percentage of male patients and study type; ii) cancer type and ICI drugs; iii) BMI cut-off value; and iv) OS and PFS.
Article quality evaluation
The quality of the included studies on the BMI was evaluated using the Newcastle-Ottawa scale (18). Quality was assessed according to the following inclusion criteria: i) representativeness of the exposed; ii) selection of the non-exposed; iii) ascertainment of exposure; iv) demonstration that outcome of interest was not present at the start; v) study controls for age and sex; vi) study controls for any additional factors (chemoradiotherapy, curative resection and drug resistance); vii) assessment of outcome; viii) follow-up time of >36 months; and ix) adequacy of follow-up of cohorts.
Sensitivity and publication bias
Contour-enhanced meta-analysis funnel plots were used to distinguish publication bias from other asymmetry causes. Publication bias was assessed using Begg's and Egger's tests. Sensitivity analysis was conducted by excluding one study at a time.
Statistical analysis
OS and PFS were used to evaluate the clinical outcomes of ICI treatment. The association between BMI and ICI efficacy in patients with cancer was measured by the hazard ratio (HR) with 95% CI. Statistical heterogeneity among the included studies was evaluated using the I2 statistic. I2 values of <40, 40-60, 60-75 and >75% were considered to indicate low, moderate, substantial and considerable heterogeneity, respectively. I2>40% or P<0.1 was considered to indicate statistical heterogeneity. A random-effects model was applied to calculate the summary HR and 95% CI. All analyses were performed with the meta package of R 4.0.5-win software (https://rstudio.com/products/rstudio/). A two-sided P<0.05 was considered to indicate a statistically significant difference.
Results
Study selection
A total of 5,078 studies were retrieved through the initial literature search, with 3,467 studies remaining after removing duplicates. Next, 3,413 articles were excluded through reviewing titles and abstracts. The remaining 54 studies were reviewed and screened according to the present inclusion and exclusion criteria. Finally, 15 studies reporting on the BMI (7-10,15,16,19-27) were included in the current meta-analysis (Fig. 1). The association between body fat and survival was not suitable for meta-analysis. Therefore, 16 studies reporting on body fat (15-17,24,27-38) were included in the systematic review and descriptively summarized in one table.
Characteristics of studies included in the meta-analysis
General information on the included studies reporting on the BMI is presented in Table I. All analyses were published between 2017 and 2022, of which 12 studies were retrospective and 3 studies were prospective. A total of 5,205 male and 3,105 female patients were included in the meta-analysis. The patients in the meta-analysis were from the USA, Canada, Italy, France, Israel, Spain, Australia and Japan. Melanoma was the most commonly reported cancer type. All enrolled patients were at an advanced or metastatic stage. Since the cut-off values for the BMI in the selected studies were not consistent, 8 studies that stratified the patients based on the BMI value into normal weight (18.5-24.9 kg/m2), overweight (25.0-29.9 kg/m2) and obese (≥30 kg/m2) groups were included, as well as 7 studies that divided the patients by their BMI value into BMI <25 kg/m2 and BMI ≥25 kg/m2 groups. With regard to the types of ICIs used, 6 studies used anti-PD-1/PD-L1 monotherapy, 1 study utilized anti-CTLA-4 monotherapy and 8 studies used anti-PD-1/PD-L1 monotherapy or anti-CTLA-4 monotherapy or their combination. The quality of the included studies was assessed with the Newcastle-Ottawa scale, which revealed high or moderate quality of evidence in the included studies (Fig. S1).
Association between BMI and OS in patients with cancer receiving immunotherapy
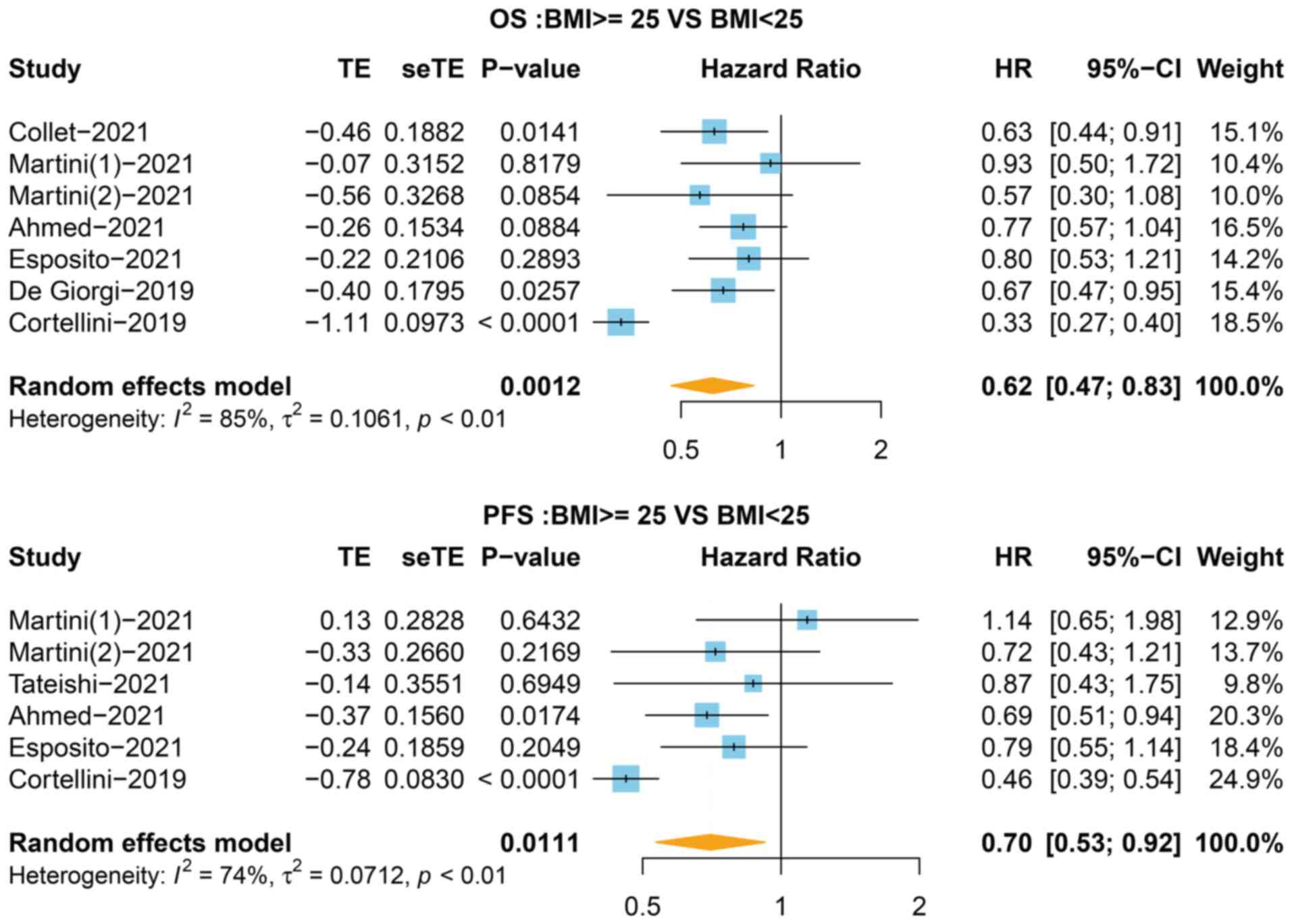
To evaluate the association between BMI and survival, the HR for OS in 7 studies was first analyzed, stratifying the BMI value into <25 and ≥25 kg/m2 groups. As shown in Fig. 2, patients with a BMI ≥25 kg/m2 exhibited increased OS compared with the BMI <25 kg/m2 group (HR=0.62, 95% CI=0.47-0.83, P=0.001, I2=85%). Next, the OS of overweight and obese patients was compared with that of the normal group. The results of the pooled analysis showed that improved OS was observed in the overweight (HR=0.79, 95% CI=0.64-0.98, P=0.030, I2=84%) and obese (HR=0.75, 95% CI=0.60-0.94, P=0.014, I2=76%) groups compared with the normal group (Fig. 3). The heterogeneity test indicated that there was heterogeneity among the studies in terms of OS. Thus, a sensitivity analysis was performed to assess the impact of a single study on the overall outcomes, which revealed that the results were stable (Figs. S2 and S3).
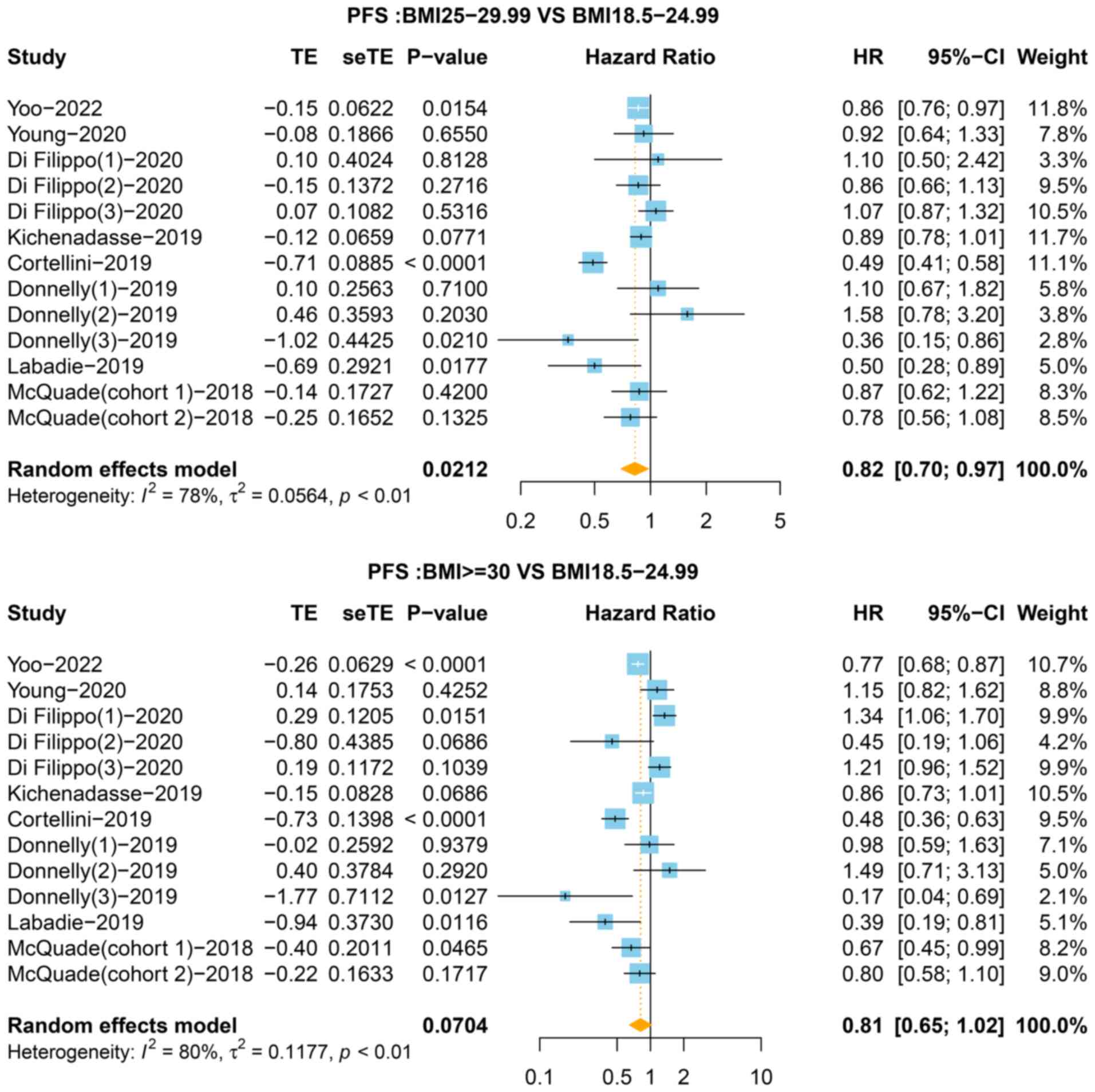
Association between BMI and PFS in patients with cancer receiving immunotherapy
In total, 6 of the 9 studies that stratified the BMI value into <25 and ≥25 kg/m2 groups reported the HR for PFS. As shown in Fig. 2, the BMI ≥25 kg/m2 group was associated with improved PFS (HR=0.70, 95% CI=0.53-0.92, P=0.011) with a high level of heterogeneity (I2=74%). In the third classification, compared with the normal group, the pooled HR for PFS was 0.82 (95% CI=0.70-0.97, P=0.021, I2=78%) for the overweight group and 0.81 (95% CI: 0.65-1.02, P=0.070, I2=80%) for the obese group (Fig. 4). The sensitivity analysis showed that no single study significantly changed the pooled results (Figs. S2 and S4). As presented in Fig. 5, funnel plots showed no significant publication bias in the present meta-analysis.
Characteristics of studies involving body fat and immunotherapy
A total of 16 studies that were published from 2019 to 2022 involving 1,888 patients focused on body fat analysis and were included in the present study. Among them, males accounted for 61.5% of patients. These studies were performed in Asia, North America and Europe. In total, 5 studies were conducted on patients with non-small cell lung cancer (NSCLC) (29-31,34,35); 3 on patients with melanoma (27,33,37); 3 on patients with multiple cancer types (25,28,32); 2 on patients with renal cancer (15,38); 1 on patients with breast cancer (36); 1 on patients with liver cancer (17); and 1 on patients with urothelial cancer (16). The average patient age and immunotherapy drugs were similar in all the studies. Most studies adopted baseline abdominal CT images in the middle of the third lumbar vertebra (mid-L3). Subcutaneous, intermuscular, intramuscular and visceral fat were measured using different segmentation methods. The majority of studies used the Hounsfield unit (HU) value to quantify adipose tissue (-29 to +150 HU for skeletal muscle; -190 to -30 HU for subcutaneous and intermuscular fat; and -150 to -50 HU for visceral fat). Further details are presented in Table II.
Association between body fat and outcomes in patients with cancer receiving immunotherapy
Due to the different parameters and statistical methods, the findings were not consistent. As presented in Table II, in NSCLC, 2 studies showed that subcutaneous adipose tissue (SAT) was associated with prognosis. Popinat et al (29) reported that low subcutaneous fat mass was significantly associated with poor survival (HR=0.75, P=0.006). Degens et al (35) showed that loss of SAT at week 6 of treatment with nivolumab was a significant poor prognostic factor for survival. A total of 4 studies assessed the association between visceral adipose tissue (VAT) and survival (29,31,34,35), but only one of them reported that VAT loss at week 6 of treatment with nivolumab was associated with poor OS (35). Out of 3 studies, 1 study indicated that low body adipose mass was significantly associated with poor survival (HR=0.80, P=0.004) (29). Only 1 study explored the correlation between intramuscular fat and prognosis in NSCLC (31). In addition, 3 studies reported no association between skeletal muscle and survival (30,34,35). These studies indicated that increased body fat, rather than skeletal muscle was associated with improved survival in patients with NSCLC receiving ICI therapy.
In melanoma, SAT was not associated with survival (33). However, increased VAT or total adipose tissue (TAT) predicted favorable survival in patients treated with ICIs (27,37). In renal cell carcinoma (RCC), 1 article showed that low subcutaneous fat index (SFI), low visceral fat index (VFI) or low total fat index (TFI) were associated with significantly inferior survival in metastatic RCC (15). Of note, another article reported no association between body fat and survival in metastatic clear cell RCC (38).
In breast cancer, only 1 study found that a high quantity of subcutaneous or total abdominal fat tissue was a poor prognostic factor in patients receiving trastuzumab/pertuzumab-based first-line treatment for human epidermal growth factor receptor 2 (HER2)-positive metastatic breast cancer (36). Of note, visceral fat was not associated with outcome.
In urothelial carcinoma, only 1 article reported that increased SFI and VFI, and decreased intermuscular fat index (IFI) were associated with improved outcomes in patients treated with immunotherapy (16). In liver cancer, increased VAT and TAT were associated with improved survival rates in patients treated with ICIs (17).
Regarding multiple cancer types, 3 studies presented different results. Esposito et al (25) showed that neither subcutaneous fat area (SFA), visceral fat area (VFA) or total fat area influenced patient survival. However, a higher VFA/SFA ratio led to increased OS in patients treated with ICIs. Martini et al (28) reported that increased SFI and decreased IFI were associated with prolonged survival in patients with cancer treated with immunotherapy. Crombé et al (32) determined that changes in the subcutaneous adipose tissue index from the first day of patients' treatment to 2 months later was associated with survival, while none of the baseline fat parameters were associated with PFS in metastatic cancer patients treated with ICIs.
Discussion
Although obesity has been considered a significant risk factor for developing several types of cancer, it appears to have a contradictory protective effect in patients with cancer treated with targeted therapy, chemotherapy and ICIs (8,39). Thus, this ‘obesity paradox’ has propelled a reconsideration of whether defining obesity by the BMI is correct. It is widely known that obesity is characterized by large fat accumulation. Due to the method of BMI calculation, it cannot correctly distinguish different types of fat (visceral, subcutaneous, intermuscular or intramuscular). Therefore, the present study investigated the association between adiposity and clinical outcomes using the BMI and fat indices in patients with cancer subjected to ICI treatments.
The association between different BMI groups and the OS or PFS of patients with cancer treated with ICIs was first investigated. Through systematic literature screening, the current meta-analysis included 15 eligible studies containing 8,310 patients aimed to assess the impact of the BMI on the efficacy of ICIs. The results revealed that overweight and obese patients with cancer treated with ICIs exhibited improved OS and PFS. According to the weight characteristics of each population, the association between different comparative models of BMI categories and survival was examined in different countries. For instance, several Japanese studies set the cutoff values for the BMI as 18.5 or 20 kg/m2, and it was found that a low BMI was a negative predictive factor in patients with NSCLC or melanoma (40,41). In a Chinese study, the cutoff value for the BMI was 24.0 kg/m2. This study showed that a high BMI was associated with improved OS and PFS in patients treated with PD-1 inhibitors (42). Furthermore, Wang et al (43) observed a marked improvement in the clinical outcomes of obese (BMI ≥30 kg/m2) vs. nonobese (BMI <30 kg/m2) patients in a cohort of 250 US patients treated with PD-L1 inhibitors for a variety of cancer types. All of these studies concluded that the BMI could be a predictive factor of immunotherapy outcomes.
Besides the BMI classification, subgroup analyses based on sex, cancer type, study region and type of ICI have also assessed the efficacy of immunotherapy. Meta-analyses showed that a high BMI was associated with a lower risk of mortality after ICI treatment in multiple cancer types, including NSCLC and melanoma (11,12). By contrast, no consistent results were obtained from these meta-analyses regarding RCC (11-14). When stratifying by sex, the results of the analysis conducted by Xu et al (12) suggested that male and female patients with a high BMI (≥25 kg/m2) who were treated with ICIs exhibited similar survival. However, according to the findings of Chen et al (11), an improvement in OS was observed in male patients with a higher BMI. In addition, the study revealed an association between the survival of patients and treatment with anti-PD1/PD-L1 but not with anti-CTLA-4 therapy. No association was observed between BMI and the survival of American patients (11). The difference in results may be attributed to the absence of a homogeneous cutoff value for the BMI. Therefore, a more standard cutoff value definition was required to stratify by the BMI and reduce heterogeneity between studies. Subgroup analyses based on sex, cancer type, study region and type of ICI should also be conducted to evaluate the influence of the BMI on patient survival after immunotherapy. If all the raw data from the included studies could be obtained, it may be possible to set the optimal cutoff for the BMI using statistical analysis, such as receiver operating characteristic curve analysis.
Tumor heterogeneity has been recognized to be associated with clinical outcomes for ICIs, such PD-L1 protein expression, TILs, TMB and MSI (3). The difference may affect the influence of the BMI on the prognosis of patients with cancer treated with ICIs. In addition, different treatment procedures and regimens for various cancer types may be another factor affecting the relationship between the BMI and cancer survival. Future additional studies are needed to explore the effect of the BMI on the outcomes of different therapy methods for patients with cancer.
The complex body composition cannot be accurately reflected by the BMI alone. It has been reported that a subset of obese patients (BMI ≥30 kg/m2) with a healthy distribution of fat mass and normal inflammatory profile displayed a decreased risk for diseases related to obesity, such as cancer and cardiovascular diseases (44). Another study showed no influence of the BMI on the outcomes of ICI treatment in patients with RCC, while a high body fat mass was a favorable factor for immunotherapy (15). Thus, the prognostic implication of the bodily composition may be more important than that of the BMI in obese patients with cancer treated with ICIs.
Fat composition measurement is mainly based on the calculation of visceral and subcutaneous adipose tissues. Body fat is typically measured via the visceral/subcutaneous adipose area (cm2), area divided by height squared (cm2/m2) or other methods. TAT is generally considered the sum of subcutaneous and visceral adipose tissues. The adipose area can be measured by surface area (cm2) at the third lumbar landmark using a single cross-sectional CT image (45). In the present study, it was observed that the association of imaging-measured visceral, subcutaneous and total adiposity with survival was not consistent in patients with cancer receiving immunotherapy. For patients with NSCLC, RCC and urothelial cancer, increased subcutaneous adiposity was reported to be associated with improved survival (15,16,29,35). Similarly, high visceral adiposity was also associated with an increased survival rate in patients with NSCLC, melanoma, RCC, liver cancer and urothelial cancer (15-17,35,37). In addition, total adiposity was also a favorable factor in patients with NSCLC, melanoma, RCC, breast cancer and liver cancer (15,17,27,29,36). These studies suggested that a high fat distribution may be a good predictor of immunotherapy survival outcome. However, a meta-analysis of the aforementioned studies was not performed due to the inconsistent cutoff values in adipose metrics and the small number of studies on certain cancer types.
The current study confirmed an association between improved survival and high BMI or increased subcutaneous/visceral/total adiposity in patients with cancer receiving immunotherapy. A retrospective study on RCC found that patients with a higher SFI, VFI or TFI showed improved survival, while no influence of the BMI on survival outcomes of immunotherapy was observed (15). Another study on patients with HER2-positive metastatic breast cancer reported no association between BMI and cancer patient survival, but found an association between low SFI or TAFI and better outcomes (36). Based on the currently available data, it may be speculated that the body fat distribution may be strongly associated with the survival of patients with cancer subjected to immunotherapy.
Recently, the underlying mechanisms behind the positive association between obesity and immunotherapy have been explored. Adipose tissue, as an endocrine organ, influences the homeostasis of the immune system by releasing pro-inflammatory hormones such as leptin, tumor necrosis factor (TNF)-α and interleukin (IL)-6(46). A high level of leptin in obese patients may result in increased expression of PD-1 and dysfunction of CD8+ T cells, which leads to a more pronounced response to immunotherapy (43). In addition, it was previously found that increased leptin secreted from adipose tissues may cause upregulation of PD-1 receptors on T cells through signal transduction and activator of transcription 3(47). Elevated PD-1 expression is associated with increased T-cell exhaustion, which may explain why targeted PD-1 therapy may improve survival outcomes in obese populations (48). Obesity induces chronic low-grade inflammation, which is accompanied by innate and adaptive immune suppression and immune aging acceleration (49). For instance, obesity-associated hyperinsulinemia reduced T regulatory cells, thus inhibiting IL-10 and TNF-α production via the AKT/mTOR signaling pathway (50). Natural killer cells, which are responsible for innate immunity and anticancer functions, have been shown to be impaired in obese patients (51). Furthermore, obesity may lead to an imbalance in the ratio of M1/M2 macrophages, thus resulting in an upregulation of M1 ‘pro-inflammatory’ macrophages and a downregulation of M2 ‘anti-inflammatory’ macrophages (52). The above factors caused exacerbation of the chronic inflammatory state. This evidence suggests that alterations of the anti-tumor immune function in obese patients may explain the favorable outcomes of cancer immunotherapy.
Different adipose tissues have various regulatory roles in the body's immune microenvironment and metabolism, which may impact cancer survival. In the present study, one of the articles included reported that increased VAT, but not SAT, predicted favorable survival in patients with liver cancer treated with ICIs (17). A possible explanation for this is that visceral fat may increase a range of inhibitory immune checkpoints on the surface of T cells, including T-cell immunoglobulin and ITIM domain, adenosine A2a receptor, PD-L2 and CD160, which may be beneficial for ICIs to control anticancer immunity (53). A total of 2 studies reviewed in the present study showed that subcutaneous fat was significantly associated with survival, while there was no association between visceral fat and survival (34,38). A potential explanation is that high subcutaneous fat indicates a better nutritional status and it resists the energy consumption caused by tumors. Another reason may be that subcutaneous fat may induce the expression of PD-1 on T cells by secreting leptin, thereby improving the response to immunotherapy (43,54). Further studies are needed to explore the mechanisms of different types of body fat affecting the survival outcomes of immunotherapy.
Several limitations in the current meta-analysis need to be considered. First, certain confounding risk factors across studies, such as age, sex, cancer type and immunotherapy regimen may have increased the heterogeneity among studies. Furthermore, the HR provided in certain studies was not available; thus, these studies were excluded to improve the accuracy of the results. In addition, since certain studies did not stratify the BMI cutoff value according to the WHO, only studies categorizing patients based on the BMI into three groups (normal, overweight and obese) or into two groups (BMI <25 kg/m2 and BMI ≥25 kg/m2) were included, which may have resulted in certain selection bias. Finally, due to the different parameters and statistical methods, the association between body fat and survival was not quantitatively determined by any meta-analysis.
In conclusion, the study of body fat composition as a predictive marker in cancer immunotherapy is an area of compelling interest. Clinical CT scans may provide precise estimates of adipose tissue beyond the BMI for predicting the effectiveness of immunotherapy. Identifying the accurate quantification ability and cutoff values of different indicators of adipose tissue is a challenging endeavor, but it is likely to improve the current understanding of the effects of obesity on cancer patient survival. Body composition evaluation is an effective method for predicting the efficacy of cancer immunotherapy. Defining the biological mechanisms linking obesity and efficacy of immunotherapy will provide guidance for obese patients receiving cancer immunotherapy.
Supplementary Material
Quality assessment of the included studies using the Newcastle-Ottawa scale. «, the study satisfied the item; -, the study did not satisfy the item; RE, representativeness of the exposed; SNE, selection of the non-exposed; AE, ascertainment of exposure; DON, demonstration that outcome of interest was not present at start; SC, study controls for age, sex; SCA, study controls for any additional factors (chemoradiotherapy, curative resection and drug resistance); AO, assessment of outcome; FUL, follow-up time >36 months; AFU, adequacy of follow-up of cohorts.
Sensitivity analysis of the association between BMI (<25 and ≥25 kg/m2 groups) and survival in patients with cancer receiving immunotherapy. BMI, body mass index; IV, inverse variance; PFS, progression-free survival; OS, overall survival.
Sensitivity analysis of the association between BMI (overweight, obese and normal groups) and OS in patients with cancer receiving immunotherapy. BMI, body mass index; IV, inverse variance; OS, overall survival.
Sensitivity analysis of the association between BMI (overweight, obese and normal groups) and PFS in patients with cancer receiving immunotherapy. BMI, body mass index; IV, inverse variance; PFS, progression-free survival.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed in the present study are available from the corresponding author on reasonable request.
Authors' contributions
XYL, SF and CW performed data collection and meta-analysis. HG and LQY completed the systematic review. XGS and DPL contributed to the conception and design of the study. HG and DPL checked and confirmed the authenticity of the raw data. All authors revised the manuscript and read and approved the final version.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
|
Ribas A and Wolchok J: Cancer immunotherapy using checkpoint blockade. Science. 359:1350–1355. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Sharma P, Hu-Lieskovan S, Wargo JA and Ribas A: Primary, adaptive, and acquired resistance to cancer immunotherapy. Cell. 168:707–723. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Gibney GT, Weiner LM and Atkins MB: Predictive biomarkers for checkpoint inhibitor-based immunotherapy. Lancet Oncol. 17:e542–e551. 2016.PubMed/NCBI View Article : Google Scholar | |
|
Friedenreich CM, Ryder-Burbidge C and McNeil J: Physical activity, obesity and sedentary behavior in cancer etiology: Epidemiologic evidence and biologic mechanisms. Mol Oncol. 15:790–800. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Avgerinos KI, Spyrou N, Mantzoros CS and Dalamaga M: Obesity and cancer risk: Emerging biological mechanisms and perspectives. Metabolism. 92:121–135. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Caan BJ, Feliciano EM and Kroenke CH: The importance of body composition in explaining the overweight paradox in cancer-counterpoint. Cancer Res. 78:1906–1912. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Labadie BW, Liu P, Bao R, Crist M, Fernandes R, Ferreira L, Graupner S, Poklepovic AS, Duran I, Vareki SM, et al: BMI, irAE, and gene expression signatures associate with resistance to immune-checkpoint inhibition and outcomes in renal cell carcinoma. J Transl Med. 17(386)2019.PubMed/NCBI View Article : Google Scholar | |
|
McQuade JL, Daniel CR, Hess KR, Mak C, Wang DY, Rai RR, Park JJ, Haydu LE, Spencer C, Wongchenko M, et al: Association of body-mass index and outcomes in patients with metastatic melanoma treated with targeted therapy, immunotherapy, or chemotherapy: A retrospective, multicohort analysis. Lancet Oncol. 19:310–322. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Yoo SK, Chowell D, Valero C, Morris LGT and Chan TA: Outcomes among patients with or without obesity and with cancer following treatment with immune checkpoint blockade. JAMA Netw Open. 5(e220448)2022.PubMed/NCBI View Article : Google Scholar | |
|
Di Filippo Y, Dalle S, Mortier L, Dereure O, Dalac S, Dutriaux C, Leccia MT, Legoupil D, Saiag P, Brunet-Possenti F, et al: Relevance of body mass index as a predictor of systemic therapy outcomes in metastatic melanoma: Analysis of the MelBase French cohort data(✩). Ann Oncol. 32:542–551. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Chen H, Wang D, Zhong Q, Tao Y, Zhou Y and Shi Y: Pretreatment body mass index and clinical outcomes in cancer patients following immune checkpoint inhibitors: A systematic review and meta-analysis. Cancer Immunol Immunother. 69:2413–2424. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Xu H, Cao D, He A and Ge W: The prognostic role of obesity is independent of sex in cancer patients treated with immune checkpoint inhibitors: A pooled analysis of 4090 cancer patients. Int Immunopharmacol. 74(105745)2019.PubMed/NCBI View Article : Google Scholar | |
|
An Y, Wu Z, Wang N, Yang Z, Li Y, Xu B and Sun M: Association between body mass index and survival outcomes for cancer patients treated with immune checkpoint inhibitors: A systematic review and meta-analysis. J Transl Med. 18(235)2020.PubMed/NCBI View Article : Google Scholar | |
|
Nie R, Chen GM, Wang Y, Yuan SQ, Zhou J, Duan J, Liu WW, Chen S, Cai MY and Li YF: Association between body mass index and survival outcomes in patients treated with immune checkpoint inhibitors: Meta-analyses of individual patient data. J Immunother Cancer. 44:371–375. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Martini DJ, Olsen TA, Goyal S, Liu Y, Evans ST, Magod B, Brown JT, Yantorni L, Russler GA, Caulfield S, et al: Body composition variables as radiographic biomarkers of clinical outcomes in metastatic renal cell carcinoma patients receiving immune checkpoint inhibitors. Front Oncol. 11(707050)2021.PubMed/NCBI View Article : Google Scholar | |
|
Martini DJ, Shabto JM, Goyal S, Liu Y, Olsen TA, Evans ST, Magod BL, Ravindranathan D, Brown JT, Yantorni L, et al: Body composition as an independent predictive and prognostic biomarker in advanced urothelial carcinoma patients treated with immune checkpoint inhibitors. Oncologist. 26:1017–1025. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Xiao LS, Li RN, Cui H, Hong C, Huang CY, Li QM, Hu CY, Dong ZY, Zhu HB and Liu L: Use of computed tomography-derived body composition to determine the prognosis of patients with primary liver cancer treated with immune checkpoint inhibitors: a retrospective cohort study. BMC Cancer. 22(737)2022.PubMed/NCBI View Article : Google Scholar | |
|
Stang A: Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 25:603–605. 2010.PubMed/NCBI View Article : Google Scholar | |
|
Kichenadasse G, Miners JO, Mangoni AA, Rowland A, Hopkins AM and Sorich MJ: Association between body mass index and overall survival with immune checkpoint inhibitor therapy for advanced non-small cell lung cancer. JAMA Oncol. 6:512–518. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Ahmed M, von Itzstein MS, Sheffield T, Khan S, Fattah F, Park JY, Popat V, Saltarski JM, Gloria-McCutchen Y, Hsiehchen D, et al: Association between body mass index, dosing strategy, and efficacy of immune checkpoint inhibitors. J Immunother Cancer. 9(e002349)2021.PubMed/NCBI View Article : Google Scholar | |
|
Collet L, Delrieu L, Bouhamama A, Crochet H, Swalduz A, Nerot A, Marchal T, Chabaud S and Heudel PE: Association between body mass index and survival outcome in metastatic cancer patients treated by immunotherapy: Analysis of a French retrospective cohort. Cancers (Basel). 13(2200)2021.PubMed/NCBI View Article : Google Scholar | |
|
Cortellini A, Bersanelli M, Buti S, Cannita K, Santini D, Perrone F, Giusti R, Tiseo M, Michiara M, Di Marino P, et al: A multicenter study of body mass index in cancer patients treated with anti-PD-1/PD-L1 immune checkpoint inhibitors: When overweight becomes favorable. J Immunother Cancer. 7(57)2019.PubMed/NCBI View Article : Google Scholar | |
|
De Giorgi U, Procopio G, Giannarelli D, Sabbatini R, Bearz A, Buti S, Basso U, Mitterer M, Ortega C, Bidoli P, et al: Association of systemic inflammation index and body mass index with survival in patients with renal cell cancer treated with nivolumab. Clin Cancer Res. 25:3839–3846. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Donnelly D, Bajaj S, Yu J, Hsu M, Balar A, Pavlick A, Weber J, Osman I and Zhong J: The complex relationship between body mass index and response to immune checkpoint inhibition in metastatic melanoma patients. J Immunother Cancer. 7(222)2019.PubMed/NCBI View Article : Google Scholar | |
|
Esposito A, Marra A, Bagnardi V, Frassoni S, Morganti S, Viale G, Zagami P, Varano GM, Buccimazza G, Orsi F, et al: Body mass index, adiposity and tumour infiltrating lymphocytes as prognostic biomarkers in patients treated with immunotherapy: A multi-parametric analysis. Eur J Cancer. 145:197–209. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Tateishi A, Horinouchi H, Yoshida T, Masuda K, Jo H, Shinno Y, Okuma Y, Goto Y, Yamamoto N and Ohe Y: Correlation between body mass index and efficacy of anti-PD-1 inhibitor in patients with non-small cell lung cancer. Respir Investig. 60:234–240. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Young AC, Quach HT, Song H, Davis EJ, Moslehi JJ, Ye F, Williams GR and Johnson DB: Impact of body composition on outcomes from anti-PD1 +/- anti-CTLA-4 treatment in melanoma. J Immunother Cancer. 8(e000821)2020.PubMed/NCBI View Article : Google Scholar | |
|
Martini D, Kline M, Liu Y, Shabto J, Williams M, Khan A, Lewis C, Collins H, Akce M, Kissick H, et al: Adiposity may predict survival in patients with advanced stage cancer treated with immunotherapy in phase 1 clinical trials. Cancer. 126:575–582. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Popinat G, Cousse S, Goldfarb L, Becker S, Gardin I, Salaün M, Thureau S, Vera P, Guisier F and Decazes P: Sub-cutaneous Fat Mass measured on multislice computed tomography of pretreatment PET/CT is a prognostic factor of stage IV non-small cell lung cancer treated by nivolumab. Oncoimmunology. 8(e1580128)2019.PubMed/NCBI View Article : Google Scholar | |
|
Magri V, Gottfried T, Di Segni M, Urban D, Peled M, Daher S, Stoff R, Bar J and Onn A: Correlation of body composition by computerized tomography and metabolic parameters with survival of nivolumab-treated lung cancer patients. Cancer Manag Res. 11:8201–8207. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Minami S, Ihara S, Tanaka T and Komuta K: Sarcopenia and visceral adiposity did not affect efficacy of immune-checkpoint inhibitor monotherapy for pretreated patients with advanced non-small cell lung cancer. World J Oncol. 11:9–22. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Crombe A, Kind M, Toulmonde M, Italiano A and Cousin S: Impact of CT-based body composition parameters at baseline, their early changes and response in metastatic cancer patients treated with immune checkpoint inhibitors. Eur J Radiol. 133(109340)2020.PubMed/NCBI View Article : Google Scholar | |
|
Faron A, Opheys NS, Nowak S, Sprinkart AM, Isaak A, Theis M, Mesropyan N, Endler C, Sirokay J, Pieper CC, et al: Deep learning-based body composition analysis predicts outcome in melanoma patients treated with immune checkpoint inhibitors. Diagnostics (Basel). 11(2314)2021.PubMed/NCBI View Article : Google Scholar | |
|
Baldessari C, Pecchi A, Marcheselli R, Guaitoli G, Bonacini R, Valoriani F, Torricelli P, Reverberi L, Menozzi R, Pugliese G, et al: Body composition and inflammation impact in non-small-cell lung cancer patients treated by first-line immunotherapy. Immunotherapy. 13:1501–1519. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Degens J, Dingemans AC, Willemsen ACH, Gietema HA, Hurkmans DP, Aerts JG, Hendriks LEL and Schols A: The prognostic value of weight and body composition changes in patients with non-small-cell lung cancer treated with nivolumab. J Cachexia Sarcopenia Muscle. 12:657–664. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Palleschi M, Iamurri AP, Scarpi E, Mariotti M, Maltoni R, Mannozzi F, Barone D, Paganelli G, Casi M, Giampalma E, et al: Computed tomography based analyses of body mass composition in HER2 positive metastatic breast cancer patients undergoing first line treatment with pertuzumab and trastuzumab. Sci Rep. 12(3385)2022.PubMed/NCBI View Article : Google Scholar | |
|
Lee JH, Hyung S, Lee J and Choi SH: Visceral adiposity and systemic inflammation in the obesity paradox in patients with unresectable or metastatic melanoma undergoing immune checkpoint inhibitor therapy: A retrospective cohort study. J Immunother Cancer. 10(e005226)2022.PubMed/NCBI View Article : Google Scholar | |
|
Ged Y, Sanchez A, Patil S, Knezevic A, Stein E, Petruzella S, Weiss K, Duzgol C, Chaim J, Akin O, et al: Associations between pretreatment body composition features and clinical outcomes among patients with metastatic clear cell renal cell carcinoma treated with immune checkpoint blockade. Clin Cancer Res. 28:5180–5189. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Dahlberg SE, Schiller JH, Bonomi PB, Sandler AB, Brahmer JR, Ramalingam SS and Johnson DH: Body mass index and its association with clinical outcomes for advanced non-small-cell lung cancer patients enrolled on Eastern cooperative oncology group clinical trials. J Thorac Oncol. 8:1121–1127. 2013.PubMed/NCBI View Article : Google Scholar | |
|
Katayama Y, Shimamoto T, Yamada T, Takeda T, Yamada T, Shiotsu S, Chihara Y, Hiranuma O, Iwasaku M, Kaneko Y, et al: Retrospective efficacy analysis of immune checkpoint inhibitor rechallenge in patients with non-small cell lung cancer. J Clin Med. 9(102)2019.PubMed/NCBI View Article : Google Scholar | |
|
Kondo T, Nomura M, Otsuka A, Nonomura Y, Kaku Y, Matsumoto S and Muto M: Predicting marker for early progression in unresectable melanoma treated with nivolumab. Int J Clin Oncol. 24:323–327. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Qi Y, Liao D, Fu X, Gao Q and Zhang Y: Elevated platelet-to-lymphocyte corresponds with poor outcome in patients with advanced cancer receiving anti-PD-1 therapy. Int Immunopharmacol. 74(105707)2019.PubMed/NCBI View Article : Google Scholar | |
|
Wang Z, Aguilar EG, Luna JI, Dunai C, Khuat LT, Le CT, Mirsoian A, Minnar CM, Stoffel KM, Sturgill IR, et al: Paradoxical effects of obesity on T cell function during tumor progression and PD-1 checkpoint blockade. Nat Med. 25:141–151. 2019.PubMed/NCBI View Article : Google Scholar | |
|
Kovarik M, Hronek M and Zadak Z: Clinically relevant determinants of body composition, function and nutritional status as mortality predictors in lung cancer patients. Lung Cancer. 84:1–6. 2014.PubMed/NCBI View Article : Google Scholar | |
|
Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ and Baracos VE: A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab. 33:997–1006. 2008.PubMed/NCBI View Article : Google Scholar | |
|
Mojibi Y, Seif F, Mojibi N, Aghamajidi A, Mohsenzadegan M and Torang HA: Efficacy of immunotherapy in obese patients with cancer. Immunopharmacol Immunotoxicol. 44:471–483. 2022.PubMed/NCBI View Article : Google Scholar | |
|
Bu LL, Yu GT, Wu L, Mao L, Deng WW, Liu JF, Kulkarni AB, Zhang WF, Zhang L and Sun ZJ: STAT3 induces immunosuppression by upregulating PD-1/PD-L1 in HNSCC. J Dent Res. 96:1027–1034. 2017.PubMed/NCBI View Article : Google Scholar | |
|
Woodall MJ, Neumann S, Campbell K, Pattison ST and Young SL: The effects of obesity on anti-cancer immunity and cancer immunotherapy. Cancers (Basel). 12(1230)2020.PubMed/NCBI View Article : Google Scholar | |
|
Aguilar EG and Murphy WJ: Obesity induced T cell dysfunction and implications for cancer immunotherapy. Curr Opin Immunol. 51:181–186. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Han JM, Patterson SJ, Speck M, Ehses JA and Levings MK: Insulin inhibits IL-10-mediated regulatory T cell function: implications for obesity. J Immunol. 192:623–629. 2014.PubMed/NCBI View Article : Google Scholar | |
|
Bahr I, Jahn J, Zipprich A, Pahlow I, Spielmann J and Kielstein H: Impaired natural killer cell subset phenotypes in human obesity. Immunol Res. 66:234–244. 2018.PubMed/NCBI View Article : Google Scholar | |
|
Kraakman MJ, Murphy AJ, Jandeleit-Dahm K and Kammoun HL: Macrophage polarization in obesity and type 2 diabetes: Weighing down our understanding of macrophage function? Front Immunol. 5(470)2014.PubMed/NCBI View Article : Google Scholar | |
|
Davern M, Bracken-Clarke D, Donlon NE, Sheppard AD, O'Connell F, Heeran AB, Majcher K, Conroy MJ, Mylod E, Butler C, et al: Visceral adipose tissue secretome from early and late-stage oesophageal cancer patients differentially affects effector and regulatory T cells. J Cancer Res Clin Oncol. 149:6583–6599. 2023.PubMed/NCBI View Article : Google Scholar | |
|
Porter SA, Massaro JM, Hoffmann U, Vasan RS, O'Donnel CJ and Fox CS: Abdominal subcutaneous adipose tissue: A protective fat depot? Diabetes Care. 32:1068–1075. 2009.PubMed/NCBI View Article : Google Scholar |