IL-32 exacerbates adenoid hypertrophy via activating NLRP3-mediated cell pyroptosis, which promotes inflammation
- Authors:
- Published online on: January 24, 2021 https://doi.org/10.3892/mmr.2021.11865
- Article Number: 226
-
Copyright: © Zhang et al. This is an open access article distributed under the terms of Creative Commons Attribution License.
Abstract
Introduction
Adenoids are lymphatic tissues of the nasopharynx located at the junction of the posterior wall of the nasopharynx and between the pharyngeal recesses on both sides. Adenoids exist from birth, and can gradually shrink after 8–10 years of age under normal physiological conditions (1). Adenoid hypertrophy (AH) is caused when the adenoid is stimulated by repeated inflammation, thus resulting in its pathological hypertrophy (2). AH is a common pediatric disease that may cause a series of local and systemic symptoms, such as nasal congestion, snoring, mouth breathing and obstructive sleep apnea. These symptoms may lead to hypoxia and carbon dioxide retention, thereby affecting children's intellectual development (3). AH can also directly cause mandibular dysplasia, leading to an adenoid facial appearance (4).
The main cause of AH is mainly bacterial virus infection, but there are also other factors, such as allergen stimulation. AH is the hypertrophy of lymphoid tissue (loose connective tissue) and lymphatic follicles, or may also be hypertrophy of mucosal epithelial cells (5). The hypertrophy process is also accompanied by increased numbers of various lymphocytes, which further aggravates the stimulation. The inflammatory stimulation of epithelial cells on the surface of adenoids can directly or indirectly cause rhinitis and sinusitis (6). Inflammatory products that invade the eustachian tube on both sides can cause otitis media (7). However, the related underlying mechanisms of adenoid epithelial cell hypertrophy have not been fully elucidated.
IL-32 is a pro-inflammatory cytokine produced by T lymphocytes, natural killer cells, monocytes and epithelial cells, and its association with airway inflammation has demonstrated in a number of studies (8). For example, IL-32 was identified as an important cytokine involved in the inflammation of allergic rhinitis (AR) (9). Inhibition of IL-32 signaling was shown to attenuate AR in both cellular and animal models (10,11). Elevated levels of IL-32 were also found to play a role in the pathogenesis of rhinosinusitis through its role as a pro-inflammatory cytokine (12). However, whether IL-32 is involved in AH remains to be elucidated.
IL-32 can exert its pro-inflammatory role via numerous pathways or mediators, including p38, MAPK, NF-κB, caspase-1 and caspase-3 (13). In fact, these pathways are interrelated. For example, IL-32 can activate the NF-κB pathway by increasing nucleotide-binding oligomerization domain-containing protein (NOD) 1 and NOD2 expression, therefore promoting NACHT LRR and PYD domains-containing protein 3 (NLRP3) activation and IL-1β production (14). Exogenous activation of NOD1 and NOD2 can also in turn promote the secretion of IL-32, stimulate the activation and release of IL-1β through the caspase-1 pathway and thus further mediate the progression of inflammation (15). Notably, NLRP3-mediated caspase-1 activation was recently confirmed to trigger cell pyroptosis, a form of programmed cell death (16). Moreover, the NLRP3 inflammasome was implicated to promote the development and progression of AR by enhancing inflammatory responses and epithelium pyroptosis (17).
The present study demonstrated IL-32 expression in the adenoid tissues of patients with AH. IL-32 stimulation significantly promoted the production of pro-inflammatory cytokines and cell pyroptosis in human nasal epithelial cells. Meanwhile, silencing of IL-32 significantly inhibited LPS-induced inflammation and pyroptosis.
Materials and methods
Sample collection
The study cohort in the present investigation consisted of 10 children (age range, 6–12 years; 4 female patients and 6 male patients) diagnosed with AH in Tianjin Children's Hospital (Tianjin, China) between February 2019 and June 2019. The diagnosis of AH was based on patient history as well as physical and endoscopic examinations. The normal group consisted of 10 healthy children without AH, but needed required operation on the adenoid due to other reasons. Tissue was collected from the adenoid during surgical operation and immediately stored in liquid nitrogen before use. Parents of the children were informed about the study and signed consent was obtained. The study was approved by the Ethics Committee of Tianjin Children's Hospital (approval no. IACUC-20190111-13).
Cell culture and treatment
Human nasal epithelial cells (HNEpC; RPMI 2650, ATCC-CCL-30; http://www.atcc.org/products/all/CCL-30.aspx), which exhibit epithelioid morphology and have been largely utilized in previous studies as the nasal epithelial cell (18–21), were purchased from American Type Culture Collection. Cells were cultured in DMEM (Invitrogen; Thermo Fisher Scientific, Inc.) supplemented with 10% fetal bovine serum (Gibco; Thermo Fisher Scientific, Inc.), 100 µg/ml streptomycin and 100 U/ml penicillin in an incubator at 37°C.
Cells were cultured overnight to reach 80–90% confluence before transfection. IL-32 small interfering RNA (siRNA) (cat. no. sc-60841) and control siRNA-A (cat. no. sc-37007) were purchased from Santa Cruz Biotechnology, Inc. Transfection was performed using Lipofectamine® 2000 transfection reagent (Invitrogen; Thermo Fisher Scientific, Inc.). All experiments were performed in strict accordance with the manufacturer's instructions. At 48 h post-transfection, the cells were selected for subsequent experiments.
Cell Counting Kit-8 (CCK-8) assay
The cell proliferation of HNEpCs exposed to different concentrations (0, 2, 10 and 50 ng/ml) of recombinant human IL-32 (R&D Systems, Inc.) for 12, 24 and 48 h (22), as well as HNEpCs transfected with IL-32 siRNA or siRNA-negative control (NC) in the presence of lipopolysaccharide (LPS; 1 µg/ml; Beijing Solarbio Science & Technology Co., Ltd.) stimulation for 12, 24 and 48 h, were determined using a CCK-8 assay (cat. no. HY-K0301; MedChemExpress), according to the manufacturer's instructions.
Hematoxylin and eosin (H&E) staining
Adenoid tissues were fixed with 10% formalin (Beyotime Institute of Biotechnology) at 4°C for 24h and embedded in paraffin following alcohol dehydration. The tissues were sliced at a thickness of 4 mm according to the manufacturer's protocol (Leica Autostainer XL; Leica Microsystems, Inc.) and stained with H&E at room temperature for 2 min (Thermo Fisher Scientific, Inc.). Stained samples were observed under light microscopy (magnification, ×200; Olympus FV-1mm; Olympus Corporation).
Immunohistochemical staining
For immunohistochemical analysis, the tissue slides were dewaxed in xylene, rehydrated using graded ethanol, and then heated to expose antigenic sites. Following antigenic retrieval, the sections were incubated overnight at 4°C with diluted rabbit polyclonal antibody against IL-32 (cat. no. ab37158; Abcam; 1:1,000) at a concentration of 10 µg/ml. An HRP-conjugated anti-rabbit secondary antibody (cat. no. ab6721; Abcam; 1:1,000) were used and detected with peroxidase-labelled streptavidin, both incubated for 10 min at room temperature. Immunoreactivity was visualized by incubating the sections for 2 min in 0.1% 3,3′-diaminobenzidine (Beyotime Institute of Biotechnology). The sections were observed under a light microscope (Carl Zeiss AG) and photographed with a digital camera (AxioCam MRc5; Zeiss AG). IL-32 expression is shown by a brown or dark brown stain, while blue staining indicates negative expression. The darker the brown color, the higher the expression of IL-32.
Flow cytometry
Cell apoptosis was measured using flow cytometry analysis based on an Annexin V-FITC Apoptosis Detection kit (Sigma-Aldrich; Merck KGaA) according to the manufacturer's protocol. In brief, HNEpCs and cells transfected with siRNA-IL-32 were seeded at a density of 1×105 cells/well in a six-well culture plate and treated with IL-32 or LPS. The cells were then harvested with 0.25% trypsin, washed twice with cold PBS and suspended in 500 µl binding buffer that was included in the kit. The cells were then incubated with 500 µl Annexin V and 500 µl propidium iodide reagent in the dark for 20 min. Analysis was performed using a BD FACSAria flow cytometer (Becton, Dickinson and Company) and iSort Automated Cell Sorter software (version A.0; Thermo Fisher Scientific, Inc.).
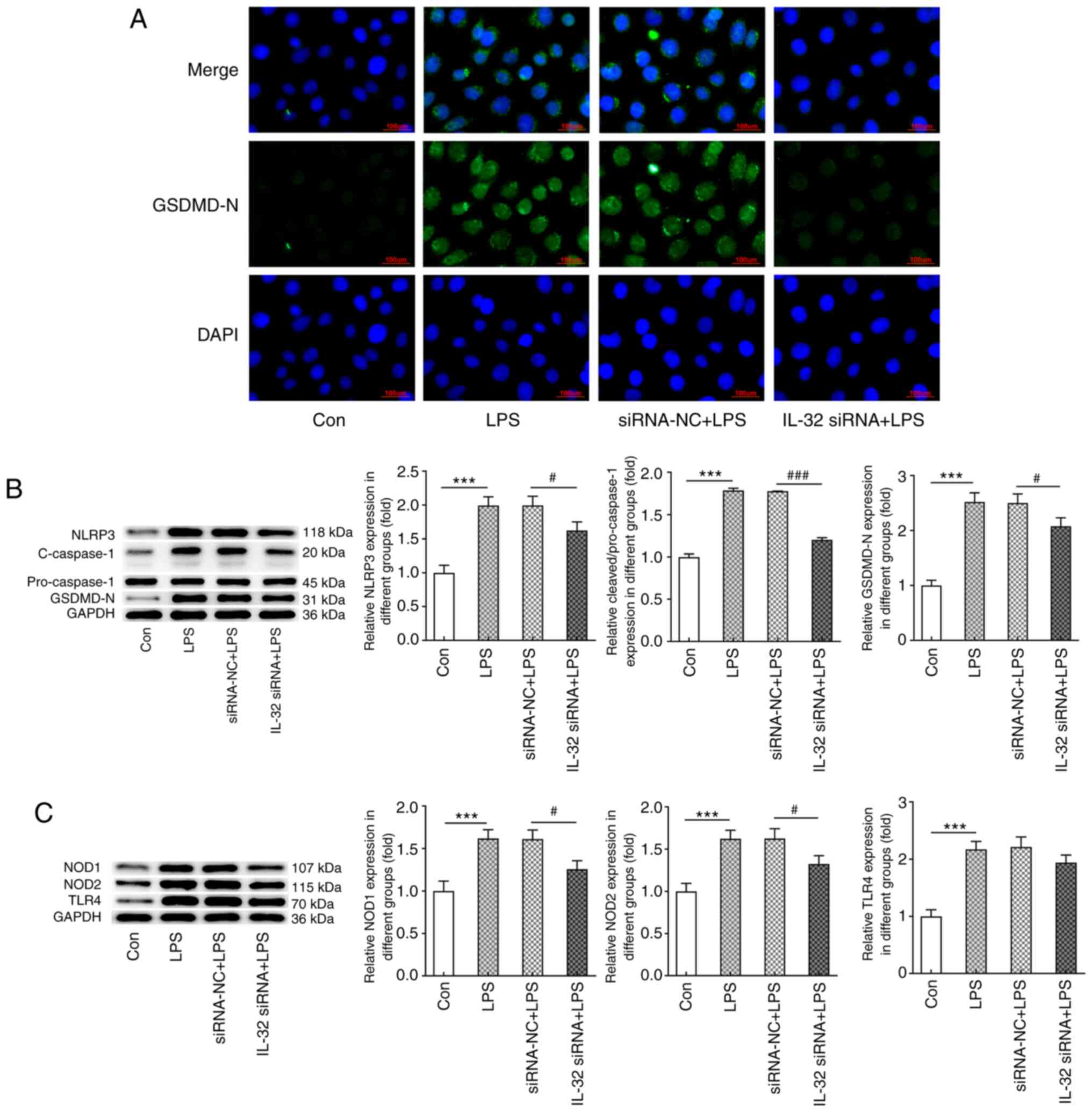
Immunofluorescence (IF) staining
The expression of cleaved gasdermin D (GSDMD) was detected by IF staining. In brief, cells were exposed to 4% paraformaldehyde for 20 min and then blocked with 1% BSA (Gibco; Thermo Fisher Scientific, Inc.) and 0.1% Triton-X for 2 h at room temperature. Subsequently, the cells were incubated with primary antibody against the N-terminal of GSDMD (GSDMD-N; cat. no. ab215203; 1:1,000; Abcam) at 4°C overnight, followed by incubation with goat anti-rabbit IgG-H&L secondary antibody (cat. no. ab150077; 1:500; Abcam) for 2 h at room temperature. The nuclei were stained with DAPI (Beyotime Institute of Biotechnology) at room temperature for 5 min. Stained cells were observed using a fluorescence microscope.
ELISA
ELISA kits were used to measure the concentrations of IL-1β (cat. no. ab217608; Abcam), IL-6 (cat. no. ab46027; Abcam) and TNF-α (cat. no. ab181421; Abcam) as per the manufacturer's instructions. Briefly, 50 µl samples or standards were added to appropriate wells. This was followed by the addition of antibody cocktails from the ELISA kits into each well and incubation at room temperature for 1 h. Subsequently, 3,3′,5,5′-tetramethylbenzidine substrate from the kits was added to each well and incubated for 10 min in the dark with shaking at 400 rpm. Following incubation with stop solution, the optical density values of each well were measured at a wavelength of 450 nm using a microplate reader.
Reverse transcription-quantitative PCR (RT-qPCR)
Total RNA was extracted from HNEpCs using TRIzol® reagent (Invitrogen; Thermo Fisher Scientific, Inc.). RT to synthesize cDNA was performed using SuperScript™ III Reverse Transcriptase (Thermo Fisher Scientific, Inc.) according to the manufacturer's protocol. The PCR reaction system was prepared using SYBR® Green Real-Time PCR Master mix (Thermo Fisher Scientific, Inc). The following primers for IL-32 were used: Forward, 5′-GGCTGAGTATTTGTGCCAGG-3′ and reverse, 5′-TATGGCCTGGTGCATTCGG-3′. The following thermocycling conditions were used for qPCR: 95°C for 2 min, followed by 40 cycles of 95°C for 20 sec and 65°C for 40 sec. The expression levels of IL-32 were normalized to the endogenous control GAPDH (forward, 5′-AATGGGCAGCCGTTAGGAAA-3′ and reverse, 5′-AATGGGCAGCCGTTAGGAAA-3′) using the 2−∆∆Cq method (23).
Western blotting
Total protein was extracted from adenoid tissues and HNEpC cells using RIPA lysis buffer (Beyotime Institute of Biotechnology). Following mixing with SDS lysis buffer and boiling, the protein content in cell lysates were measured using BCA Protein Assay reagent (Pierce; Thermo Fisher Scientific, Inc.). Equal amounts of protein (30 µg) were loaded onto 12% SDS-PAGE and separated via electrophoresis, then separated proteins were transferred to PVDF membranes. Following blocking in 5% skimmed milk at room temperature for 2 h, membranes were incubated overnight with primary antibodies against IL-32 (cat. no. ab37158; 1:1,000; Abcam), NLRP3 (cat. no. ab263899; 1:1,000; Abcam), IL-1β (cat. no. ab216995; 1:1,000; Abcam), caspase-1 (cat. no. ab207802; 1:1,000; Abcam), GSDMD-N (cat. no. ab215203; 1:1,000; Abcam), NOD1 (cat. no. ab189435; 1:1,000; Abcam), NOD2 (cat. no. ab31488; 1:500; Abcam), Toll-like receptor 4 (TLR4; cat. no. ab13556; 1:500; Abcam) and GAPDH (cat. no. ab8245; 1:5,000; Abcam). Membranes were then incubated with goat anti-rabbit IgG (cat. no. ab6721; Abcam; 1:2,000) or goat anti-mouse IgG (cat. no. ab6789; Abcam; 1:2,000) secondary antibodies at room temperature for 2 h. Proteins were then visualized using a gel imaging system (Amersham; Cytiva). Protein expression levels were semi-quantified using Image-Pro Plus software (version 6.0; Media Cybernetics, Inc.).
Statistical analysis
All generated data were analyzed using SPSS software (version 22.0; IBM Corp.). All experiments were repeated at least three times. Data are presented as the mean ± SD. An unpaired Student's t-test was conducted for two-group comparisons. One-way ANOVA followed by Tukey's post hoc test was performed to compare between three or more groups. P<0.05 was considered to indicate a statistically significant difference.
Results
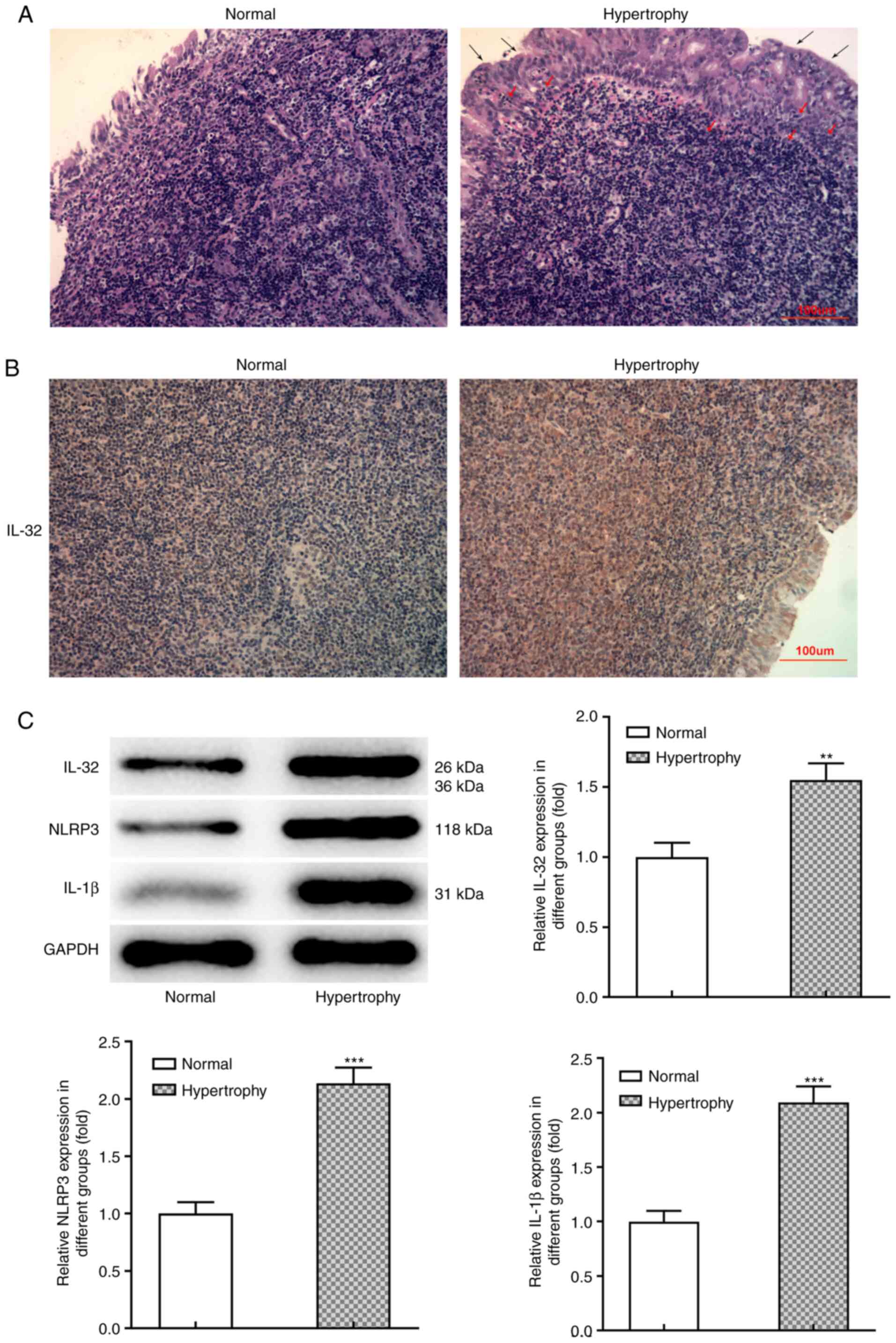
IL-32 is upregulated in adenoid tissues with AH
Firstly, to determine whether IL-32 is involved in AH, IL-32 expression in normal and hypertrophic adenoid tissues was detected. Fig. 1A demonstrates the typical pathological manifestation of hypertrophy and hyperplasia in adenoid tissues from patients with AH. Compared with the normal group, the obvious hypertrophy and lymphocyte infiltration can be observed in the adenoid epithelial tissue of the hyperplasia group. Immunohistochemical analysis (Fig. 1B) revealed that IL-32 expression was markedly upregulated in hypertrophic adenoid tissues compared with normal tissues. Consistently, western blot analysis confirmed higher protein expression of IL-32 in hypertrophic adenoid tissues (Fig. 1C). Meanwhile, the protein expression levels of NLRP3 and IL-1β, which both play important roles in inflammation and pyroptosis, were also significantly increased in hypertrophic adenoid tissues (Fig. 1C). These data indicated that IL-32, together with inflammation and pyroptosis, may contribute to AH progression.
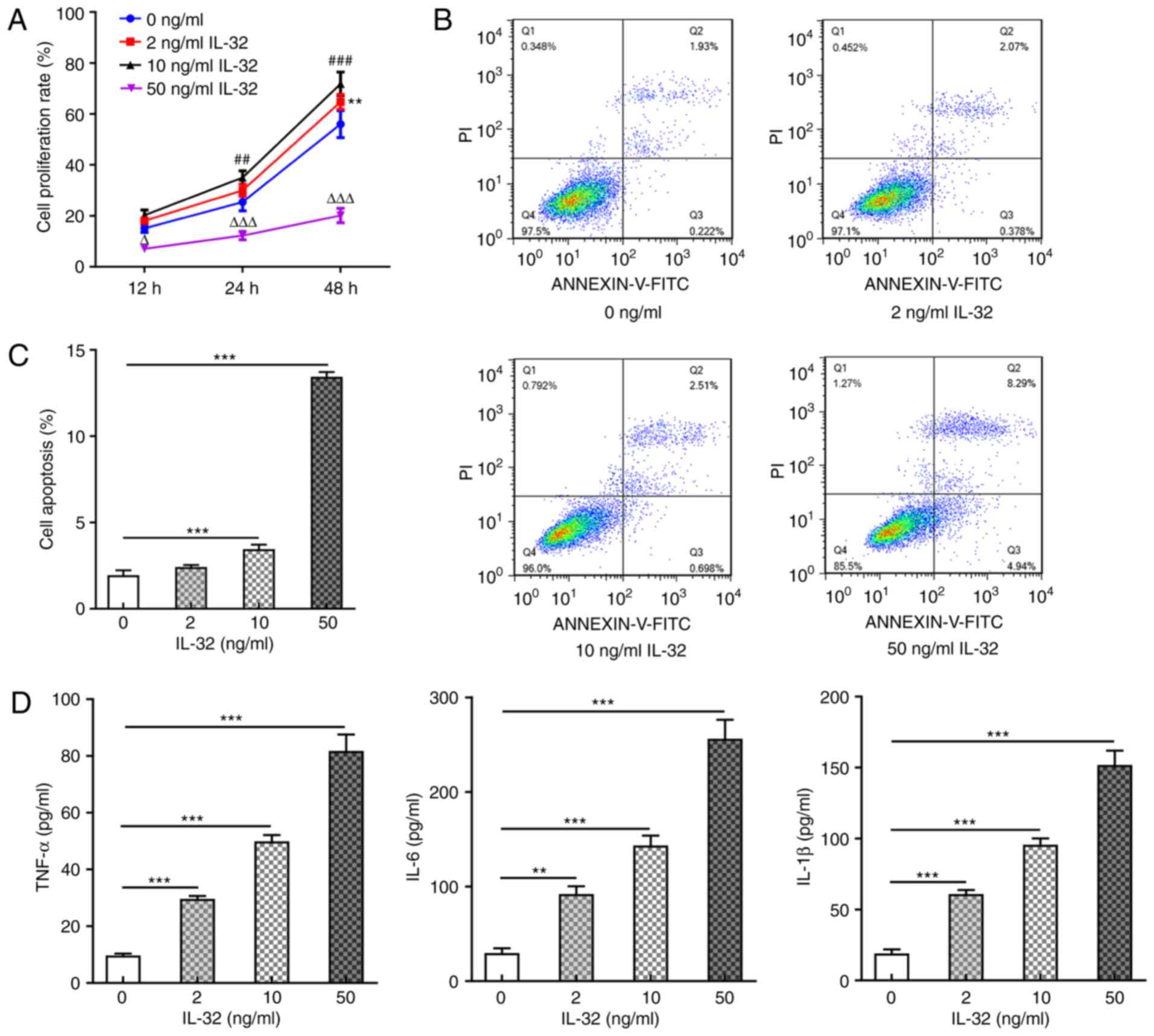
IL-32 induces apoptosis and inflammation
Subsequently, HNEpCs were utilized as the cell model and exposed to different concentrations (0, 2, 10 and 50 ng/ml) of recombinant human IL-32. Fig. 2A shows the cell proliferation rate at 12, 24 and 48 h post IL-32 treatment, revealing that 2 ng/ml IL-32 promoted cell proliferation at 48 h post-treatment, while 10 ng/ml IL-32 significantly promoted cell proliferation at 24 and 48 h post-treatment, owing to the stressful cell proliferation caused by mild inflammation upon IL-1β activation (24). Meanwhile, 50 ng/ml IL-32 significantly inhibited cell proliferation, which can be explained by significant apoptosis or cell death (Fig. 2B and C) caused by 50 ng/ml IL-32 treatment. In the following experiments, cells were exposed to 2, 10 and 50 ng/ml for 48 h. The results shown in Fig. 2B and C revealed that 10 ng/ml IL-32 significantly increased the ratio of cell apoptosis, and 50 ng/ml IL-32 resulted in an especially high ratio of apoptosis (nearly 6-fold of the control). As shown in Fig. 2D, IL-32 also increased the production of pro-inflammatory cytokines, including TNF-α, IL-6 and IL-1β, in a concentration-dependent manner. These results suggested that IL-32 could induce apoptosis and inflammation in normal HNEpCs.
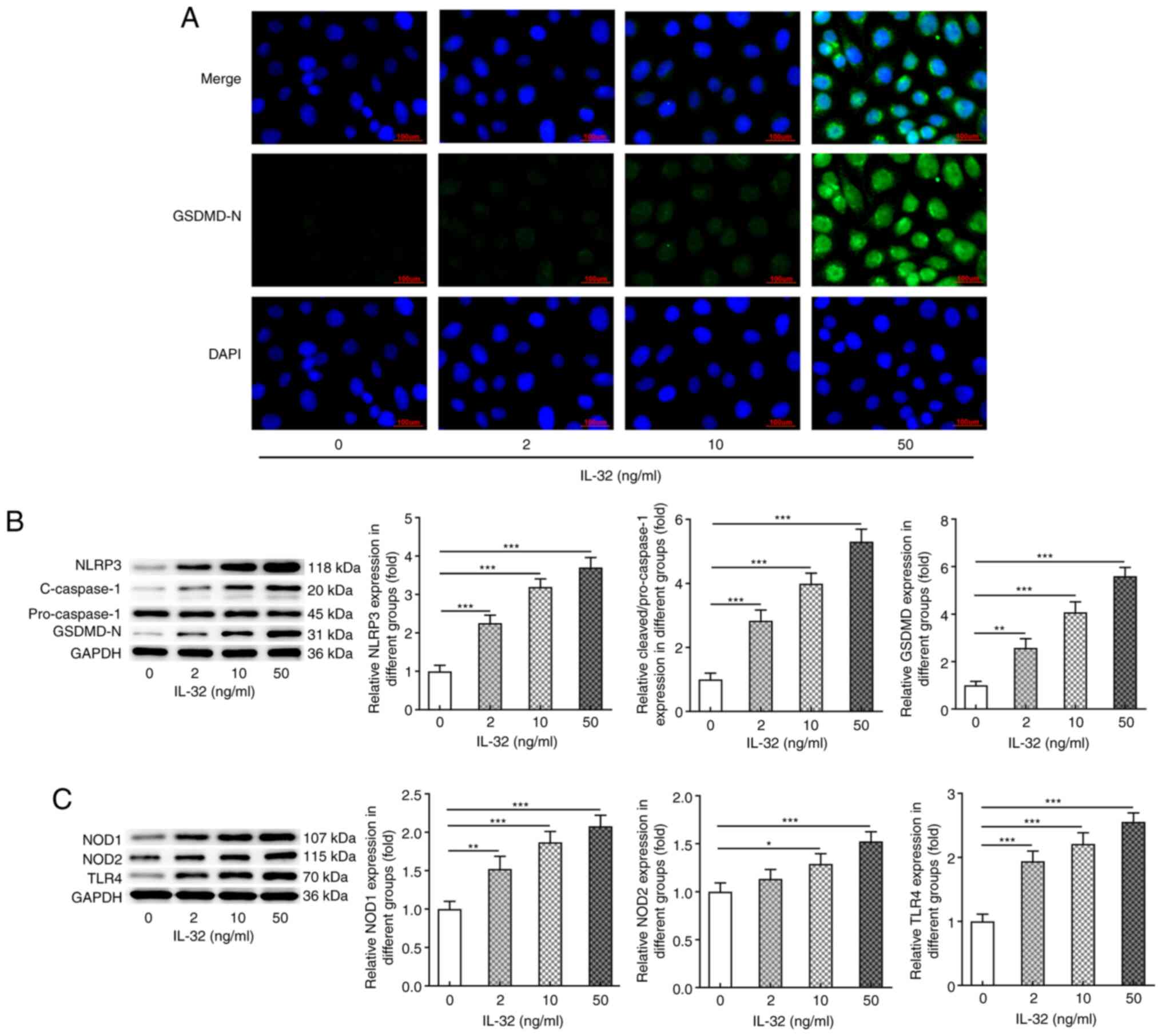
IL-32 promotes NLRP3-mediated pyroptosis
Subsequently, the present study assessed whether IL-32 could induce pyroptosis in HNEpCs. IF staining (Fig. 3A) illustrated that IL-32 stimulation significantly enhanced the activation (cleavage) of GSDMD, suggesting the occurrence of pyroptosis. Similar results were observed in Fig. 3B, which show the protein expression of NLRP3, cleaved-caspase-1 and GSDMD-N in response to IL-32 stimulation. NLRP3, cleaved-caspase-1 and GSDMD-N expression levels were also markedly increased upon IL-32 stimulation. In addition, following exposure to 2, 10 and 50 ng/ml IL-32, the protein expression levels of NOD1, NOD2 and TLR4 were also significantly enhanced (Fig. 3C). The aforementioned data indicated that IL-32 could induce pyroptosis of normal HNEpCs.
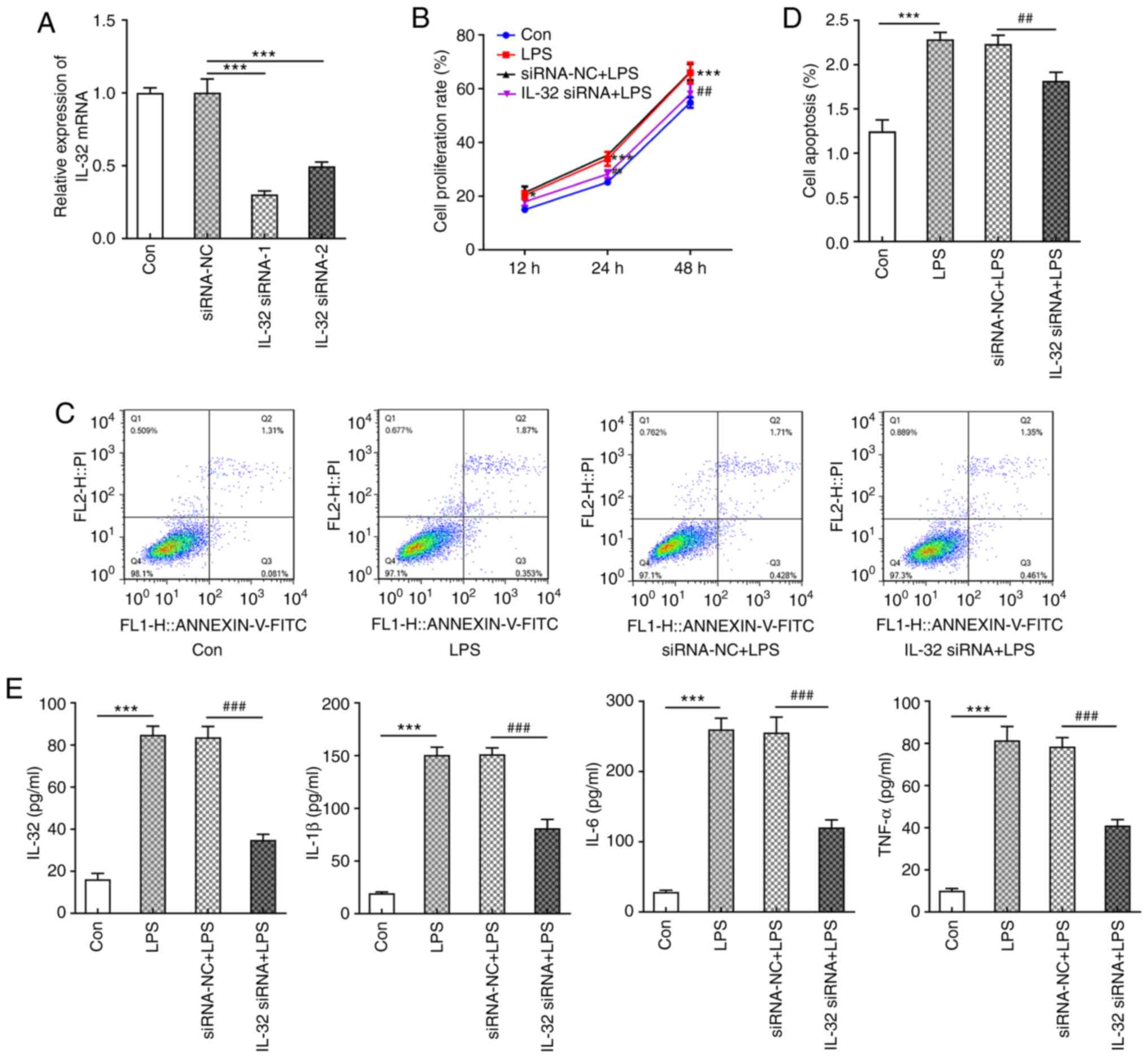
Knockdown of IL-32 inhibits LPS-induced inflammation and pyroptosis
Next, to further examine the modulatory role of IL-32 in AH, IL-32 expression levels in HNEpCs were knocked down using siRNAs. IL-32 siRNA-1 was chosen for subsequent experiments due to its enhanced silencing effects (Fig. 4A). LPS was used to stimulate control HNEpC cells and IL-32 knockdown cells. Similar to low concentrations of IL-32 (2 and 10 ng/ml), LPS also significantly promoted cell proliferation compared with the control group (Fig. 4B). However, cells silenced with IL-32 siRNA-1 in the presence of LPS exerted a lower proliferation rate compared with cells transfected with NC vectors (Fig. 4B). LPS also enhanced the ratio of cell apoptosis, which was reversed by IL-32 knockdown (Fig. 4C and D). In addition, LPS resulted in the production of a large amount of pro-inflammatory cytokines, including IL-32, IL-1β, IL-6 and TNF-α, which was significantly inhibited by IL-32 silencing (Fig. 4E). These results revealed that silencing of IL-32 could inhibit LPS-induced acceleration of proliferation, apoptosis and inflammation.
Finally, the expression levels of proteins involved in NLRP3-mediated pyroptosis were evaluated. As shown in Fig. 5A, cells exerted significantly higher expression of cleaved GSDMD in response to LPS stimulation, while the knockdown of IL-32 markedly inhibited GSDMD activation. As presented in Fig. 5B, LPS also increased the expression of NLRP3, cleaved-caspase-1 and GSDMD-N, which was reversed by IL-32 silencing. As illustrated in Fig. 5C, the LPS-induced enhanced expression of NOD1, NOD2 and TLR4 was notably inhibited by IL-32 knockdown. These data indicated that IL-32 knockdown could effectively inhibit LPS-induced pyroptosis.
Discussion
The inflammatory response has been extensively reported to contribute to the occurrence and progression of AH (7,25). The present study aimed to analyze the association between the pro-inflammatory cytokine IL-32 and AH. IL-32 is a member of the IL family, which are lymphokines that interact between leukocytes or immune cells (13). To the best of our knowledge, the present study is the first to evaluate the association between IL-32 and AH. The results from the present study suggested the close association between IL-32 and AH pathogenesis as well as LPS-induced HNEpC injury.
Adenoids are considered to be essential parts of the system that protect organisms from pathogens. It is known that human adenoids are immunoreactive lymphoid organs, which exhibit specific antibodies together with B and T cell activities in response to various antigens performing the functions of humoral and cellular immunity (26). These are extremely important for the growth and development of children (26). At present, adenoidectomy is a direct and preferred method to solve AH in children, but it may bring risks and complications, including postoperative bleeding, nasopharyngeal stenosis and velopharyngeal insufficiency (27). Another possible risk is that removing adenoid tissue may result in a negative impact on immune function (28). These factors indicate the urgency to discover more suitable treatments.
ILs consist of a large family that can transmit information, activate and regulate immune cells, mediate the activation, proliferation and differentiation of T and B cells and play an important role in inflammation. In addition to IL-32, numerous other IL members have also been illustrated to regulate airway inflammation (29–31). For example, IL-17A was found to be upregulated in adenoid tissues from patients with AH and pneumococcal carriage (32). IL-33 plays a role in the pathophysiology of chronic rhinosinusitis (30). These data indicate the modulatory role of ILs in AH and other types of airway inflammation. The present study found that IL-32, together with NLRP3 and IL-1β, were significantly upregulated in AH tissues, indicating their role in AH. Subsequently, it was found that treatment with low concentrations of IL-32 (2 and 10 ng/ml) could promote HNEpC proliferation, while higher concentrations of IL-32 (50 ng/ml) inhibited cell proliferation. This can be explained by the stressful cell proliferation caused by mild inflammation upon low concentrations of IL-32 (2 and 10 ng/ml) stimulation (24), but predominant apoptosis or cell death caused by high concentration of IL-32 (50 ng/ml) treatment. The present study showed that IL-32 significantly enhanced apoptosis, inflammation and the expression of proteins involved in pyroptosis in a concentration-dependent manner.
Pyroptosis is a newly discovered programmed cell death. It can cause excessive inflammation and immune response in tissues, which in turn results in local and even systemic inflammation and immunopathological damage (33). Pyroptosis can be divided into classical and non-classical pathways according to its recognition mechanisms, reactants and reaction pathways (16). Among both, GDSMD cleavage can expose its N domain with pore-forming activities, which forms a large pore in the membrane that induces pyroptosis (16). Meanwhile, the activation of inflammasome NLRP3 induced by GSDMD-N and external stimuli can trigger caspase-1 activation, thereby resulting in the release of a large number of pro-inflammatory cytokines, ultimately aggravating inflammation (17). The present results showed that IL-32 increased GSDMD-N, NLRP3 and cleaved-caspase-1 expression in HNEpCs, suggesting that IL-32 triggered pyroptosis in HNEpCs. TLRs and NOD-like receptors are two major pattern recognition receptors that provide responses against pathogenic invasion or tissue injury (34). It has been reported that TLR4, NOD1 and NOD2 are also associated with airway inflammation (35). The present study found that IL-32 also promoted TLR4, NOD1 and NOD2 expression in a concentration-dependent manner. Notably, NOD1/2 and TLR4 are known to activate NF-κB signaling, which is able to trigger NLRP3 activation (36–37). Therefore, the present results indicated that IL-32 could also induce inflammation and NLRP3-mediated pyroptosis by activating pattern recognition receptors.
To further verify the present hypothesis, IL-32 expression was silenced in HNEpCs stimulated with LPS using siRNA. Similar to IL-32, LPS significantly triggered high proliferation, apoptosis, inflammation and activation of GSDMD, NLRP3, caspase-1, NOD1/2 and TLR4. Besides, IL-32 knockdown significantly inhibited all effects induced by LPS, revealing the protective effects of IL-32 knockdown against LPS-induced injury in HNEpCs. To the best of our knowledge, the present study is the first to identify IL-32 as an important inflammatory cytokine involved in AH inflammation. However, this study were only carried out in a cell model, thus it lacks the validation of in vivo models. Future research will aim to verify these findings using in vivo experiments and uncover the specific underlying mechanisms involved in the actions of IL-32 in AH.
Taken together, the results of the present study demonstrated that during AH and upon LPS exposure, adenoid tissues and nasal epithelial cells released IL-32, which then regulated apoptosis and excretion of inflammatory cytokines via activation of the NOD1/2/TLR4/NLRP3 pathway, ultimately leading to pyroptosis. Approaches targeting IL-32 to downregulate its expression may provide novel therapeutic targets for AH. However, further in vivo and clinical investigations need to be performed.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
JZ and XS conceived and designed the study. JZ, XS, LZ and BS acquired and analyzed the data. JZ and XS confirmed the authenticity of all the raw data. JZ prepared the draft of the manuscript, including the figures. All authors read and approved the final manuscript.
Ethics approval and consent to participate
All experimental procedures were approved by the Ethical Committee of the Tianjin Children's Hospital (Tianjin, China). The parents of the children were informed about the study and consent was obtained.
Patient consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
References
|
Coca-Pelaz A, Rodrigo JP, Bradley PJ, Vander Poorten V, Triantafyllou A, Hunt JL, Strojan P, Rinaldo A, Haigentz M Jr, Takes RP, et al: Adenoid cystic carcinoma of the head and neck - An update. Oral Oncol. 51:652–661. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Buzatto GP, Tamashiro E, Proenca-Modena JL, Saturn TH, Prates MC, Gagliardi TB, Carenzi LR, Massuda ET, Hyppolito MA, Valera FC, et al: The pathogens profile in children with otitis media with effusion and adenoid hypertrophy. PLoS One. 12:e01710492017. View Article : Google Scholar : PubMed/NCBI | |
|
Durgut O and Dikici O: The effect of adenoid hypertrophy on hearing thresholds in children with otitis media with effusion. Int J Pediatr Otorhinolaryngol. 124:116–119. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Stupak HD and Park SY: Gravitational forces, negative pressure and facial structure in the genesis of airway dysfunction during sleep: A review of the paradigm. Sleep Med. 51:125–132. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Scadding G: Non-surgical treatment of adenoidal hypertrophy: the role of treating IgE-mediated inflammation. Pediatr Allergy Immunol. 21:1095–1106. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
Gulotta G, Iannella G, Vicini C, Polimeni A, Greco A, de Vincentiis M, Visconti IC, Meccariello G, Cammaroto G, De Vito A, et al: Risk factors for obstructive sleep apnea syndrome in children. Int J Environ Res Public Health. 16:32352019. View Article : Google Scholar | |
|
Marazzato M, Zicari AM, Aleandri M, Conte AL, Longhi C, Vitanza L, Bolognino V, Zagaglia C, De Castro G, Brindisi G, et al: 16S metagenomics reveals dysbiosis of nasal core microbiota in children with chronic nasal inflammation: Role of adenoid hypertrophy and allergic rhinitis. Front Cell Infect Microbiol. 10:4582020. View Article : Google Scholar : PubMed/NCBI | |
|
Hong JT, Son DJ, Lee CK, Yoon DY, Lee DH and Park MH: Interleukin 32, inflammation and cancer. Pharmacol Ther. 174:127–137. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Jeong HJ, Shin SY, Oh HA, Kim MH, Cho JS and Kim HM: IL-32 up-regulation is associated with inflammatory cytokine production in allergic rhinitis. J Pathol. 224:553–563. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Nam SY, Oh HA, Choi Y, Park KY, Kim HM and Jeong HJ: Inhibition of IL-32 signaling by bamboo salt decreases pro-inflammatory responses in cellular models of allergic rhinitis. J Med Food. 17:939–948. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Jeong HJ, Oh HA, Lee BJ and Kim HM: Inhibition of IL-32 and TSLP production through the attenuation of caspase-1 activation in an animal model of allergic rhinitis by Naju Jjok (Polygonum tinctorium). Int J Mol Med. 33:142–150. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Keswani A, Kern RC, Schleimer RP and Kato A: Role of interleukin-32 in chronic rhinosinusitis. Curr Opin Allergy Clin Immunol. 13:13–18. 2013. View Article : Google Scholar : PubMed/NCBI | |
|
Kim SH, Han SY, Azam T, Yoon DY and Dinarello CA: Interleukin-32: A cytokine and inducer of TNFalpha. Immunity. 22:131–142. 2005. View Article : Google Scholar : PubMed/NCBI | |
|
Pan X, Cao H, Lu J, Shu X, Xiong X, Hong X, Xu Q, Zhu H, Li G and Shen G: Interleukin-32 expression induced by hepatitis B virus protein X is mediated through activation of NF-κB. Mol Immunol. 48:1573–1577. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Lu J, Fang K, Wang S, Xiong L, Zhang C, Liu Z, Guan X, Zheng R, Wang G, Zheng J, et al: Anti-inflammatory effect of columbianetin on lipopolysaccharide-stimulated human peripheral blood mononuclear cells. Mediators Inflamm. 2018:91917432018. View Article : Google Scholar : PubMed/NCBI | |
|
Wang S, Yuan YH, Chen NH and Wang HB: The mechanisms of NLRP3 inflammasome/pyroptosis activation and their role in Parkinson's disease. Int Immunopharmacol. 67:458–464. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Yang Z, Liang C, Wang T, Zou Q, Zhou M, Cheng Y, Peng H, Ji Z, Deng Y, Liao J, et al: NLRP3 inflammasome activation promotes the development of allergic rhinitis via epithelium pyroptosis. Biochem Biophys Res Commun. 522:61–67. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Hu H and Li H: Prunetin inhibits lipopolysaccharide-induced inflammatory cytokine production and MUC5AC expression by inactivating the TLR4/MyD88 pathway in human nasal epithelial cells. Biomed Pharmacother. 106:1469–1477. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Tsou YA, Tung YT, Wu TF, Chang GRL, Chen HC, Lin CD, Lai CH, Chen HL and Chen CM: Lactoferrin interacts with SPLUNC1 to attenuate lipopolysaccharide-induced inflammation of human nasal epithelial cells via down-regulated MEK1/2-MAPK signaling. Biochem Cell Biol. 95:394–399. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Li YQ, Zhong Y, Xiao XP, Li DD, Zhou Z and Tian YY: IL-33/ST2 axis promotes the inflammatory response of nasal mucosal epithelial cells through inducing the ERK1/2 pathway. Innate Immun. 26:505–513. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Nian JB, Zeng M, Zheng J, Zeng LY, Fu Z, Huang QJ and Wei X: Epithelial cells expressed IL-33 to promote degranulation of mast cells through inhibition on ST2/PI3K/mTOR-mediated autophagy in allergic rhinitis. Cell Cycle. 19:1132–1142. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Lin J, Xu R, Hu L, You J, Jiang N, Li C, Che C, Wang Q, Xu Q, Li J, et al: Interleukin-32 induced thymic stromal lymphopoietin plays a critical role in the inflammatory response in human corneal epithelium. Cell Signal. 49:39–45. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Livak KJ and Schmittgen TD: Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 25:402–408. 2001. View Article : Google Scholar : PubMed/NCBI | |
|
Kiraly O, Gong G, Olipitz W, Muthupalani S and Engelward BP: Inflammation-induced cell proliferation potentiates DNA damage-induced mutations in vivo. PLoS Genet. 11:e10049012015. View Article : Google Scholar : PubMed/NCBI | |
|
Anfuso A, Ramadan H, Terrell A, Demirdag Y, Walton C, Skoner DP and Piedimonte G: Sinus and adenoid inflammation in children with chronic rhinosinusitis and asthma. Ann Allergy Asthma Immunol. 114:103–110. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Sun YL, Zheng HT, Tao JL, Jiang MC, Hu CC, Li XM and Yuan B: Effectiveness and safety of Chinese herbal medicine for pediatric adenoid hypertrophy: A meta-analysis. Int J Pediatr Otorhinolaryngol. 119:79–85. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Richter GT and Bower CM: Cervical complications following routine tonsillectomy and adenoidectomy. Curr Opin Otolaryngol Head Neck Surg. 14:375–380. 2006. View Article : Google Scholar : PubMed/NCBI | |
|
van den Akker EH, Sanders EA, van Staaij BK, Rijkers GT, Rovers MM, Hoes AW and Schilder AG: Long-term effects of pediatric adenotonsillectomy on serum immunoglobulin levels: Results of a randomized controlled trial. Ann Allergy Asthma Immunol. 97:251–256. 2006. View Article : Google Scholar : PubMed/NCBI | |
|
Rogala B and Glück J: The role of interleukin-33 in rhinitis. Curr Allergy Asthma Rep. 13:196–202. 2013. View Article : Google Scholar : PubMed/NCBI | |
|
Kim DK, Jin HR, Eun KM, Mo JH, Cho SH, Oh S, Cho D and Kim DW: The role of interleukin-33 in chronic rhinosinusitis. Thorax. 72:635–645. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Luo XQ, Ma F, Wang S, Zhao MZ, Shao JB, Geng XR, Liu JQ, Mo LH, Guan L, Liu ZG, et al: Interleukin-5 induces apoptotic defects in CD4+ T cells of patients with allergic rhinitis. J Leukoc Biol. 105:719–727. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Huang CC, Wu PW, Chen CL, Wang CH, Lee TJ, Tsai CN and Chiu CH: IL-17A expression in the adenoid tissue from children with sleep disordered breathing and its association with pneumococcal carriage. Sci Rep. 8:167702018. View Article : Google Scholar : PubMed/NCBI | |
|
Bergsbaken T, Fink SL and Cookson BT: Pyroptosis: Host cell death and inflammation. Nat Rev Microbiol. 7:99–109. 2009. View Article : Google Scholar : PubMed/NCBI | |
|
Keestra-Gounder AM, Byndloss MX, Seyffert N, Young BM, Chávez-Arroyo A, Tsai AY, Cevallos SA, Winter MG, Pham OH, Tiffany CR, et al: NOD1 and NOD2 signalling links ER stress with inflammation. Nature. 532:394–397. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Di Stefano A, Ricciardolo FLM, Caramori G, Adcock IM, Chung KF, Barnes PJ, Brun P, Leonardi A, Andò F, Vallese D, et al: Bronchial inflammation and bacterial load in stable COPD is associated with TLR4 overexpression. Eur Respir J. 49:16020062017. View Article : Google Scholar : PubMed/NCBI | |
|
Luo M, Yan D, Sun Q, Tao J, Xu L, Sun H and Zhao H: Ginsenoside Rg1 attenuates cardiomyocyte apoptosis and inflammation via the TLR4/NF-κB/NLRP3 pathway. J Cell Biochem. 121:2994–3004. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Aabdin ZU, Bilal MS, Dai H, Abaker JA, Liu X, Benazir S, Yan J and Shen X: NOD1/NF-κB signaling pathway inhibited by sodium butyrate in the mammary gland of lactating goats during sub-acute ruminal acidosis. Microb Pathog. 122:58–62. 2018. View Article : Google Scholar : PubMed/NCBI |