miRNAs as predictive biomarkers of response to treatment in pediatric patients with acute lymphoblastic leukemia
- Authors:
- Published online on: December 21, 2023 https://doi.org/10.3892/ol.2023.14204
- Article Number: 71
-
Copyright: © Tsotridou et al. This is an open access article distributed under the terms of Creative Commons Attribution License.
Abstract
Introduction
Acute leukemia constitutes the most common malignancy in childhood, accounting for ~25% of new cancer cases in the USA (1). There are ~0.6 deaths/100,000 per year attributed to the disease, with the highest rate recorded in adolescents aged 15–19 years (1). Acute lymphoblastic leukemia (ALL) accounts for ~85% of leukemia cases in childhood (2). Survival rates have increased over previous decades and are >90% at present, an improvement which can be attributed to the implementation of efficacious risk-adapted treatment, high-dose chemotherapy, novel targeted therapies and advances in supportive care (2). Currently, risk stratification is based on demographic characteristics (age and sex), and clinical (presence of extramedullary disease) and laboratory [number of white blood cells (WBCs) at diagnosis, karyotype and cytogenetic findings] parameters. Regarding cytogenetic findings, it is noteworthy that the presence of the translocation (12;21)(p13;q22), which gives rise to the fusion gene erythroblast transformation specific (ETS) variant transcription factor 6 (ETV6)-RUNX family transcription factor 1 (RUNX1; previously known as translocation-Ets-leukemia-acute myeloid leukemia 1 protein), which occurs in ~25% of pediatric patients with ALL, is associated with a favorable prognosis and is part of the risk stratification system of chemotherapeutic protocols (3). Response to treatment during induction is assessed based on the number of blasts in the peripheral blood on day 8 of the therapeutic protocol and the minimal residual disease (MRD) on day 15 and 33 of the therapeutic protocol (3). However, relapsed or refractory disease still poses a therapeutic challenge, as it remains one of the most common causes of mortality attributed to disease in childhood. The event-free-survival and overall survival rates of relapsed patients with B-ALL and T-ALL do not exceed 33% even with the use of the new protocols (4). Furthermore, the fact that patients with favorable prognosis according to the established criteria do not exhibit the anticipated response to treatment, while at the same time a subset of patients is overtreated (in risk of treatment-associated toxicities), underlines the need for additional prognostic factors that can be used for risk stratification (5,6).
MicroRNAs (miRNAs/miRs) are small (19–22 nucleotides), endogenous, non-coding, single-stranded RNA molecules that act as epigenetic regulators and are implicated in several biological processes, including cell division, differentiation and death, thus guarding cell homeostasis (7). Therefore, disruption of normal miRNA expression can lead to oncogenesis and aberrant miRNA expression has been implicated in a plethora of solid tumors, including breast, cervical, ovarian, prostate, lung, colorectal and brain cancer, as well as in hematological malignancies (7). Multiple miRNAs regulate hematopoiesis lineage differentiation (8). Particularly, in pediatric ALL, the miRNA expression profile has been evaluated as a marker for diagnosis and classification, as well as to determine prognosis (9–11). Recently, miRNAs have also been proposed as therapeutic targets in leukemia (12). However, the high heterogeneity among studies hinders the recognition of a set of miRNAs that can be effectively used for risk stratification and assessment of response to treatment.
The aim of the present pilot study was to assess the miRNA expression profile in bone marrow aspirates of pediatric patients with newly diagnosed ALL at two crucial time points: i) At diagnosis (day 0 of induction therapy); and ii) at day 33 [end of induction therapy in the Acute Lymphoblastic Leukemia Intercontinental Berlin-Frankfurt-Münster (ALL IC BFM) 2009 protocol (13)]. Additionally, the present study aimed to evaluate the association of miRNA expression levels with established prognostic factors, to identify miRNAs that could be used as prognostic biomarkers or are involved in the mechanisms underlying resistance to therapy and that could serve as novel therapeutic targets. To the best of our knowledge, the present study was the first to assess such a large number of candidate miRNAs in the bone marrow not only at diagnosis, but also at the end of induction, in a Greek population. The set of miRNAs used in the present study comprised 84 miRNAs that have been previously associated with tumorigenesis, but the majority of them had not been studied in pediatric acute lymphoblastic leukemia.
Materials and methods
Clinical samples
Patients aged <18 years with newly diagnosed ALL and no history of malignancy or autoimmune disease were enrolled between October 2021 and October 2022. Patients were diagnosed and treated in the pediatric hematology units of AHEPA University Hospital (Thessaloniki, Greece) and Hippokration General Hospital (Thessaloniki, Greece). A total of 10 patients who fulfilled the inclusion criteria were included in the study. A total of 4 patients were excluded due to unavailable samples (bone marrow aspirates) either at diagnosis or on day 33 of induction. All patients were treated according to the ALL IC BFM 2009 protocol. The biological samples included two bone marrow aspirates in EDTA-containing tubes for each patient obtained at diagnosis (day 0 of induction therapy) and at day 33 (end of induction therapy). Sample collection and storage complied with the General Data Protection Regulation. The present study was approved by the Committee for Bioethics and Ethics of the School of Medicine of the Aristotle University of Thessaloniki (Thessaloniki, Greece; approval no. 1.463; 19/10/2021). Written informed consent was obtained from patients or legal caregivers of all patients, as well as from patients aged >12 years.
Separation of bone marrow mononuclear cells (BMNCs)
BMNCs were separated using Histopaque®−1077 (MilliporeSigma; Merck KGaA), according to the manufacturer's instructions. Briefly, 1.5 ml bone marrow aspirate was diluted with PBS solution to a final volume of 3 ml and layered on top of 3 ml Histopaque-1077. The gradient was centrifuged at 400 × g for 30 min at room temperature, and the BMNCs were then collected. Once collected, the BMNCs were washed with PBS and stored at −80°C until use.
miRNA isolation
Total RNA was isolated from BMNCs using the miRNeasy Mini Kit with QIAzol Lysis reagent (cat. no. 217004; Qiagen GmbH), according to the manufacturer's protocol. As a quality control and to determine the efficiency of RNA extraction, three synthetic RNAs (spike-ins: UniSp2, UniSp4 and UniSp5) included in the RNA Spike-in Kit, For RT (cat. no. 339390; Qiagen GmbH) were added as recommended by the manufacturer. The quantity and quality (purity) of the isolated RNA was assessed spectrophotometrically, with measurements at wavelengths of 230, 260 and 280 nm.
Reverse transcription-quantitative (RT-q)PCR
Purified RNA was used for RT using the miRCURY LNA RT Kit (cat. no. 339340; Qiagen GmbH). During RT, a spike-in mix of two synthetic RNAs (UniSp6 and cel-miR-39-3p) was used as a quality control for complementary (c)DNA synthesis. The RT conditions were 60 min at 42°C, followed by 5 min at 95°C (inactivation step).
cDNA samples were then prepared using the miRCURY LNA SYBR® Green PCR Kit (cat. no. 339345; Qiagen GmbH). A Human Cancer Focus miRCURY LNA miRNA Focus PCR Panel (cat. no. 339325; Qiagen GmbH) was used to assess the RNA expression levels of 84 cancer-relevant human miRNAs. Each plate included lyophilized primer sets for 84 miRNAs and additionally contained primers for interplate calibrators, candidate reference genes, RNA spike-in controls and one water blank. qPCR was performed using a StepOnePlus™ Real-Time PCR System (Applied Biosystems™; Thermo Fisher Scientific, Inc.) with the following conditions: 95°C for 2 min, followed by 45 cycles at 95°C for 10 sec and 56°C for 1 min. Melting curve analysis was performed at the end of the PCR cycles. UniSp3 synthetic RNA was used as an interplate calibrator.
Data analysis
Raw Cq values from each PCR panel (Table SI) were uploaded to the GeneGlobe Data Analysis tool (Qiagen GmbH) for normalization, using let-7a-5p as a reference gene, as this miRNA was one of the most stably expressed candidates (Table SI). The relative quantity of each miRNA was calculated using the 2−ΔCq method (14) using let-7a-5p as the endogenous control. The fold change (FC) in miRNA expression between the two timepoints was calculated using the 2−ΔΔCq method and treated as a dichotomous variable (FC <1 corresponding to an increase in expression levels at the end of induction and FC >1 corresponding to a decrease).
Statistical analysis
The Mann-Whitney U test was used to evaluate differences in the expression levels of the miRNAs of interest at diagnosis between the patient groups defined by the following demographic and clinical characteristics: Age; sex; WBCs/µl; immunophenotype; hyperploidy; presence of the t(12;21)(p13;q22) translocation; prednisone response; risk group; and complete response at the end of induction (day 33) according to the definitions of the ALL IC BFM 2009 protocol. Spearman's rank correlation coefficient was used to evaluate the correlation between miRNA expression levels at diagnosis and MRD values on days 15 and 33. The Wilcoxon signed-rank test was used to assess differences between expression levels at diagnosis and day 33. Fisher's exact test was performed to assess possible associations between FC and the risk group, and between FC and complete response at the end of induction. SPSS software version 25 (IBM Corp.) was used for statistical analysis. P<0.05 was considered to indicate a statistically significant difference.
Bioinformatics analysis
The MicroRNA ENrichment TURned NETwork (15) web tool (release 3.4.4, March 2018) was used to identify experimentally proven targets of miRNAs of interest from miRTarBase release 9.0 beta (16), construct the interaction networks between miRNAs of interest and mRNAs, and identify the associated molecular pathways based on the Reactome database (17), version 85. The false discovery rate was set at ≤0.05 in all cases.
Results
Demographic and clinical characteristics of the patients
A total of 10 patients who fulfilled the inclusion criteria were included in the present study. The majority were female (6/10), aged 1–6 years (8/10) and without underlying conditions (8/10). One patient was diagnosed with congenital hearing impairment, neuropsychomotor developmental delay and epilepsy, and one patient with a ventricular septal defect. Upon diagnosis, 7/10 patients had <20,000 WBCs per µl [risk stratification cut-off (13)] and 8/10 were diagnosed with B-cell ALL (B-ALL). No patients exhibited extramedullary manifestations. The cytogenetic findings demonstrated that, 4/10 patients had hyperploidy and 5/10 had the translocation t(12;21)(p13;q22), which gives rise to the fusion gene ETV6-RUNX1 (3). None of the translocations t(1;19)(q23;p13), t(4;11)(q21;q23) and t(9;22)(q34;q11) were detected. Regarding response to treatment, good prednisone response with an absolute blast count of <1,000 in the peripheral blood on day 8 of the therapeutic protocol was observed in 8/10 patients. The mean MRD on days 15 and 33 was 7.1±15.3% (range, 0–50%) and 0.9±2.6% (range, 0–8.35%), respectively. A total of 2 patients were allocated to the standard-risk group, 5 to the intermediate-risk group and 3 to the high-risk group, as defined by the criteria of the ALL IC BFM 2009 protocol. A total of 8/10 patients achieved complete remission at the end of induction, based on the criteria of the ALL IC BFM 2009 protocol. The demographic and clinical characteristics of the patients are presented in Table I.
Association of miRNA levels at diagnosis with demographic and clinical characteristics of the patients
Among the evaluated miRNAs, the following results were demonstrated: The expression levels of nine miRNAs were significantly upregulated in patients aged 1–6 years compared with patients aged <1 year or >6 years; the expression levels of 26 miRNAs were significantly upregulated in male patients compared with female patients; the expression levels of three miRNAs were significantly upregulated in patients with <20,000/µl WBCs at diagnosis; the expression levels of three miRNAs were significantly upregulated in patients with B-ALL compared with T-cell ALL (T-ALL); and the expression levels of 13 miRNAs were significantly upregulated in patients with hyperploidy compared with those in patients without hyperploidy. No statistically significant differences between patients with and without t(12;21)(p13;q22) were observed. The miRNAs with significantly different expression levels between the aforementioned patient groups are presented in Table SII.
Association of miRNA levels at diagnosis with response to treatment
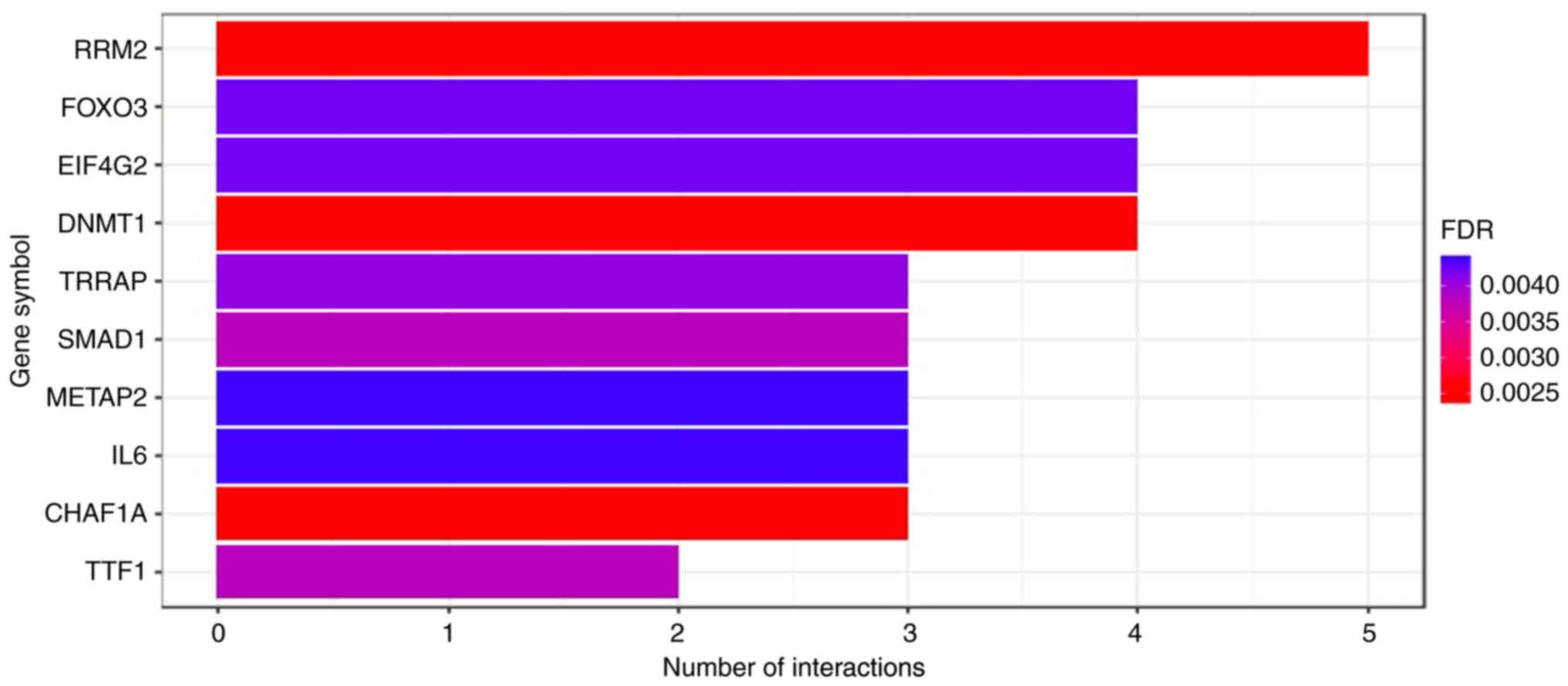
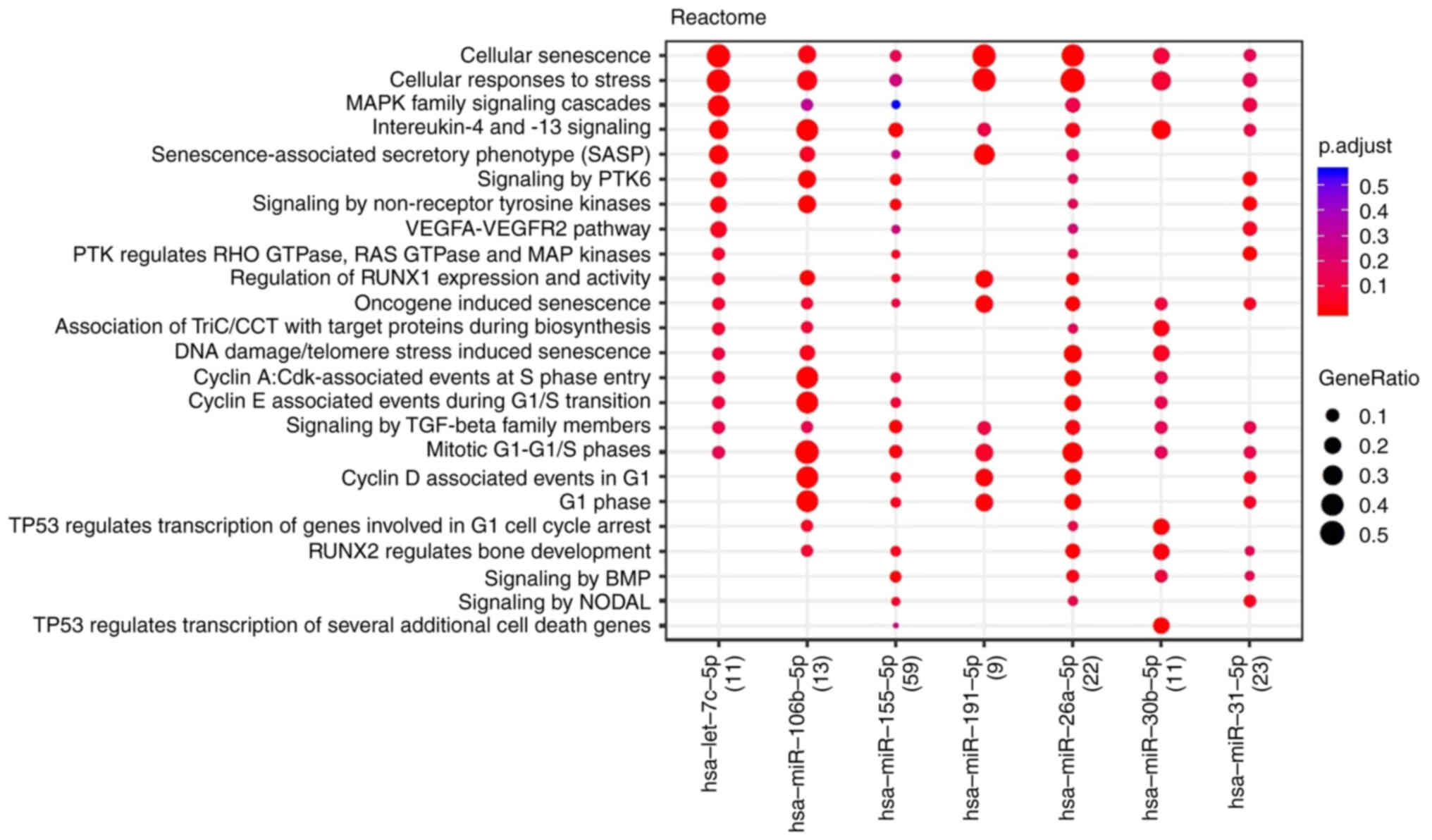
Patients with a good prednisone response exhibited markedly higher expression levels of seven miRNAs at diagnosis, namely let-7c-5p, miR-106b-5p, miR-26a-5p, miR-155-5p, miR-191-5p, miR-30b-5p and miR-31-5p, compared with those with poor prednisone response (Table II). The 10 most significant protein-coding genes targeted by the seven miRNAs, identified by miRTarBase, are presented in Fig. 1. The associated molecular pathways were identified using the Reactome database and are presented in Fig. 2. Cellular senescence, responses to stress and cell cycle regulation by cyclins appeared to be the key pathways involved.
Table II.miRNAs with expression levels at diagnosis that were significantly associated with at ≥2 parameters (demographic/clinical characteristics, laboratory findings and measures of response to treatment). |
Regarding other measures of response to treatment, a strong or moderate-to-strong negative correlation was observed between the expression levels of 18 (Table SIII) and 12 (Table SIII) miRNAs at diagnosis and MRD on days 15 and 33 of the therapeutic protocol, respectively. Conversely, a strong positive correlation was observed between the levels of miR-206 and MRD on day 33, based on the calculated Spearman's correlation coefficient.
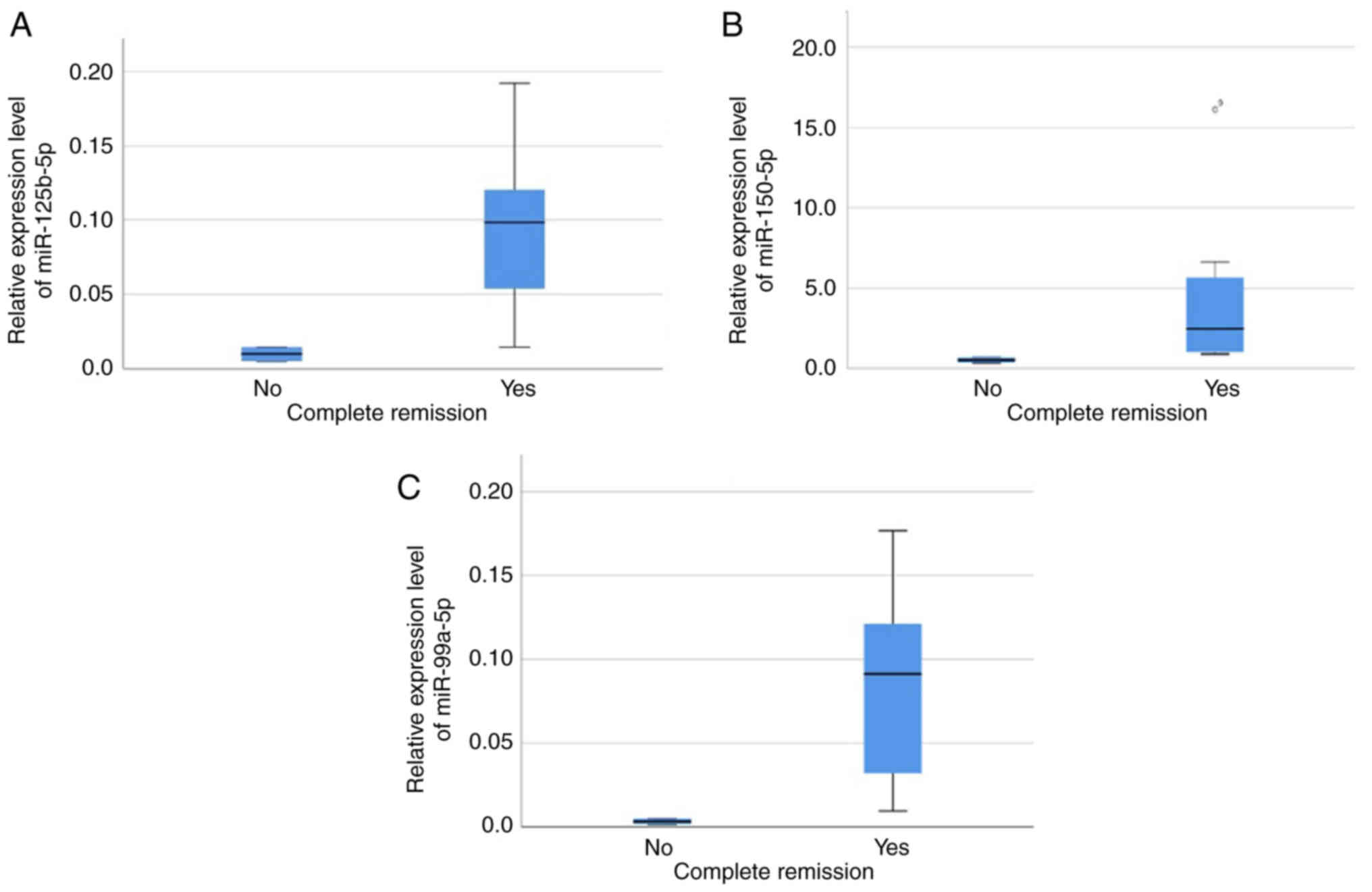
The expression levels of 14 miRNAs differed significantly between the risk groups (patients in the standard- or intermediate-risk groups vs. patients in the high-risk group; Table SIV). Mann-Whitney U test was performed in order to detect the miRNAs whose expression differed significantly between patients with and without complete remission at the end of induction (day 33). Higher expression levels of miR-125b-5p, miR-150-5p and miR-99a-5p were associated with a complete response at the end of induction (Mann-Whitney U P=0.044 for all 3 miRNAs; Table II), as shown in Fig. 3. The interaction networks of these three miRNAs and their targets (based on miRTarBase) are presented in Fig. 4 and the associated molecular pathways are shown in Fig. 5. TP53 and BH3 interacting domain death agonist associated signaling appeared to serve a central role in response to treatment.
miRNAs significantly associated with at least two parameters (demographic and clinical characteristics, laboratory findings and measures of response to treatment) and the respective P-values are summarized in Table II.
Effect of induction chemotherapy on the miRNA expression profile
The expression levels of seven miRNAs (miR-100-5p, miR-10b-5p, miR-143-3p, miR-145-5p, miR-182-5p, miR-10a-5p and miR-22-3p) were markedly upregulated at diagnosis, whilst those of eight miRNAs (miR-130a-3p, miR-146a-5p, miR-181a-5p, miR-181b-5p, miR-195-5p, miR-20b-5p, miR-210-3p and miR-222-3p) were markedly upregulated at the end of induction (day 33 of the therapeutic protocol) (Table SV).
The FC between diagnosis and day 33 (as a dichotomous variable, namely increase/decrease) differed significantly between risk groups for three miRNAs (Table SVI). A significant increase in expression levels of miR-206 was observed in all high-risk patients, compared with a significant decrease in 6/7 standard/intermediate-risk patients (P=0.033). Conversely, an increase in miR-210 levels was significantly associated with standard/intermediate-risk disease, as it was observed in all standard/intermediate-risk patients, compared with the significant decrease in miR-210 levels observed in 2/3 high-risk patients (P=0.047). An increase in miR-99a was also significantly associated with standard/intermediate-risk disease, as all standard/intermediate-risk patients had higher levels at the end of induction compared with diagnosis, whilst its expression levels were decreased in all high-risk patients (P=0.008).
Discussion
In the present study, differentially expressed miRNAs were identified among pediatric ALL patient groups with favorable and poor prognostic factors. The present study used a commercially available cancer panel which included 84 miRNAs that were tested in hematological malignancies or evaluated in solid tumors. This allowed for the detection of novel associations that have not been described previously, to the best of our knowledge. Furthermore, certain associations that have been described previously were further demonstrated in the present study.
Prednisone response was initially associated with event-free survival by the Berlin-Frankfurt-Munster Group in 1983 (18) and its importance regarding disease outcome has since been reported in a series of studies (19–21). In the current pilot study, good prednisone response was associated with increased expression levels of let-7c-5p, miR-106b-5p, miR-26a-5p, miR-155-5p, miR-191-5p, miR-30b-5p and miR-31-5p at diagnosis. Notably, 5/7 of this set of miRNAs target the mRNA of the gene encoding the ribonucleotide reductase regulatory subunit M2 (RRM2). RRM2 is an essential enzyme for DNA synthesis and cell homeostasis as it catalyzes the formation of deoxyribonucleotides from ribonucleotides, and imbalanced deoxyribonucleoside triphosphate pools hinder proper DNA replication and repair (22). RRM2 expression has been reported to be upregulated in cancer as may be expected due to the increased DNA synthesis in the rapidly proliferating neoplastic cells. It has also been used as a biomarker associated with poor prognosis in solid tumors (22,23). Thomas et al (24) first reported that administration of dexamethasone reduced RRM2 levels in multiple myeloma through glucocorticoid receptor binding within 100 kB of the transcription start site. Apart from its enzymatic function, RRM2 has been implicated in the regulation of cell death and its knockdown induces both autophagy and ferroptosis (25). Additionally, RRM2 is associated with immune escape through macrophage polarization and the programmed death protein 1/programmed death-ligand 1 signaling pathway (22). However, to the best of our knowledge, no studies have addressed the potential role of RRM2 in ALL. The present study provided a basis for the use of RRM2 and/or its pathway as a biomarker predictive of response, and as a therapeutic target in case of high expression levels. Regarding the other genes that serve as targets of more than two of the miRNAs associated with prednisone response, forkhead box O3 has previously been associated with poor prognosis and relapse in pediatric ALL (26). DNA methyltransferase 1 and transformation/transcription domain associated protein have been implicated in epigenetic dysregulation, a defining feature of ALL (27). Methionine aminopeptidase 2 is a metallopeptidase that catalyzes the removal of the N-terminal methionine from newly synthesized proteins, an essential step for their proper function, and has been implicated in the pathogenesis of numerous solid tumors (28). Chromatin assembly factor 1 subunit A (CHAF1A) mediates the assembly of histone octamers onto replicating DNA during the S-phase of the cell cycle and is required for normal hematopoiesis, as CHAF1A deletion results in failure of stem and progenitor cells to enter S-phase from G0/G1. Its overexpression is associated with leukemogenesis (29).
The expression levels of three miRNAs (miR-125b-5p, miR-99a-5p and miR-150-5p) were significantly upregulated at diagnosis in standard/intermediate-risk patients (P=0.017, P=0.033 and P=0.017, respectively), as well as in those who achieved a complete response on day 33 of induction (P=0.044 for all three miRNAs).
The expression levels of miR-125b were higher in patients with B-ALL, standard/intermediate-risk disease and a complete response on day 33, and were negatively correlated with MRD values on day 15 and 33. These findings are in-line with previous studies, which reported that low levels of miR-125b may be associated with a poor prognosis in pediatric ALL (30,31). Low levels of miR-125b have not only been associated with older age (>9 years), increased WBCs (>50.000/µl) and the high-risk group, but have also been reported to be an independent prognostic factor based on multivariate analysis (30). Increased miR-125b RNA expression levels have also been associated with the presence of the ETV6-RUNX1 fusion gene (10). In the present study, higher expression levels of miR-125b were observed in patients with the translocation t(12;21)(p13;q22) compared with those without; however, the observation did not reach statistical significance (P=0.22), possibly due to the small sample size. Nevertheless, both El-Khazragy et al (30) and Piatopoulou et al (31) previously reported an association of an increase in miR-125b levels post-chemotherapy with unfavorable clinicopathological prognostic features, poor survival and relapse. These findings are in accordance with the association of increased miR-125b levels with resistance to vincristine and daunorubicin (32), which are both included in the ALL IC BFM 2009 protocol (13). Regarding the underlying molecular mechanism, miR-125b serves an essential role in normal B-cell development and protection from carcinogenesis by targeting lin-28 homolog A (33). Furthermore, miR-125b regulates apoptosis by targeting the antiapoptotic gene BCL2 (30,34).
miR-99a RNA expression levels were significantly higher in patients with B-ALL, standard/intermediate-risk disease and complete response on day 33 and were significantly negatively correlated with MRD values on day 15 and 33. These findings are also in-line with previous studies. Li et al (35) reported that miR-99a was downregulated in high-risk patients and its expression levels were associated with survival. In vitro restoration of miR-100 and miR-99a expression has been reported to result in suppression of cell proliferation and to enhance the effect of dexamethasone regarding induction of apoptosis by targeting two important signaling pathways: i) FK506-binding protein 51, which along with heat shock proteins regulates the translocation of the glucocorticoid receptor from the cytoplasm to the nucleus; and ii) insulin like growth factor 1 receptor/mTOR, and subsequently the antiapoptotic MCL1 gene of the BCL2 family (35). Notably, in the present study, the expression levels of miR-99a were increased in all standard/intermediate-risk patients and decreased in all high-risk patients. The present results supported the previously reported observation that miR-99a acts as a tumor suppressor miRNA in pediatric B-ALL, compared with its activity as an oncomiR in acute myeloid leukemia (36). Furthermore, similar to miR-125b, miR-99a is part of the molecular signature of ETV6-RUNX1+ ALL and is also associated with resistance to vincristine and daunorubicin (9,37,38). In the present study, the levels of miR-99a were higher in the patient group with the translocation t(12;21)(p13;q22); however, this was not statistically significant (P=0.22), possibly due to the small sample size (data not shown).
The expression levels of miR-150 were higher in patients with B-ALL, standard/intermediate-risk disease and a complete response on day 33 of induction chemotherapy. In accordance with the present findings, previous studies have reported downregulation of miR-150 at diagnosis to be associated with unfavorable prognostic factors, namely age <1 year and >6 years, increased WBCs (>20,000/µl) and T-ALL, as well as with a greater risk of relapse (39,40). Fang et al (41) reported that miR-150 suppressed cell proliferation and induced apoptosis in ALL cell lines and had a synergistic effect with cytarabine administration, which is also an agent used in the ALL IC BFM 2009 protocol (13). miR-150 exerts its antileukemic activity by regulating key cellular processes, including transcription and cell metabolism, and its experimentally identified targets include eukaryotic translation initiation factor 4B, forkhead box O4, protein kinase C a and Tet methylcytosine dioxygenase 3 (41).
A total of three miRNAs, namely let-7c-5p, miR-106b-5p and miR-191-5p, were associated with four prognostic factors. let-7c-5p is known to be a part of the molecular signature of ETV6-RUNX1+ ALL (10). Naderi et al (42) reported that miR-106b was implicated in the pathogenesis of T-ALL by targeting cyclin D1, a key gene in the Notch signaling pathway. Furthermore, miR-106b has been reported to be upregulated in relapsed lysine methyltransferase 2A-rearranged acute myeloid leukemia in pediatric patients (43). However, to the best of our knowledge, there are no data regarding the role of miR-106b in pediatric ALL at present. A total of two studies have associated lower levels of miR-191-5p with relapse in ALL in the Chinese pediatric population (39,44).
Bioinformatics analysis revealed that all three miRNAs (miR-125b-5p, miR-99a-5p and miR-150-5p) that were associated with complete response at the end of induction, targeted the mRNA encoding MON1 homolog B (MON1B), which interferes with NF-κB signaling. Knockdown of MON1B has been demonstrated to increase the expression levels of of NF-κB inhibitor A and reduce the expression levels of p65 (45). Constitutively activated NF-κB complexes are found in the majority of childhood ALL cases, regardless of subtype (46). Regarding the molecular pathways associated with response to treatment, TP53 signaling seems to serve a key role. Unlike in solid tumors, the role of TP53 in ALL has only recently been reported. TP53 mutations are very rare in pediatric ALL, accounting for 2–4% of B-ALL cases at diagnosis and 12% at relapse, and they are associated with a poor prognosis (47). However, functional deregulation of TP53 has been observed in B-ALL due to variations in isoform expression (48). Furthermore, Nakagawa et al (49) recently reported that TP53 was implicated in the nucleolar stress response, through which 6-mercaptopurine, methotrexate, daunorubicin and cytarabine exert their antileukemic activity. Further studies are required to elucidate the role of miRNAs in TP53 deregulation in pediatric ALL and possible associations with clinicopathological features and prognosis.
In the present study, miR-210 levels exhibited changes pre- and post-therapy that markedly differed between risk groups. miR-210 is a well-known hypoxamir, the expression of which is induced by hypoxia inducible factor (HIF); it regulates key cellular processes, including mitochondrial metabolism, angiogenesis, DNA repair and cell survival (50,51). Increased levels of miR-210 have been observed in several solid tumors, serving at the same time as a biomarker associated with a poor prognosis (50). However, its role in ALL remains unclear with contradicting results in the few studies with clinical samples (39,52,53). In the present pilot study, there was no significant difference between risk groups at diagnosis, but a significant increase in expression levels was observed in all standard/intermediate-risk patients compared with a decrease in 2/3 high-risk patients (P=0.047) after chemotherapy administration. Contrary to its protective effect in hypoxia, increased expression of miR-210 in normoxia leads to the accumulation of reactive oxygen species and oxidative stress mainly due to repression of the iron-sulfur cluster scaffold proteins, ISCU1 and ISCU2. Furthermore, by targeting DNA repair protein RAD52, miR-210 inhibits homology-dependent DNA repair (50,51). This causes accumulation of DNA damage and suppression of cell proliferation via additional targeting of fibroblast growth factor receptor like 1, homeobox A3, homeobox A9 and E2F transcription factor 3 (50,51). As the extremely hypoxic state due to rapid uncontrolled proliferation of leukemic cells in the bone marrow at diagnosis is normalized with therapy administration, the mechanism may provide a plausible explanation of the present results. The proposed mechanism is presented in Fig. 6. Further studies are needed to elucidate the complex mechanisms of the hypoxia-induced epigenetic dysregulation in ALL and the effect of therapy administration, the HIF-independent actions of miR-210 and ultimately of its possible use as a biomarker for monitoring response to treatment in pediatric ALL.
Furthermore, in the present study, the expression levels of miR-206 were significantly increased in all high-risk patients, compared with their decrease in 6/7 standard/intermediate-risk patients (P=0.033) after chemotherapy administration. miR-206 was also significantly positively correlated with MRD on day 33 (r=0.724; P=0.018). The role of miR-206 has been extensively investigated in solid tumors, where it acts as a tumor suppressor miRNA in the majority of cases (54); however, there is a lack of data regarding its role in hematological malignancies. Existing evidence suggests that miR-206 is upregulated in pediatric patients with B-ALL compared with age-matched controls and that it inhibits cell proliferation by targeting neuroepithelial cell-transforming 1 (55). Although the mechanism behind the results of the present study is not yet clear, it can be hypothesized that miR-206 participates in pathways associated with cell proliferation. However, the potential for its use as a prognostic biomarker needs to be addressed by larger studies.
In conclusion, the present study identified miRNAs that were associated with established prognostic factors, including age, sex, WBCs at diagnosis, immunophenotype and cytogenetic findings. Furthermore, analysis revealed miRNA signatures associated with the prednisone response, risk group and complete response at the end of induction, as well as miRNAs, whose change with chemotherapy administration could be monitored to assess the response to treatment. These miRNAs could be added to the existing measures of evaluating response to treatment, namely, prednisone response and MRD, especially as RT-qPCR detection of molecular markers is more sensitive than flow cytometry, which is routinely used for MRD measurement (56). Moreover, the present findings provide the basis for further exploration of certain miRNA targets, whose role in pediatric ALL has not yet been investigated. However, the short follow-up time and the small sample size constitute the main limitations of the present study, thus necessitating the validation of these findings in larger patient cohorts to evaluate the extent to which these miRNAs could serve as independent prognostic factors and whether they could be successfully integrated into the current risk stratification systems. Furthermore, evaluation of the target genes at the mRNA and protein level could provide confirmation of the role of the miRNAs and elucidate the molecular mechanisms of treatment resistance.
Supplementary Material
Supporting Data
Supporting Data
Acknowledgements
Not applicable.
Funding
The present study was funded by Pfizer Hellas S.A. (grant no. 75239833).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Authors' contributions
ET, EH, AT and EG were responsible for conceptualization, EG and GT were responsible for the methodology, ET and EG were responsible for formal analysis, ET, CA, ML, EP and AGT performed the investigation, ML, EP, EH, AT, AGT and GT provided resources, ET, CA and EG were responsible for data curation, ET and CA prepared the original draft of the manuscript, EH, AT, EG, GT, EP, and AGT reviewed and edited the manuscript, ET was responsible for visualization of the study results, EH, AT, EG, AGT and GT supervised the project, EH, AT, EG, GT and AGT were responsible for administration and AT was responsible for funding acquisition. ET and EG confirm the authenticity of all the raw data. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
The present study was performed in accordance with the Declaration of Helsinki and approved by the Committee for Bioethics and Ethics of the School of Medicine of the Aristotle University of Thessaloniki (Thessaloniki, Greece; approval no. 1.463; 15/10/2021).
Written informed consent was obtained from parents or legal caregivers of all patients, as well as from patients aged >12 years.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
|
Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ and Cronin KA: SEER Cancer Statistics Review, 1975–2018. National Cancer Institute; Bethesda, MD: 2011 | |
|
Hunger SP, Lu X, Devidas M, Camitta BM, Gaynon PS, Winick NJ, Reaman GH and Carroll WL: Improved survival for children and adolescents with acute lymphoblastic leukemia between 1990 and 2005: A report from the children's oncology group. J Clin Oncol. 30:1663–1669. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Pui CH, Carroll WL, Meshinchi S and Arceci RJ: Biology, risk stratification, and therapy of pediatric acute leukemias: An update. J Clin Oncol. 29:551–565. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Eckert C, Parker C, Moorman AV, Irving JA, Kirschner-Schwabe R, Groeneveld-Krentz S, Révész T, Hoogerbrugge P, Hancock J, Sutton R, et al: Risk factors and outcomes in children with high-risk B-cell precursor and T-cell relapsed acute lymphoblastic leukaemia: Combined analysis of ALLR3 and ALL-REZ BFM 2002 clinical trials. Eur J Cancer. 151:175–189. 2021. View Article : Google Scholar : PubMed/NCBI | |
|
Pui CH, Mullighan CG, Evans WE and Relling MV: Pediatric acute lymphoblastic leukemia: Where are we going and how do we get there? Blood. 120:1165–1174. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Woo JS, Alberti MO and Tirado CA: Childhood B-acute lymphoblastic leukemia: A genetic update. Exp Hematol Oncol. 3:162014. View Article : Google Scholar : PubMed/NCBI | |
|
Esquela-Kerscher A and Slack FJ: Oncomirs-microRNAs with a role in cancer. Nat Rev Cancer. 6:259–269. 2006. View Article : Google Scholar : PubMed/NCBI | |
|
Montagner S, Dehó L and Monticelli S: MicroRNAs in hematopoietic development. BMC Immunol. 15:142014. View Article : Google Scholar : PubMed/NCBI | |
|
Carvalho de Oliveira J, Molinari Roberto G, Baroni M, Bezerra Salomão K, Alejandra Pezuk J and Sol Brassesco M: MiRNA dysregulation in childhood hematological cancer. Int J Mol Sci. 19:26882018. View Article : Google Scholar : PubMed/NCBI | |
|
Gutierrez-Camino A, Garcia-Obregon S, Lopez-Lopez E, Astigarraga I and Garcia-Orad A: MiRNA deregulation in childhood acute lymphoblastic leukemia: A systematic review. Epigenomics. 12:69–80. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Szczepanek J: Role of microRNA dysregulation in childhood acute leukemias: Diagnostics, monitoring and therapeutics: A comprehensive review. World J Clin Oncol. 11:348–369. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Durmaz B, Bagca BG, Cogulu O, Susluer SY, Alpay A, Aksoylar S and Gunduz C: Antileukemic Effects of Anti-miR-146a, Anti-miR-155, Anti-miR-181a, and prednisolone on childhood acute lymphoblastic leukemia. Biomed Res Int. 2021:32073282021. View Article : Google Scholar : PubMed/NCBI | |
|
Stary J, Zimmermann M, Campbell M, Castillo L, Dibar E, Donska S, Gonzalez A, Izraeli S, Janic D, Jazbec J, et al: Intensive chemotherapy for childhood acute lymphoblastic leukemia: Results of the randomized intercontinental trial ALL IC-BFM 2002. J Clin Oncol. 32:174–184. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Schmittgen TD and Livak KJ: Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc. 3:1101–1108. 2008. View Article : Google Scholar : PubMed/NCBI | |
|
Licursi V, Conte F, Fiscon G and Paci P: MIENTURNET: An interactive web tool for microRNA-target enrichment and network-based analysis. BMC Bioinformatics. 20:5452019. View Article : Google Scholar : PubMed/NCBI | |
|
Hsu SD, Lin FM, Wu WY, Liang C, Huang WC, Chan WL, Tsai WT, Chen GZ, Lee CJ, Chiu CM, et al: miRTarBase: A database curates experimentally validated microRNA-target interactions. Nucleic Acids Res. 39:(Database issue). D163–D169. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Gillespie M, Jassal B, Stephan R, Milacic M, Rothfels K, Senff-Ribeiro A, Griss J, Sevilla C, Matthews L, Gong C, et al: The reactome pathway knowledgebase 2022. Nucleic Acids Res. 50((D1)): D687–D692. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Riehm H, Reiter A, Schrappe M, Berthold F, Dopfer R, Gerein V, Ludwig R, Ritter J, Stollmann B and Henze G: Corticosteroid-dependent reduction of leukocyte count in blood as a prognostic factor in acute lymphoblastic leukemia in childhood (therapy study ALL-BFM 83). Klin Padiatr. 199:151–160. 1987.(In German). View Article : Google Scholar : PubMed/NCBI | |
|
Dördelmann M, Reiter A, Borkhardt A, Ludwig WD, Götz N, Viehmann S, Gadner H, Riehm H and Schrappe M: Prednisone response is the strongest predictor of treatment outcome in infant acute lymphoblastic leukemia. Blood. 94:1209–1217. 1999. View Article : Google Scholar : PubMed/NCBI | |
|
Schrappe M, Möricke A, Reiter A, Henze G, Welte K, Gadner H, Ludwig WD, Ritter J, Harbott J, Mann G, et al: Key treatment questions in childhood acute lymphoblastic leukemia: results in 5 consecutive trials performed by the ALL-BFM study group from 1981 to 2000. Klin Padiatr. 225 (Suppl):S62–S72. 2013. View Article : Google Scholar : PubMed/NCBI | |
|
Lauten M, Möricke A, Beier R, Zimmermann M, Stanulla M, Meissner B, Odenwald E, Attarbaschi A, Niemeyer C, Niggli F, et al: Prediction of outcome by early bone marrow response in childhood acute lymphoblastic leukemia treated in the ALL-BFM 95 trial: Differential effects in precursor B-cell and T-cell leukemia. Haematologica. 97:1048–1056. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Aye Y, Li M, Long MJ and Weiss RS: Ribonucleotide reductase and cancer: Biological mechanisms and targeted therapies. Oncogene. 34:2011–2021. 2015. View Article : Google Scholar : PubMed/NCBI | |
|
Su YF, Wu TF, Ko JL, Tsai HT, Tee YT, Chien MH, Chou CH, Lin WL, Low HY, Chou MY, et al: The expression of ribonucleotide reductase M2 in the carcinogenesis of uterine cervix and its relationship with clinicopathological characteristics and prognosis of cancer patients. PLoS One. 9:e916442014. View Article : Google Scholar : PubMed/NCBI | |
|
Thomas AL, Coarfa C, Qian J, Wilkerson JJ, Rajapakshe K, Krett NL, Gunaratne PH and Rosen ST: Identification of potential glucocorticoid receptor therapeutic targets in multiple myeloma. Nucl Recept Signal. 13:e0062015. View Article : Google Scholar : PubMed/NCBI | |
|
Zuo Z, Zhou Z, Chang Y, Liu Y, Shen Y, Li Q and Zhang L: Ribonucleotide reductase M2 (RRM2): Regulation, function and targeting strategy in human cancer. Genes Dis. 11:218–233. 2022. View Article : Google Scholar : PubMed/NCBI | |
|
Han BW, Feng DD, Li ZG, Luo XQ, Zhang H, Li XJ, Zhang XJ, Zheng LL, Zeng CW, Lin KY, et al: A set of miRNAs that involve in the pathways of drug resistance and leukemic stem-cell differentiation is associated with the risk of relapse and glucocorticoid response in childhood ALL. Hum Mol Genet. 20:4903–4915. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Yuan B, Zhang J, Wang H, Xiong L, Cai Q, Wang T, Jacobsen S, Pradhan S and Wang Y: 6-Thioguanine reactivates epigenetically silenced genes in acute lymphoblastic leukemia cells by facilitating proteasome-mediated degradation of DNMT1. Cancer Res. 71:1904–1911. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Selvakumar P, Lakshmikuttyamma A, Dimmock JR and Sharma RK: Methionine aminopeptidase 2 and cancer. Biochim Biophys Acta. 1765:148–154. 2006.PubMed/NCBI | |
|
Volk A, Liang K, Suraneni P, Li X, Zhao J, Bulic M, Marshall S, Pulakanti K, Malinge S, Taub J, et al: A CHAF1B-Dependent molecular switch in hematopoiesis and leukemia pathogenesis. Cancer Cell. 34:707–723.e7. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
El-Khazragy N, Elshimy AA, Hassan SS, Matbouly S, Safwat G, Zannoun M and Riad RA: Dysregulation of miR-125b predicts poor response to therapy in pediatric acute lymphoblastic leukemia. J Cell Biochem. 120:7428–7438. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Piatopoulou D, Avgeris M, Marmarinos A, Xagorari M, Baka M, Doganis D, Kossiva L, Scorilas A and Gourgiotis D: MiR-125b predicts childhood acute lymphoblastic leukaemia poor response to BFM chemotherapy treatment. Br J Cancer. 117:801–812. 2017. View Article : Google Scholar : PubMed/NCBI | |
|
Schotte D, Chau JCK, Sylvester G, Liu G, Chen C, van der Velden VH, Broekhuis MJ, Peters TC, Pieters R and den Boer ML: Identification of new microRNA genes and aberrant microRNA profiles in childhood acute lymphoblastic leukemia. Leukemia. 23:313–322. 2009. View Article : Google Scholar : PubMed/NCBI | |
|
Chaudhuri AA, So AY, Mehta A, Minisandram A, Sinha N, Jonsson VD, Rao DS, O'Connell RM and Baltimore D: Oncomir miR-125b regulates hematopoiesis by targeting the gene Lin28A. Proc Natl Acad Sci USA. 109:4233–4238. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Willimott S and Wagner SD: miR-125b and miR-155 contribute to BCL2 repression and proliferation in response to CD40 ligand (CD154) in human leukemic B-cells. J Biol Chem. 287:2608–2617. 2012. View Article : Google Scholar : PubMed/NCBI | |
|
Li XJ, Luo XQ, Han BW, Duan FT, Wei PP and Chen YQ: MicroRNA-100/99a, deregulated in acute lymphoblastic leukaemia, suppress proliferation and promote apoptosis by regulating the FKBP51 and IGF1R/mTOR signalling pathways. Br J Cancer. 109:2189–2198. 2013. View Article : Google Scholar : PubMed/NCBI | |
|
Zhang L, Li X, Ke Z, Huang L, Liang Y, Wu J, Zhang X, Chen Y, Zhang H and Luo X: MiR-99a may serve as a potential oncogene in pediatric myeloid leukemia. Cancer Cell Int. 13:1102013. View Article : Google Scholar : PubMed/NCBI | |
|
Schotte D, De Menezes RX, Akbari Moqadam F, Khankahdani LM, Lange-Turenhout E, Chen C, Pieters R and Den Boer ML: MicroRNA characterize genetic diversity and drug resistance in pediatric acute lymphoblastic leukemia. Haematologica. 96:703–711. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Akbari Moqadam F, Lange-Turenhout EA, Ariës IM, Pieters R and den Boer ML: MiR-125b, miR-100 and miR-99a co-regulate vincristine resistance in childhood acute lymphoblastic leukemia. Leuk Res. 37:1315–1321. 2013. View Article : Google Scholar : PubMed/NCBI | |
|
Zhang H, Luo XQ, Zhang P, Huang LB, Zheng YS, Wu J, Zhou H, Qu LH, Xu L and Chen YQ: MicroRNA patterns associated with clinical prognostic parameters and CNS relapse prediction in pediatric acute leukemia. PLoS One. 4:e78262009. View Article : Google Scholar : PubMed/NCBI | |
|
Avigad S, Verly IR, Lebel A, Kordi O, Shichrur K, Ohali A, Hameiri-Grossman M, Kaspers GJ, Cloos J, Fronkova E, et al: miR expression profiling at diagnosis predicts relapse in pediatric precursor B-cell acute lymphoblastic leukemia. Genes Chromosomes Cancer. 55:328–339. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Fang ZH, Wang SL, Zhao JT, Lin ZJ, Chen LY, Su R, Xie ST, Carter BZ and Xu B: miR-150 exerts antileukemia activity in vitro and in vivo through regulating genes in multiple pathways. Cell Death Dis. 7:e23712016. View Article : Google Scholar : PubMed/NCBI | |
|
Naderi T, Mohammadi-Yeganeh S, Mohammadi-Hezaveh N, Hadavi R, Gharehbaghian A, Vazifeh-Shiran N, Fallah Azad V and Paryan M: Investigating the inhibitory effect of miR-34a, miR-449a, miR-1827, and miR-106b on target genes including NOTCH1, c-Myc, and CCND1 in human T cell acute lymphoblastic leukemia clinical samples and cell line. Iran J Basic Med Sci. 23:376–382. 2020.PubMed/NCBI | |
|
Verboon LJ, Obulkasim A, De Rooij JD, Katsman-Kuipers JE, Sonneveld E, Baruchel A, Trka J, Reinhardt D, Pieters R, Cloos J, et al: MicroRNA-106b ~ 25 cluster is upregulated in relapsed MLL-rearranged pediatric acute myeloid leukemia. Oncotarget. 7:48412–48422. 2016. View Article : Google Scholar : PubMed/NCBI | |
|
Xu L, Liang YN, Luo XQ, Liu XD and Guo HX: Association of miRNAs expression profiles with prognosis and relapse in childhood acute lymphoblastic leukemia. Zhonghua Xue Ye Xue Za Zhi. 32:178–181. 2011.(In Chinese). PubMed/NCBI | |
|
Jiang L, Qian J, Yang Y and Fan Y: Knockdown of MON1B exerts anti-tumor effects in colon cancer in vitro. Med Sci Monit. 24:7710–7718. 2018. View Article : Google Scholar : PubMed/NCBI | |
|
Kordes U, Krappmann D, Heissmeyer V, Ludwig WD and Scheidereit C: Transcription factor NF-κB is constitutively activated in acute lymphoblastic leukemia cells. Leukemia. 14:399–402. 2000. View Article : Google Scholar : PubMed/NCBI | |
|
Ueno H, Yoshida K, Shiozawa Y, Nannya Y, Iijima-Yamashita Y, Kiyokawa N, Shiraishi Y, Chiba K, Tanaka H, Isobe T, et al: Landscape of driver mutations and their clinical impacts in pediatric B-cell precursor acute lymphoblastic leukemia. Blood Adv. 4:5165–5173. 2020. View Article : Google Scholar : PubMed/NCBI | |
|
Oh L, Hainaut P, Blanchet S and Ariffin H: Expression of p53 N-terminal isoforms in B-cell precursor acute lymphoblastic leukemia and its correlation with clinicopathological profiles. BMC Cancer. 20:1102020. View Article : Google Scholar : PubMed/NCBI | |
|
Nakagawa S, Kawahara K, Okamoto Y, Kodama Y, Nishikawa T, Kawano Y and Furukawa T: Association between dysfunction of the nucleolar stress response and multidrug resistance in pediatric acute lymphoblastic leukemia. Cancers (Basel). 14:51272022. View Article : Google Scholar : PubMed/NCBI | |
|
Devlin C, Greco S, Martelli F and Ivan M: miR-210: More than a silent player in hypoxia. IUBMB Life. 63:94–100. 2011. View Article : Google Scholar : PubMed/NCBI | |
|
Chan SY and Loscalzo J: MicroRNA-210: A unique and pleiotropic hypoxamir. Cell Cycle. 9:1072–1083. 2010. View Article : Google Scholar : PubMed/NCBI | |
|
Mei Y, Gao C, Wang K, Cui L, Li W, Zhao X, Liu F, Wu M, Deng G, Ding W, et al: Effect of microRNA-210 on prognosis and response to chemotherapeutic drugs in pediatric acute lymphoblastic leukemia. Cancer Sci. 105:463–472. 2014. View Article : Google Scholar : PubMed/NCBI | |
|
Mei Y, Li Z, Zhang Y, Zhang W, Hu H, Zhang P, Wu M and Huang D: Low miR-210 and CASP8AP2 expression is associated with a poor outcome in pediatric acute lymphoblastic leukemia. Oncol Lett. 14:8072–8077. 2017.PubMed/NCBI | |
|
Khalilian S, Hosseini Imani SZ and Ghafouri-Fard S: Emerging roles and mechanisms of miR-206 in human disorders: A comprehensive review. Cancer Cell Int. 22:4122022. View Article : Google Scholar : PubMed/NCBI | |
|
Sun H, Zhang Z, Luo W, Liu J, Lou Y and Xia S: NET1 enhances proliferation and chemoresistance in acute lymphoblastic leukemia cells. Oncol Res. 27:935–944. 2019. View Article : Google Scholar : PubMed/NCBI | |
|
Contreras Yametti GP, Ostrow TH, Jasinski S, Raetz EA, Carroll WL and Evensen NA: Minimal residual disease in acute lymphoblastic leukemia: Current practice and future directions. Cancers (Basel). 13:18472021. View Article : Google Scholar : PubMed/NCBI |