COVID‑19‑associated acute appendicitis in adults. A report of five cases and a review of the literature
- Authors:
- Published online on: June 1, 2022 https://doi.org/10.3892/etm.2022.11409
- Article Number: 482
-
Copyright: © Georgakopoulou et al. This is an open access article distributed under the terms of Creative Commons Attribution License.
Abstract
Introduction
With ~429 million confirmed cases of infection by the end of February, 2022, the novel coronavirus, which causes coronavirus disease 2019 (COVID-19), has negatively affected patients and healthcare systems worldwide (1). Patients with COVID-19 present with a wide spectrum of respiratory symptoms, ranging from mild flu-like symptoms to severe and potentially life-threatening pneumonia (2). Furthermore, some patients report gastrointestinal symptoms, such as nausea, vomiting, diarrhea and abdominal pain in addition to the aforementioned respiratory symptoms or, in rare cases, as a distinct presentation of illness (3).
In several studies, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) RNA has been found in stool samples from infected individuals, and its viral receptor, angiotensin-converting enzyme 2 (ACE2), is known to be overexpressed all across the length of the gut mucosa, with an increased expression in the small bowel and colon (3). These data suggest that SARS-CoV-2 can infect and multiply effectively in the gastrointestinal system, which may have consequences for disease treatment, transmission and infection control (4).
Even though abdominal pain syndrome suggests acute appendicitis, it is crucial to consider SARS-CoV-2 infection as a potential diagnosis during this pandemic era. Prior to emergency surgery, screening for a co-infection may change the patient circuit and force a re-evaluation of the therapeutic strategy. In rare situations, it may even lead to a differential diagnosis that requires a markedly different medical therapy rather than surgery (5). However, there have been reports of a few cases of acute appendicitis associated with SARS-CoV-2 infection (6). Due to the high infectivity and potential for extensive lung damage, healthcare professionals have to react quickly to treat individuals who have been diagnosed with COVID-19, while they are concurrently suffering from other diseases, such as acute appendicitis (7).
The gold standard of treatment for acute appendicitis is appendectomy. Ηowever, research has indicated that conservative care with intravenous antibiotics can result in equivalent results and can be used as a substitute in some individuals (8). Appendectomy in patients with acute appendicitis who suffer from COVID-19 is challenging, since it entails significant surgical risks for the patients, as well as dangers for healthcare workers who are exposed to SARS-CoV-2. While medical treatment decreases the morbidity and mortality associated with surgery, it comes with a high possibility of treatment failures, which can lead to perforation, peritonitis and even death (9).
The present study describes five cases of adult patients with COVID-19 with simultaneous acute appendicitis in an aim to provide further insight into the diagnosis and management of adult patients with COVID-19 with acute appendicitis.
Case report
Case 1
A 19-year-old male, with no significant previous medical history, presented to the emergency department (ED) of Laiko General Hospital (Athens, Greece) with complaints of acute epigastric pain, nausea and multiple episodes of non-projectile, non-bilious vomiting and diarrhea 12 h prior. The pain was sharp, with radiation to his right lower abdominal quadrant (RLAQ) and was aggravated by movement. He reported no fever or respiratory symptoms, such as sore throat, dyspnea and cough.
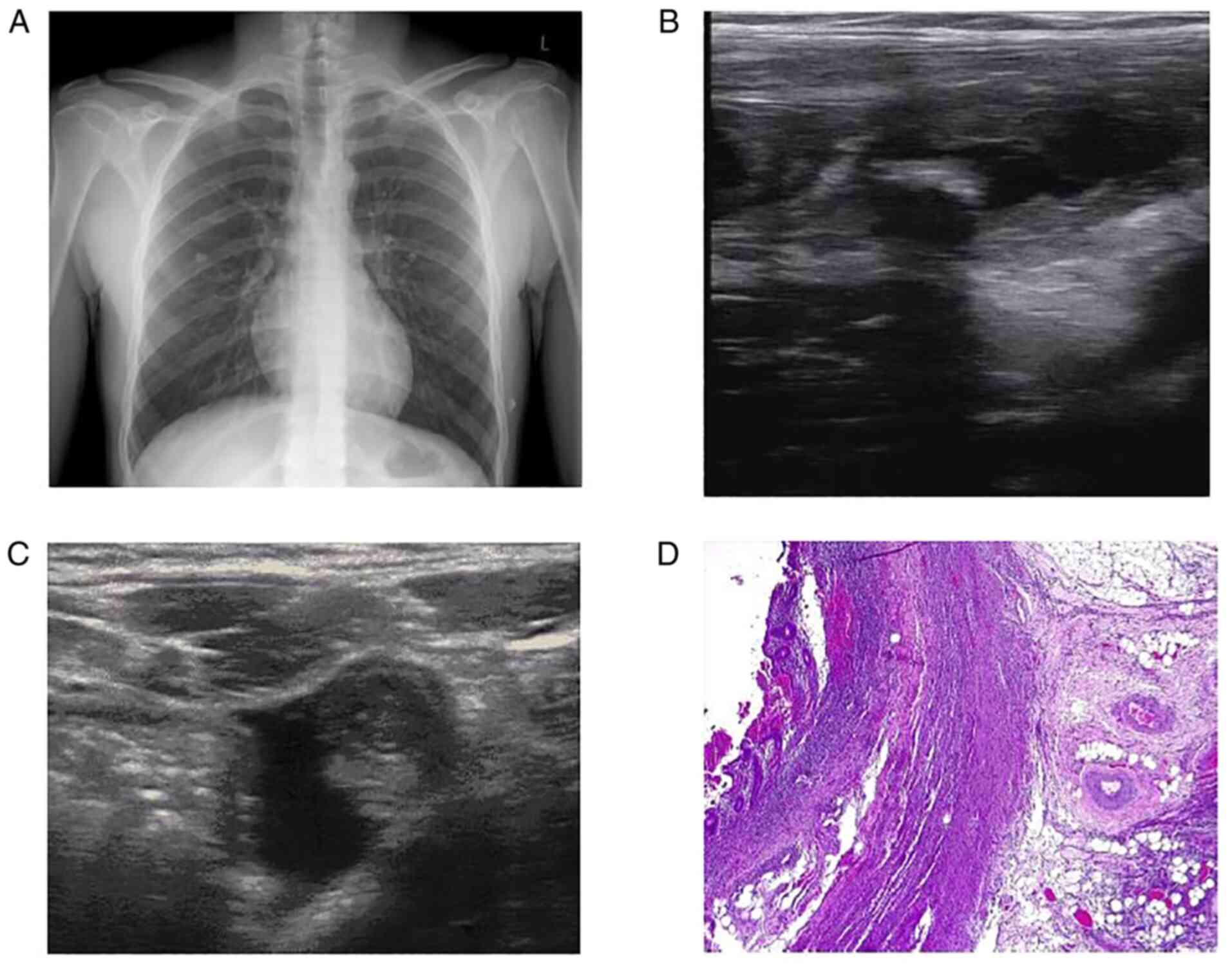
Upon an examination, the patient appeared to be fatigued; however, he had normal vital signs. An abdominal examination revealed superficial and deep tenderness on the RLAQ with guarding and rebound tenderness. Laboratory investigations revealed an increased leukocyte count (16.11 k/µl; reference range, 4.5-11 k/µl) with neutrophilia (88.8%; reference range, 40-74%) and lymphopenia (0.9 k/µl; reference range, 1.2-3.4 k/µl), elevated C-reactive protein (CRP) levels (6.69 mg/l; reference range, 0-5 mg/l), elevated total bilirubin levels (1.27 mg/dl; reference range, 0.3-1.2 mg/dl), elevated creatine kinase (CK) levels (231 U/l; reference range, 38-190 U/l) and elevated ferritin levels (452 ng/ml; reference range, 30-400 ng/ml). Pancreatic enzyme, urine analysis, liver enzyme and renal function test results were within the normal range. In addition, his chest X-ray was normal (Fig. 1A).
The patient underwent abdominal and pelvic ultrasonography (U/S), which revealed a hyperechoic shadowing lesion consistent with an appendicolith (Fig. 1B) and a dilated appendix, that was measured up to 0.8 cm in the transverse dimension with surrounding fluid (Fig. 1C). The Alvarado total score was 8 out of 10 based on the symptoms and laboratory tests that supported the diagnosis of acute appendicitis. A reverse transcription-PCR (RT-PCR) test for COVID-19 was conducted as per the hospital's protocol surgery, the result of which was positive. With all COVID-19 precautions taken, an open appendectomy was conducted under general anesthesia. The histopathological examination of the appendicular tissue revealed acute appendicitis with massive inflammatory infiltrate of the appendicular wall and mesenterium (Fig. 1D).
The patient received intravenous antibiotic therapy with cefoxitine at 1 g three times daily and metronidazole at 500 mg three times daily. His clinical condition gradually improved. A post-operative follow-up was uneventful and the patient was transferred to the COVID-19 unit of the hospital for further management. The patient had a good evolution. He never presented symptoms indicative of respiratory involvement, nor did he receive any specific therapy for COVID-19.
Case 2
A 62-year-old male patient with a previous medical history of cholecystectomy presented to the ED of Laiko General Hospital with complaints of fever, diffuse abdominal pain and nausea 2 days prior. The pain had migrated to the RLAQ. The patient had close contact with a patient with COVID-19 4 days prior; however, he reported no respiratory symptoms.
Upon an examination, the patient was found to be febrile, but the other vital signs were normal. The chest examination was unremarkable. An abdominal examination revealed superficial and deep tenderness on the RLAQ with guarding and rebound tenderness. Laboratory investigations revealed a normal leukocyte count (10.87 k/µl; reference range, 4.5-11 k/µl) with neutrophilia (87%; reference range, 40-74%) and lymphopenia (0.840 k/µl; reference range, 1.2-3.4 k/µl), significantly elevated CRP levels (229.75 mg/l; reference range, 0-5 mg/l), elevated alanine aminotranferase (ALT) levels (70 U/l; reference range, <41 U/l) and aspartate aminotransferase (AST) levels (55 U/l; reference, 15-40 U/l), increased gamma-glutamyl transferase (GGT) levels (349 U/l; reference range, 8-61 U/l), elevated CK levels (225 U/l; reference range, 38-190 U/l) and elevated ferritin levels (1,200 ng/ml; reference range, 30-400 ng/ml). Pancreatic enzyme, urine analysis and renal function test results were within the normal range. An arterial blood gases analysis revealed a partial pressure of oxygen (pO2) of 81 mmHg, a partial pressure of carbon dioxide (pCO2) of 34 mmHg, pH 7.50 and HCO3 26.5 mmol/l in room air.
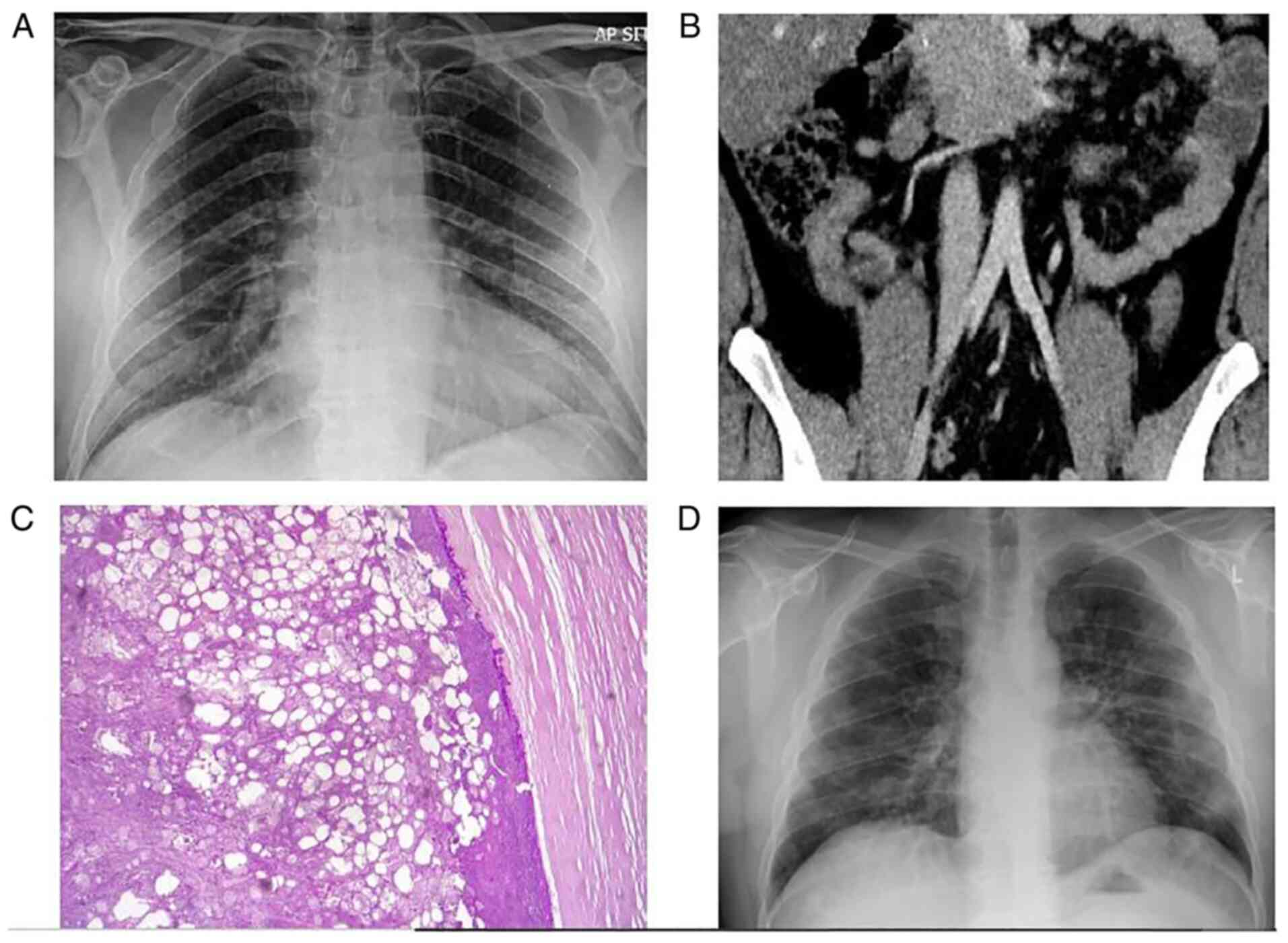
A chest X-ray was performed, which revealed mild infiltrates in both lower lung lobes (Fig. 2A). The Alvarado total score was 9 out of 10 based on the symptoms and laboratory tests that supported the diagnosis of acute appendicitis. The patient underwent an abdominal computed tomography (CT) scan, which revealed the mild dilation of the appendix and wall thickening (Fig. 2B). An RT-PCR test for COVID-19 was conducted and the result was positive. With all COVID-19 precautions taken, an open appendectomy was conducted under general anesthesia. The histopathological examination of the appendicular tissue revealed acute appendicitis with peri-appendicitis (Fig. 2C).
The patient received intravenous antibiotic therapy with cefoxitine at 1 g three times daily and metronidazole at 500 mg three times daily. His clinical condition gradually improved. The post-operative follow-up was uneventful and the patient was transferred to the COVID-19 unit for further management. On the third post-operative day, the patient presented with dyspnea and respiratory deterioration with an oxygen saturation of 92% in room air. A new arterial bloοd gas analysis revealed a pO2 of 61 mmHg, a pCO2 of 33 mmHg, pH 7.49 and HCO3 25.1 mmol/l in room air. A new chest radiograph revealed worsening infiltrates (Fig. 2D). The patient received therapy with intravenous dexamethasone at 6 mg once daily and remdesivir at 200 mg on the first day, followed by 100 mg daily for the following 4 days. He also received oxygen therapy with a nasal cannula delivering oxygen at a rate of 3 l/min. His clinical condition and oxygen levels gradually improved. No other complications occurred, and the patient was discharged following a 9-day hospitalization.
Case 3
A 51-year-old female patient presented to the ED of Laiko General Hospital with complaints of diffuse abdominal pain for 8 h prior to admission. The pain had migrated to the RLAQ. The patient had experienced a mild COVID-19 infection, with fever and a sore throat, 15 days prior to her presentation at the hospital. Upon the visit to the ED, she did not report fever, respiratory or other gastrointestinal symptoms. She had a previous medical history of hypothyroidism and partial nephrectomy of the left kidney due to renal cancer. Her current medications included levothyroxine at 100 µg daily.
Upon an examination, the patient was afebrile and all her vital signs were normal. Chest examination was unremarkable. Abdominal examination revealed superficial and deep tenderness on the RLAQ with guarding and rebound tenderness. Laboratory investigations revealed an increased leukocyte count (14.86 k/µl; reference range, 4.5-11 k/µl) with an elevated neutrophil count (9.881 k/µl; reference range, 1.5-6.6 k/µl) and a normal lymphocyte count (28.5%; reference range, 19-48%), elevated CRP levels (53.48 mg/l; reference range, 0-5 mg/,), elevated total bilirubin levels (2.45 mg/dl; reference range, 0.3-1.2 mg/dl), elevated ALT levels (60 U/l; reference range, <33 U/l) and AST levels (70 U/l; reference range, 11-35 U/l), increased GGT levels (363 U/l; reference range, 5-36 U/l), elevated CK levels (178 U/l; reference range, 26-167 U/l) and elevated ferritin levels (678 ng/ml; reference range, 30-400 ng/ml). Pancreatic enzyme, urine analysis, and renal function test results were within the normal range.
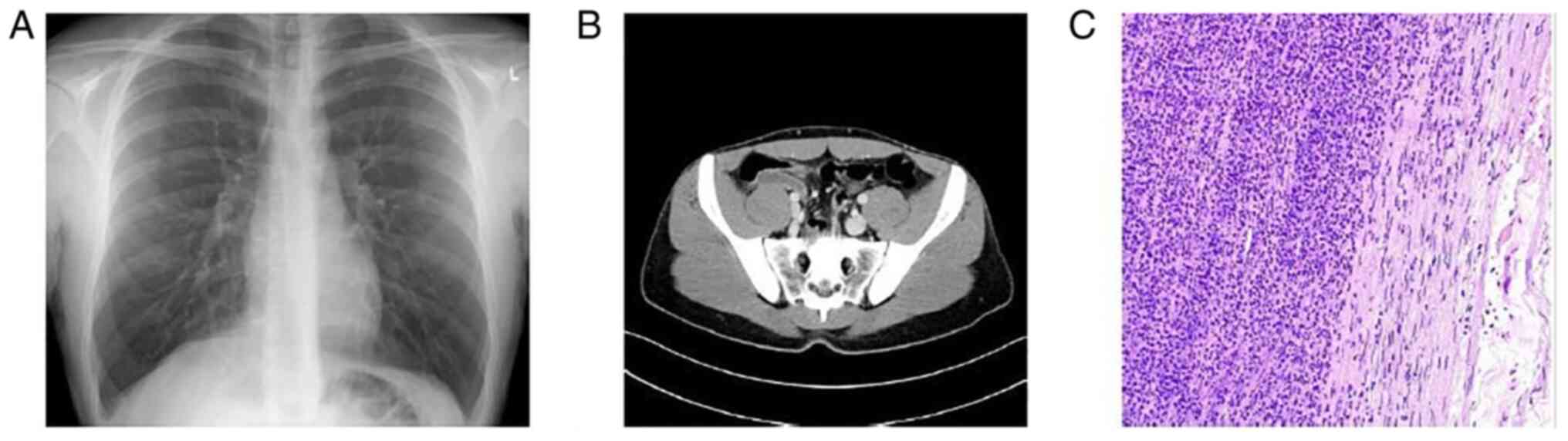
A chest X-ray was performed, which was normal (Fig. 3A). The Alvarado total score was 6 out of 10 based on the symptoms and laboratory tests. The patient had possible appendicitis according to the Alvarado score. The patient underwent an abdominal CT scan, which revealed an enlarged appendix, with marked wall thickening and stranding of the surrounding fat (Fig. 3B). RT-PCR analysis for COVID-19 was conducted and the result was positive. With all COVID-19 precautions taken, a laparoscopic appendectomy was conducted under general anesthesia. The histopathological examination of appendicular tissue revealed acute appendicitis with heavily inflamed mucosa, with accompanying extensive ulceration and hemorrhage (Fig. 3C).
The patient received intravenous antibiotic therapy with cefoxitine at 1 g three times daily and metronidazole at 500 mg three times daily. Her clinical condition gradually improved. The post-operative follow-up was uneventful and the patient was transferred to the COVID-19 unit for further management. No other complications occurred, and the patient was discharged following a 3-day hospitalization.
Case 4
A 23-year-old male patient with an insignificant previous medical history presented to the ED of Laiko General Hospital with complaints of diffuse abdominal pain for 12 h prior to admission. The pain had migrated to the RLAQ. The patient had close contact with a patient infected with COVID-19 3 days prior. Ηe did not report fever, respiratory or other gastrointestinal symptoms.
Upon an examination, the patient was afebrile and all his vital signs were normal. The chest examination was unremarkable. An abdominal examination revealed superficial and deep tenderness on the RLAQ with guarding and rebound tenderness. Laboratory investigations revealed an increased leukocyte count (13.17 k/µl; reference range, 4.5-11 k/µl) with neutrophilia (84.9%; reference range, 40-74%) and lymphopenia (1.17 k/µj; reference range, 1.2-3.4 k/µl), elevated CRP levels (6.23 mg/l; reference range, 0-5 mg/l) and elevated ferritin levels (434 ng/ml; reference range, 30-400 ng/ml). Pancreatic enzyme, liver enzyme, urine analysis and renal function test results were within the normal range.
A chest X-ray was performed, which was normal (Fig. 4A). The Alvarado total score was 7 out of 10 based on the symptoms and laboratory tests. The patient had probable appendicitis according to the Alvarado score. He underwent an abdominal CT scan, which revealed an inflamed appendix originating from the cecum in deep pelvic position (Fig. 4B). An RT-PCR test for COVID-19 was conducted and the result was positive. With all COVID-19 precautions taken, an open appendectomy was conducted under general anesthesia. The histopathological examination of appendicular tissue revealed acute appendicitis with intense neutropilic infiltration of the appendix wall (Fig. 4C).
The patient received intravenous antibiotic therapy with cefoxitine at 1 g three times daily and metronidazole at 500 mg three times daily. His clinical condition gradually improved. The post-operative follow-up was uneventful and the patient was transferred to the COVID-19 unit for further management. No other complications occurred, and the patient was discharged following a 4-day hospitalization. He never presented with any symptoms indicative of respiratory involvement, nor did he receive any specific therapy for COVID-19.
Case 5
A 60-year-old male patient presented to the ED of Laiko General Hospital with complaints of fever and diffuse abdominal pain for 3 days prior to admission. The pain had migrated to the RLAQ. He did not report any respiratory or other gastrointestinal symptoms. He had a previous medical history of diabetes mellitus type 2, arterial hypertension, hyperlipidemia, depression and cholecystectomy. His current medications included metformin at 500 mg twice daily, ramipril at 2.5 mg once daily, pitavastatin at 1 mg once daily and escitalopram at 10 mg once daily.
Upon an examination, the patient was febrile, but all the other vital signs were normal. The chest examination was unremarkable. An abdominal examination revealed superficial and deep tenderness on the RLAQ with guarding and rebound tenderness. Laboratory investigations revealed an increased leukocyte count (12.02 k/µl; reference range, 4.5-11 k/µl) with neutrophilia (85.9%; reference range, 40-74%) and lymphopenia (1.009 k/µl; reference range, 1.2-3.4 k/µl), elevated CRP levels (147.13 mg/l; reference range, 0-5 mg/l), elevated CK levels (316 U/l; reference range, 38-190 U/l) and elevated ferritin levels (850 ng/ml; reference range, 30-400 ng/ml). Pancreatic enzyme, liver enzyme, urine analysis and renal function test results were within the normal range.
A chest X-ray was performed, which was normal (Fig. 5A). The Alvarado total score was 8 out of 10 based on the symptoms and laboratory tests. The patient had probable appendicitis according to the Alvarado score. The patient underwent an abdominal CT scan, which revealed an appendiceal enlargement with intraluminal calcified fecalith and marked inflammatory changes in the surrounding mesenteric fat with possible microperforation (Fig. 5B). An RT-PCR test for COVID-19 was conducted and the result was positive. With all COVID-19 precautions taken, a laparoscopic appendectomy was conducted under general anesthesia. The histopathological examination of appendicular tissue revealed acute gangrenous appendicitis (Fig. 5C).
The patient received intravenous antibiotic therapy with cefoxitine at 1 g three times daily and metronidazole at 500 mg three times daily. His clinical condition gradually improved. The post-operative follow-up was uneventful and the patient was transferred to the COVID-19 unit for further management. No other complications occurred, and the patient was discharged following a 5-day hospitalization. He never presented with any symptoms indicative of respiratory involvement, and he did not receive any specific therapy for COVID-19.
Histopathological analysis
The tissue specimens from the patients were formalin-fixed and paraffin-embedded, as to standard histopathology laboratory routine (FFPE). The fixative used was 10% formalin solution, neutral buffered, 10%, for 24 h at room temperature. The thickness of the sections used was 4 µm. Histochemical staining with hematoxylin and eosin (supplied by Dako; Agilent Technologies, Inc.) was performed by using a DAKO Coverstainer for approximately 1 h and 15 min at room temperature. Finally, microscopic evaluation was carried out using a light microscope (Olympus BX51; Olympus Corporation).
Discussion
Patient characteristics and clinical presentation
COVID-19-associated acute appendicitis occurs in young adults, middle-aged individuals and the elderly. It can affect both males and females. Almost all the patients described herein presented with abdominal pain and complaints of various other typical symptoms, such as nausea and vomiting. As regards respiratory systems, some patients did not present with any respiratory symptoms, whereas others had more severe symptoms and suffered from COVID-19-related pneumonia. The diagnosis of acute appendicitis may precede the diagnosis of SARS-CoV-2 infection, may follow the diagnosis of SARS-CoV-2 infection or may be simultaneous to the diagnosis of SARS-CoV-2 infection (6,10-17). COVID-19-associated acute appendicitis has also been reported during pregnancy (17).
Diagnostic workup
The diagnosis of SARS-CoV-2 infection in the patients reported herein was confirmed by sending nasopharyngeal samples for the RT-PCR analysis of COVID-19 (6,10,11,13-17). In a previous study, SARS-CoV-2 infection was established by a positive RT-PCR test of an appendicular tissue sample (12). Laboratory test results have revealed increased white blood cell counts in the majority of cases (6,11,14,16), while lymphopenia, a hallmark of COVID-19 infection (18), has been observed in some cases (6,15,17), including the cases described in the present study. The diagnosis of COVID-19-associated acute appendicitis is established either by an abdominal U/S (6) or by an abdominal CT scan (10-16). In a previous study reporting a case of a pregnant woman, abdominal magnetic resonance imaging was performed to confirm the diagnosis (17). In all cases, resected appendicular tissues were sent for a histological examination, which revealed acute appendicitis (6,11-17).
Management of acute appendicitis
The majority of the cases in the present study were managed with appendectomy, either open or laparoscopic (6,11-17). Conservative successful treatment only with intravenous antibiotics has also been described in one case (10).
Outcomes
All patients with COVID-19-associated acute appendicitis reported in the literature have had an uneventful post-operative follow-up and favorable outcomes, even in cases of perforation (11,16-17) and sepsis (12). The cases of COVID-19-associated acute appendicitis found in the literature are summarized in Table I.
Pathogenetic mechanisms
Due to high expression of the viral receptor, ACE2, in the gut wall, SARS-CoV-2 may infect the intestinal wall, compromising barrier function and facilitating microbial translocation (19). The discovery of the atypical histological appearance of appendicular tissue, particularly infrequent microthrombi, the fibrinoid necrosis of blood vessels and perivascular lymphocytic inflammatory infiltration, which are indicative of SARS-CoV-2 infection, support the association between SARS-CoV-2 infection and acute appendicitis (12). Lymphocytic infiltration and fibrinous microthrombi are notable characteristics in various reports of lung specimens in patients with COVID-19(20).
Another feature supporting the association between SARS-CoV-2 infection and acute appendicitis is the laboratory findings of lymphopenia, and elevated ferritin and increased CK levels, that have been reported in COVID-19(21). The transmission route to the appendix is unknown. The presence of SARS-CoV-2 RNA in stool samples from individuals with gastrointestinal symptoms suggests that fecal-oral transmission may be a possibility. Oropharyngeal contamination can potentially bring infection into the gastrointestinal tract, allowing for bacterial translocation and appendicitis (22). Moreover, it has been reported that viral infections can cause acute appendicitis via several mechanisms, including lymphoid hyperplasia, which induces appendix blockage, and mucosal ulcerations, leading to subsequent bacterial infection (23).
Safety and management concerns
During the COVID-19 pandemic, it has been reported that the abdominal CT scan has an efficacy of 87.5% in diagnosing acute appendicitis, compared to 69.8% before the pandemic (24). An abdominal CT scan is widely used for diagnosis during the pandemic, and the rate of uncomplicated appendicitis has increased from 54.05 to 69.64%. This may help to lower the risk of viral transmission during surgery in patients with COVID-19 and symptoms consistent with acute appendicitis (25). An abdominal CT scan should be used as a tool for early and accurate diagnosis and treatment, since the prevalence of delayed diagnosis and complicated appendicitis has increased during the pandemic, and may prevent unnecessary operations.
There is no available evidence to indicate that COVID-19 is transmitted by surgical smoke (26,27). However, it has been reported that as the novel coronavirus has a structure that is comparable to viruses that have been reported to be transmitted by surgical smoke, such as Corynebacterium, human papillomavirus, poliovirus, human immunodeficiency virus and hepatitis B virus, there is a potential danger of viral transmission. When operating on COVID-19-infected patients, it is thus suggested to perform laparoscopic surgery rather than open surgery using a negative pressure operating room set-up, patient mobility and operation theater equipment (28).
In patients infected with COVID-19, post-operative consequences need to be considered. It has been demonstrated that the 30-day post-operative mortality rate of emergency surgery was greater than that of elective surgery for patients infected with COVID-19 prior to surgery. Furthermore, the mortality rate for patients with pulmonary complications has been shown to be 39.6% greater than the rate for patients without respiratory complications, which was 4.6% (29). To date, to the best of our knowledge, there are no large studies available in patients with COVID-19 suffering from acute appendicitis to estimate the mortality rate and the rate of complications in these patients compared to those with acute appendicitis without COVID-19.
Furthermore, therapy with steroids, which is administered in cases of severe COVID-19 infection, inhibits collagen production and wound maturation, and also interferes with the normal wound healing process (30). As a result, it is important to take into account the likelihood of incomplete wound healing in steroid-treated individuals. When a patient is on ventilator support, the risk of wound complications is also increased (31). Post-operative pneumonia, reintubation and inability to wean are all risk factors for wound dehiscence (32). As a result, risk factors for wound complications in patients with COVID-19 need to be considered.
In conclusion, since SARS-CoV-2 infection and acute appendicitis share symptoms including fever, anorexia, nausea, vomiting and even severe abdominal pain, the clinical diagnosis for the surgical abdomen in patients with COVID-19 is of limited effectiveness. SARS-CoV-2 may possibly be one of the causes of acute abdominal cases, such as acute appendicitis. Signs and symptoms are typically non-specific, and they may hide life-threatening conditions. Although gastrointestinal symptoms are less common in COVID-19, this infection cannot be ruled out and should be explored in every case. In patients with SARS-CoV-2 infection, a high index of suspicion for surgical issues is necessary. Furthermore, postponing surgical abdomen treatment may result in major complications and an increased risk of mortality. On the contrary, in patients with COVID-19, unnecessary surgery leads to iatrogenic morbidity and mortality, an increased demand on healthcare resources and an increased risk for healthcare professionals working in operative areas. Therefore, a surveillance system and defined rules are required for handling suspected COVID-19 cases that require immediate surgery to prevent the spread of the virus.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
VEG, CD and PP conceptualized the study. PS, SA, AA and GS obtained the medical images and prepared the table. VEG, SM, AP, AG and SC advised on patient care and medical treatment, and wrote and prepared the draft of the manuscript. NT and DAS analyzed the data and provided critical revisions. PS, SA and AA prepared the figures. VEG and SM confirm the authenticity of all the raw data. All authors contributed to manuscript revision and have read and approved the final version of the manuscript.
Ethics approval and consent to participate
Written informed consent was obtained from the patients described in the present case report.
Patient consent for publication
Written informed consent was obtained from the patients for the publication of the present case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Competing interests
DAS is the Editor-in-Chief for the journal, but had no personal involvement in the reviewing process, or any influence in terms of adjudicating on the final decision, for this article. The other authors declare that they have no competing interests.
References
|
Mishra A, Basumallick S, Lu A, Chiu H, Shah MA, Shukla Y and Tiwari A: The healthier healthcare management models for COVID-19. J Infect Public Health. 14:927–937. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, et al: Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 382:1708–1720. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Caio G, Lungaro L, Cultrera R, De Giorgio R and Volta U: Coronaviruses and gastrointestinal symptoms: An old liaison for the new SARS-CoV-2. Gastroenterol Hepatol Bed Bench. 13:341–350. 2020.PubMed/NCBI | |
|
Sultan S, Altayar O, Siddique SM, Davitkov P, Feuerstein JD, Lim JK, Falck-Ytter Y and El-Serag HB: AGA Institute. Electronic address: simpleewilson@gastro.org. AGA institute rapid review of the gastrointestinal and liver manifestations of COVID-19, meta-analysis of international data, and recommendations for the consultative management of patients with COVID-19. Gastroenterology. 159:320–334.e27. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Pautrat K and Chergui N: SARS-CoV-2 infection may result in appendicular syndrome: Chest CT scan before appendectomy. J Visc Surg. 157 (3S1):S63–S64. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Malbul K, Katwal S, Maharjan S, Shrestha S, Dhital R and Rajbhandari AP: Appendicitis as a presentation of COVID-19: A case report. Ann Med Surg (Lond). 69(102719)2021.PubMed/NCBI View Article : Google Scholar | |
|
Iyengar K, Mabrouk A, Jain VK, Venkatesan A and Vaishya R: Learning opportunities from COVID-19 and future effects on health care system. Diabetes Metab Syndr. 14:943–946. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Hansson J, Körner U, Khorram-Manesh A, Solberg A and Lundholm K: Randomized clinical trial of antibiotic therapy versus appendicectomy as primary treatment of acute appendicitis in unselected patients. Br J Surg. 96:473–481. 2009.PubMed/NCBI View Article : Google Scholar | |
|
Hansson J, Körner U, Ludwigs K, Johnsson E, Jönsson C and Lundholm K: Antibiotics as first-line therapy for acute appendicitis: Evidence for a change in clinical practice. World J Surg. 36:2028–2036. 2012.PubMed/NCBI View Article : Google Scholar | |
|
Suwanwongse K and Shabarek N: Successful conservative management of acute appendicitis in a coronavirus disease 2019 (COVID-19) Patient. Cureus. 12(e7834)2020.PubMed/NCBI View Article : Google Scholar | |
|
Vudayagiri L and Gusz J: COVID-19 positive in nasopharyngeal swab but negative in peritoneal fluid: Case report of perforated appendicitis. Cureus. 12(e9412)2020.PubMed/NCBI View Article : Google Scholar | |
|
Ahmad S, Ahmed RN, Jani P, Ullah M and Aboulgheit H: SARS-CoV-2 isolation from an appendix. J Surg Case Rep. 2020(rjaa245)2020.PubMed/NCBI View Article : Google Scholar | |
|
Romero-Velez G, Pereira X, Zenilman A and Camacho D: SARS-Cov-2 was not found in the peritoneal fluid of an asymptomatic patient undergoing laparoscopic appendectomy. Surg Laparosc Endosc Percutan Tech. 30:e43–e45. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Elbakouri A, El Azhary A, Bouali M, Bensardi F, Elhattabi K and Fadil A: Gastrointestinal manifestations related to infection with SARS-COV-2: Appendicular syndrome (A case report). Ann Med Surg (Lond). 65(102288)2021.PubMed/NCBI View Article : Google Scholar | |
|
Ngaserin SH, Koh FH, Ong BC and Chew MH: COVID-19 not detected in peritoneal fluid: A case of laparoscopic appendicectomy for acute appendicitis in a COVID-19-infected patient. Langenbecks Arch Surg. 405:353–355. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Kim IK, Kwag SJ, Kim HG, Ju YT, Lee SJ, Park TJ, Jeong SH, Jung EJ and Lee JK: Perioperative considerations for acute appendicitis in patients with coronavirus infection: Two cases report. Ann Coloproctol: Dec 7, 2021 (Epub ahead of print). | |
|
Sanders-Davis LJ and Ritchie J: Appendicitis with concurrent COVID-19 infection in a patient during the third trimester of pregnancy. BMJ Case Rep. 14(e242651)2021.PubMed/NCBI View Article : Google Scholar | |
|
Terpos E, Ntanasis-Stathopoulos I, Elalamy I, Kastritis E, Sergentanis TN, Politou M, Psaltopoulou T, Gerotziafas G and Dimopoulos MA: Hematological findings and complications of COVID-19. Am J Hematol. 95:834–847. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Han C, Duan C, Zhang S, Spiegel B, Shi H, Wang W, Zhang L, Lin R, Liu J, Ding Z and Hou X: Digestive Symptoms in COVID-19 patients with mild disease severity: Clinical presentation, stool viral RNA testing, and outcomes. Am J Gastroenterol. 115:916–923. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Wichmann D, Sperhake JP, Lütgehetmann M, Steurer S, Edler C, Heinemann A, Heinrich F, Mushumba H, Kniep I, Schröder AS, et al: Autopsy findings and venous thromboembolism in patients with COVID-19: A prospective cohort study. Ann Intern Med. 173:268–277. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Alroomi M, Rajan R, Omar AA, Alsaber A, Pan J, Fatemi M, Zhanna KD, Aboelhassan W, Almutairi F, Alotaibi N, et al: Ferritin level: A predictor of severity and mortality in hospitalized COVID-19 patients. Immun Inflamm Dis. 9:1648–1655. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Hindson J: COVID-19: Faecal-oral transmission? Nat Rev Gastroenterol Hepatol. 17(259)2020.PubMed/NCBI View Article : Google Scholar | |
|
Abdalhadi A, Alkhatib M, Mismar AY, Awouda W and Albarqouni L: Can COVID 19 present like appendicitis? IDCases. 21(e00860)2020.PubMed/NCBI View Article : Google Scholar | |
|
Brown MA: Imaging acute appendicitis. Semin Ultrasound CT MR. 29:293–307. 2008.PubMed/NCBI View Article : Google Scholar | |
|
Somers K, Abd Elwahab S, Raza MZ, O'Grady S, DeMarchi J, Butt A, Burke J, Robb W, Power C, McCawley N, et al: Impact of the COVID-19 pandemic on management and outcomes in acute appendicitis: Should these new practices be the norm? Surgeon. 19:e310–e317. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Vaghef Davari F and Sharifi A: Transmission possibility of COVID-19 via surgical smoke generated by the use of laparoscopic approaches: A subject of debate during the pandemic. J Laparoendosc Adv Surg Tech A. 31:1106–1113. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Cheruiyot I, Sehmi P, Ngure B, Misiani M, Karau P, Olabu B, Henry BM, Lippi G, Cirocchi R and Ogeng'o J: Laparoscopic surgery during the COVID-19 pandemic: Detection of SARS-COV-2 in abdominal tissues, fluids, and surgical smoke. Langenbecks Arch Surg. 406:1007–1014. 2021.PubMed/NCBI View Article : Google Scholar | |
|
Mowbray NG, Ansell J, Horwood J, Cornish J, Rizkallah P, Parker A, Wall P, Spinelli A and Torkington J: Safe management of surgical smoke in the age of COVID-19. Br J Surg. 107:1406–1413. 2020.PubMed/NCBI View Article : Google Scholar | |
|
COVIDSurg Collaborative: Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: An international cohort study. Lancet. 396:27–38. 2020.PubMed/NCBI View Article : Google Scholar | |
|
Liu D, Ahmet A, Ward L, Krishnamoorthy P, Mandelcorn ED, Leigh R, Brown JP, Cohen A and Kim H: A practical guide to the monitoring and management of the complications of systemic corticosteroid therapy. Allergy Asthma Clin Immunol. 9(30)2013.PubMed/NCBI View Article : Google Scholar | |
|
Sandy-Hodgetts K, Carville K and Leslie GD: Determining risk factors for surgical wound dehiscence: A literature review. Int Wound J. 12:265–275. 2015.PubMed/NCBI View Article : Google Scholar | |
|
Webster C, Neumayer L, Smout R, Horn S, Daley J, Henderson W and Khuri S: National Veterans Affairs Surgical Quality Improvement Program. Prognostic models of abdominal wound dehiscence after laparotomy. J Surg Res. 109:130–137. 2003.PubMed/NCBI View Article : Google Scholar |